

Libya officially the State of Libya, is a country in the Maghreb region in North Africa. It is bordered by the Mediterranean Sea to the north, Egypt to the east, Sudan to the southeast, Chad to the south, Niger to the southwest, Algeria to the west, and Tunisia to the northwest. Libya is made of three historical regions: Tripolitania, Fezzan, and Cyrenaica. With an area of almost 1.8 million km2 (700,000 sq mi), it is the fourth-largest country in Africa and the Arab world, and the 16th-largest in the world. Libya has the 10th-largest proven oil reserves in the world. The largest city and capital, Tripoli, is located in north-western Libya and contains over a million of Libya’s seven million people.
Libya is a member of the United Nations, the Non-Aligned Movement, the African Union, the Arab League, the OIC and OPEC. The country’s official religion is Islam, with 96.6% of the Libyan population being Sunni Muslims. The official language of Libya is Arabic. Vernacular Libyan Arabic is the most spoken, and the majority of Libya’s population is Arab.
In 2010, spending on healthcare accounted for 3.88% of the country’s GDP. In 2009, there were 18.71 physicians and 66.95 nurses per 10,000 inhabitants. The life expectancy at birth was 74.95 years in 2011, or 72.44 years for males and 77.59 years for females
Source: https://en.wikipedia.org/wiki/Libya
- GLOBAL PRETERM BIRTH RATES – LIBYA
- Estimated # of preterm births: 20.6%
- (USA 9.56-Global Average: 10.6)
Source: https://www.emro.who.int/child-adolescent-health/data-statistics/libya.html

COMMUNITY

Protecting Children From Wildfires And Smoke
According to Ready.gov, a wildfire is an unplanned fire that burns in areas such as a forest, grassland, or prairie. An increasing number of families live in areas prone to wildfires. The National Interagency Coordination Center has a Predictive Services Program that provides wildfire forecasts. It is important to note that a “Fire Weather Watch” means that dangerous fire weather conditions are possible over the next 12 to 72 hours. Extreme temperatures or tendencies toward hotter and drier climates (due to climate change), have led to increased wildfire activity and an intensifying of wildfires, all of which impact families and communities. Preparing in advance for potential wildfires can improve health outcomes and living situations for children and their families.
Protecting Children from Wildfires
Children are especially vulnerable to environmental hazards from wildfires. They eat more food, drink more liquids, and breathe more air than adults on a pound for pound basis. Children are in a critical period of development when toxic exposures can have profound negative effects and their exploratory behavior often places them in direct contact with materials that adults would avoid. (AAP policy: Ensuring the Health of Children in Disasters.)
Wildfires expose children to various environmental hazards (eg, fire, smoke, and the byproducts of combustion of wood, plastics, and other chemicals released from burning structures and furnishings). While wildfires are burning (acute phase), the major hazards to children are fire and smoke. In the aftermath of wildfires (recovery phase) children may be exposed to a different set of environmental hazards involving not only their homes, but also nearby structures, land, and recovery activities. The environment can include many potentially hazardous conditions and situations. Some of these are easy to see, such as broken glass and exposed electrical wires, and others are not visible, such as soil contaminated with hazardous materials like lead or persisting hot spots which can flare without warning.
Wildfires have the potential to cause short- and long-term effects on the psychological functioning, emotional adjustment, health, and developmental trajectory of children. (AAP clinical report: Providing Psychosocial Support to Children and Families in the Aftermath of Disasters and Crises).
Recommendations for Children and Masks
Wildfires can produce ashes, debris, or toxic chemicals in the air. These chemicals are especially challenging for children with asthma or other respiratory issues. This is similar to what happens when volcanic ash is in the environment after a volcano erupts. If the chemicals in the air make it not safe to breathe outdoors, public health officials might recommend that people stay indoors (in well-sealed and airconditioned facilities), limit trips outside, or briefly use masks or N95 respirators.
When Should Children Return to Areas Hit by Wildfires?
Children should be the last group to return to areas where there has been a natural disaster such as a wildfire. Key requirements for children to return to an area include restored drinking water and sewage removal, safe road conditions, removal of debris and damaged building materials, and structurally sound homes. Early education and child care facilities, schools, and outdoor play areas should be cleaned, cleared of hazards and made ready for use. Persisting hazards should be isolated and made inaccessible to children. Children, and whenever possible, teens, should only be permitted to return after affected areas have been cleaned up. Direct supervision of children by adults in these situations is important.
To address the health risks to children from wildfires, the Pediatric Environmental Health Specialty Units (PEHSU), with input from the AAP Council on Environmental Health, have developed the following fact sheets:
- Information on Health Risks of Wildfires for Children – Acute Phase – Guidance for Health Professionals
- Protecting Children from Wildfire Smoke and Ash
Contact your regional PEHSU to talk to an expert.
Free Online Couse – Wildfire Smoke and Your Patients’ Heath
The US Environmental Protection Agency (EPA) partnered with the Centers for Disease Control and Prevention (CDC) to develop an online course, Wildfire Smoke and Your Patients’ Heath. This course updates participants about the health effects associated with wildfire smoke and actions for people to take before and during a wildfire to reduce exposure. This course is intended for physicians, registered nurses, and others involved in clinical or health education. Continuing education credit is available.
Ahmad El Sherif – Baddi Tir [Music Video]
حمدالشريف – بديطير
Medical Uses of ChatGPT – The Medical Futurist

ChatGPT has been of the most popular topics on the internet for quite some time now. People usually use it to write articles, emails, or simply to gather ideas for projects. But is it possible to use it in a medical setting? Let’s see!

HEALTHCARE PARTNERS
Female leadership in neonatology: The value of mentorship
Posted on March 21, 2023 by Nancy Fliesler | Our Community, People
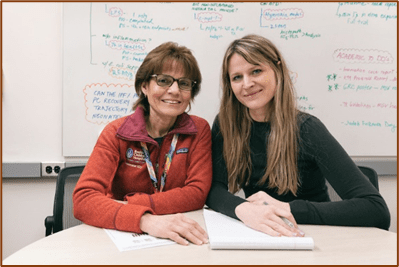
Martha Sola-Visner, MD, and Patricia Davenport, MD, enjoy a strong mentoring relationship where benefits flow in both directions.
While the majority of neonatologists are women, women make up a far smaller proportion of neonatologists in leadership positions. A recent national survey led by Kristen Leeman, MD, in the Division of Newborn Medicine at Boston Children’s and Lindsay Johnston, MD, at Yale, finds that many female neonatologists face roadblocks to career development. They often miss out on speaking engagements, career guidance, additional training, networking opportunities, and above all, mentors.
To learn more about their needs, Leeman and her colleagues contacted nearly 4,000 female neonatologists from the AAP-affiliated Women in Neonatology group and a Facebook group for female neonatologists. They received 451 survey responses, revealing several additional challenges:
- gender-based salary discrepancies, reported by 49 percent of respondents
- delayed promotion (37 percent)
- harassment by colleagues (31 percent), trainees (8 percent), staff (24 percent), and patient families (32 percent)
- lack of an established mentor (61 percent).
Female neonatologists also tend to struggle more than their male counterparts with work/life balance issues, Leeman notes, making it hard to advance. “Women commented on child care stress and burnout,” she says. “The supports are not there at vulnerable times in their careers. It’s a leaky pipeline.”
Building a mentoring program for female neonatologists
Leeman and Johnston decided to address what they see as the key missing ingredient — mentors.
“Both of us have had the benefit of superb mentorship, which has been integral to our careers,” says Leeman. “We wanted to offer an opportunity for all women across the U.S. to have access to female role models to help mentor them through different elements of their careers.”
With colleagues across the country, they created the National Women in Neonatology Mentorship Program. Bringing together senior, mid-career, and junior neonatologists, the year-long pilot program, which concludes in August, has three goals:
- to provide resources to facilitate career advancement and professional and personal satisfaction
- to identify strategies to help female neonatologists gain appropriate compensation, promotions, and professional recognition
- to foster a feeling of community.
In virtual and in-person meetings, the program’s 250-plus participants read and discuss materials, hear speakers, share their thoughts and experiences, network, offer mutual encouragement, and consult with mentors. The program has various subgroups, including groups for women practicing in community NICUs, groups for specific interests like global health or lab research, and groups for women from backgrounds that tend to be underrepresented in medicine.
Neonatology mentorship at Boston Children’s: Balancing medicine, research, and family
Patricia Davenport, MD, and Martha Sola-Visner, MD, neonatologists at Boston Children’s, illustrate the value of mentorship. As a junior faculty member, Davenport found herself juggling her clinical, research, and family responsibilities. In addition to caring for patients in the NICU, she joined Sola-Visner’s lab to conduct research on neonatal platelet transfusions. Sola-Visner quickly became a mentor.
“Martha’s mentorship has been crucial to me,” Davenport says. “She values her patients, her research, and her family. Holding those three things equally in your hands is really important. I had never done basic science before and needed a lot of mentoring, not just at the bench but also writing and presenting.”
Whether it’s an unfortunate patient outcome, an experiment that didn’t work, or a family emergency, Sola-Visner has been a vital support and sounding board. And the benefits of mentorship flow in both directions.
“I’m established now, and at this stage in my career, seeing other people progress and move forward is the most rewarding part of what I do,” says Sola-Visner. “Making sure that the people who I’ve mentored are succeeding becomes more and more important over time. I get great joy to see that.”
Davenport is also an enthusiastic participant in the national pilot mentorship program, where she is part of a subgroup on basic science.
“We talk about funding difficulties, how to organize a lab, wellness, how to care for yourself,” she says. “There’s a real sense of community across the nation. You’re always asking, ‘am I good enough?’ and it’s nice to hear other women having the same thoughts and feelings of ‘imposter syndrome.’ But we’re all doing good work.”
Source:https://answers.childrenshospital.org/mentorship-neonatology/

Preemies Are People, Too
Infant mental health should be paramount in the NICU.
Posted July 18, 2023 | Debra Brause, Psy.D

KEY POINTS
- Babies need touch and soothing to develop and thrive.
- Infant mental health deserves a critical place among the many needs of pre-term babies.
- The separation of parents and babies leads to poor outcomes on both sides.
“Your baby’s out. They’re resuscitating him now.” Those were the first words I heard while lying on the operating table, shivering from anesthesia, a glass tube next to me filling with blood. There was my son, a small, bluish thing, surrounded by frantic medical staff responding to the code blue.
That was the start of my son William’s life, named on that early morning in February for “strength.” William was rushed away to the Neonatal Intensive Care Unit for his first six weeks, and I can’t even remember how long it was before we could hold him. Visits were limited to one hour every three, and then, eventually, finally, through layers of tubes, my husband and I could make skin-to-skin contact with our baby.
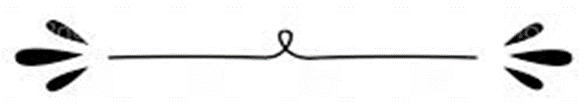
On one of those early, torturous days, when I had been sitting at the “bedside” of William’s incubator, I was struck by how bright, noisy, and chaotic the NICU felt. Beeping machines, nurses rushing to and fro, fluorescent lighting: It was a lot for my neurotypical sensory system to manage. And here were these fragile creatures, experiencing the assault of sensory overload.
I pulled the social worker aside, explaining how damaging this sensory tsunami was for these underdeveloped nervous systems and my worry for my brand-new tiny preemie. “He hasn’t even reached his due date yet,” she said. “So don’t worry. It’s like he’s not born yet.”
I was stunned. “But he’s right there. He’s taking all this in.”
I began to circulate articles. A former supervisor of mine in an infant mental health program directed me to the work of Harvard psychologist Heidelise Als, an innovator in the design and understanding of the developmental care of premature babies. I desperately distributed what I thought would be welcome insights. I was met with polite but dismissive nods.
Some of the nurses were wonderful. They suggested making audiotapes of us reading children’s stories that they would play for our son at bedtime. We still repeat the timeless rhymes of Sandra Boynton’s But Not the Hippopotamus, our only lifeline to our helpless little infant inside his glass box.
The saddest part was the babies who had no visitors. The attachment traumas unfolding before my eyes were unbearable to witness. Many parents don’t have the luxury of time away from work and other children, and, in the absence of any psychological education, the attachment needs of these babies were not being communicated from hospital to parent. Or met. Babies need skin-to-skin contact, a safe and reliable loving presence, and responsiveness to their emotional and physical needs.
That was 16 years ago. Has there been progress? We know that a NICU stay gravely impacts the mother’s mental health. Articles abound on maternal depression, PTSD, and attachment difficulties. The stress of the NICU experience can impact the parent’s capacity to connect to their baby.
But what about the babies? Kangaroo care involves holding a baby facing the parent with skin-to-skin contact. It is considered the standard of care, yet many barriers exist to its implementation. Volunteer “baby cuddler” programs have sprung up in hospitals across Canada and the U.S. Still, resources are often insufficient to fund enough volunteers to hold the babies who need them. In the meantime, these babies are subjected to painful separation from their caregivers and intrusive, distressing procedures, leading to higher rates of neurocognitive and psychosocial difficulties later in their development (Givrad et al., 2021).
As far as optimizing mental health outcomes, a baby’s relationship with their intimate caregivers is vital to their social and emotional development. Als created the evidence-based Newborn Individualized Developmental Care and Assessment Program (NIDCAP) back in 1984, and it is considered the “gold standard” of care. Part of Als’s contribution is understanding that long-term neurodevelopmental problems are prevented through a reflective stance that helps parents recognize, interpret, and respond to their baby’s communication. Holding the baby’s emotional world in mind lays the groundwork for a secure, trusting relationship that buffers against adverse mental health outcomes (Browne, 2020).
Unfortunately, a few obstacles complicate the utilization of the NIDCAP model. The primary obstacles are that the training is extensive, the model’s implementation requires coordination of the entire neonatal team, and institutional support is needed for its success (Klein et al., 2021).
I often wonder how much my son’s regulatory difficulties stem from this early stay in intensive care. He has never developed a regular sleep/wake cycle. He came home from the hospital with a feeding tube in his nose and with no ability to choose when and how much he ate; he has difficulty stopping what goes in his mouth today. Our early separation still makes it painful to part 16 years later.
The importance of mental health has taken hold in popular culture, giving voice to and bringing awareness to vulnerable and previously overlooked parts of society. I hope that, in the same way, we can begin to provide what is long overdue: a voice to the most fragile among us, our babies in the NICU.

Perspective-The Promise
Amy C. Blake, M.D.

The last promise I made was in 2013. As a first-year fellow in neonatology, I was well versed in the statistics on survival of preterm infants. When Wyatt was admitted to the neonatal intensive care unit (NICU), after being born at 31 weeks of gestation, I reassured his mother: more than 98% of infants who are born at 31 weeks survive,1 and the overwhelming majority grow into happy, healthy children. He was small — around the fifth percentile for his gestational age — but he arrived screaming with strong lungs and was doing well in his first few days.
As Wyatt closed in on 1 week of life, stable and tolerating feedings, his mother confessed her anxiety during one of our daily updates. “I’m worried,” she said. “I just want him to be OK.”
I again reassured her: 98% of babies like Wyatt survive, and most do well. “He’ll be OK,” I said. “I promise.” She took a breath and smiled. I left feeling proud of my communication skills and confident that Wyatt would continue to do well.
Two days later, I was called in from home to see another baby in the unit. “While you’re here,” one of the nurses said, “could you look at Wyatt? He’s been tachycardic, and something just seems off.”
At Wyatt’s bedside, it was clear that something was, indeed, very off. His heart rate was in the 200s — high even for a premature baby. His skin was mottled and his belly distended. When I opened his diaper, I found it full of blood.
An x-ray confirmed the diagnosis: pneumatosis intestinalis, a pattern of air within the bowel wall that’s pathognomonic for necrotizing enterocolitis. We called his parents to come in as we drew labs, increased his respiratory support, and started IV fluids. By the time they arrived 30 minutes later, we had intubated Wyatt, had placed an arterial line, and were starting dopamine to address his hypotension. A repeat x-ray only 3 hours after the onset of tachycardia showed extensive pneumoperitoneum: his intestine had perforated.
I shared this information with his family, and we prepared to transfer Wyatt to the nearby children’s hospital for surgery. As they left the unit, his mother gave me a hug. “Thank you for everything,” she said.
Two days later, despite maximal efforts, Wyatt died of fulminant necrotizing enterocolitis.
Some 7 years later, I was an attending neonatologist rounding in the NICU when I received a text message from my brother. It’s a boy, he announced. Born at term after an uncomplicated pregnancy, Nick was doing well, as was his mother.
Only a few hours later, my brother called back, concerned: Nick was having trouble breathing. They were taking him to the NICU.
The next 48 hours were a flurry of text messages and phone calls, as I tried to interpret blood gases and chest x-rays from 1500 miles away and to translate what the doctors were telling my brother into plain language. Nick was moved from CPAP to a ventilator, received surfactant, and initially had a good response. As his oxygen requirement crept back up to 40%, then 60%, I began to get uneasy. Did he have an infection? Pulmonary hypertension? Something less common?
The neonatologist taking care of Nick tried to reassure my brother, much as I had tried to reassure Wyatt’s family years before. “He’s doing OK,” she said. “His blood gas is getting better, and his oxygen needs are stable.”
My brother, hoping for answers and heavily coached by me, pressed her: Is this pneumonia? Does he need an oscillator? How about transport for ECMO? Could this be something more sinister, like one of the congenital disorders of surfactant production?
“It’s not surfactant protein B deficiency,” she said. “That’s the bad one, and Nick doesn’t have that. I promise.”
As Nick continued to get sicker, he was transferred to the level IV NICU across town. His oxygen requirements and ventilator support remained at near-maximal levels for days, and then weeks, as each intervention helped a little, and then didn’t: sedation, paralysis, inhaled nitric oxide, inotropic support. His dedicated team left no stone unturned.
Just after Nick reached 3 weeks of age, the genetics report came back: surfactant protein B deficiency, it read. Homozygous for a pathogenic mutation. My brother and his wife sat down with the team to discuss the findings, but we knew what it meant: fatal without a lung transplant.
Nick remained on support for several days more, as his older brother and grandparents were finally able to meet him. Then, when he was just under a month old, his parents withdrew support. Nick died peacefully in his mother’s arms.
As physicians, we are frequently given the gift of implicit trust by our patients and their families. Based on years of education and experience, our words matter. A broken promise, even when broken by factors out of our control, can result in not only disappointment but destruction of that trust.2 A recent study of parent–physician communication in the NICU pointed to providing hope as a key theme of good communication.3 But promising something that’s out of our control risks providing only false hope.
When I promised Wyatt’s mother that he would be OK, I fully believed that would be the case. With my limited experience at that point in my training, I didn’t yet understand how helpless all our knowledge, our medicines, our surgeries could be against such ruthless disease. I believe, too, that Nick’s first neonatologist truly believed that he couldn’t have such a rare, terrible disease and that she was doing her best to provide that much-needed hope.
Promises that are within our power to keep, on the other hand, can strengthen the bond between physicians and parents: promises to do our best, to care about their child, to remember the ones we couldn’t save.
Two years after Wyatt died, I saw his parents again. His mother had delivered another child, Bryson, this time at 34 weeks. He was admitted to our NICU, just down the hall from where his older brother had been. When their mother saw me, she gave me a hug. “Thank you for taking care of Wyatt,” she said.
I hugged her back, thinking carefully about my words. “I’ll take great care of Bryson,” I said. “And I’ll never forget Wyatt. I promise.”
Source:https://www.nejm.org/doi/full/10.1056/NEJMp2213824

An Invitation to Lunch
Eleanor R. Menzin, M.D.

When I joined my primary care pediatric practice 22 years ago, my senior partner frequently invited me to lunch, which he ate several times a week in the cafeteria of the children’s hospital across the street. Sometimes he ate with our office nurses, but often he ate with other physicians — surgeons or subspecialists whom he had met in his 30-plus years of practice, hospital work, and committee service. He frequently reminded me that these lunches were a critical way to make the professional connections every primary care doctor needs.
I never went to lunch. New to outpatient medicine, rounding daily at two or three hospitals, raising one small child (and then eventually two and three small children), I was in constant motion. I ate lunch in my car, racing from toddler music class to an afternoon session, or had it walking from the hospital to the office.
In part, I never went to lunch because of the competing demands on my time. I also avoided the invitations because, although I knew my partner would welcome me, I was also sure I would not fit in at the lunch table filled with men 30 years my senior. I viewed those lunches (and even more so, my older partners’ tales of the defunct Doctors’ Dining Room) the way I viewed my father’s stories of playing stickball in the streets of Brooklyn. I felt a faint nostalgia for a time I had never experienced — when social connections were spontaneous and time was elastic. But I did not want to put myself in that situation any more than I wanted to play stickball.
Yet it quickly became clear that a network of subspecialists and surgical colleagues was fundamental to my practice. Most of primary care is common illnesses, personal relationships, and evidence-based care algorithms. Most, but not all. Recognizing the unusual, knowing when you are the wrong clinician, and being able to access the correct specialist make the difference between good primary care and great primary care.
I set out to build my network without lunches. Luckily, I stayed at the same institution where I had trained. My residency class and the surrounding classes furnished me with three cardiologists, two neurologists, an allergist, an oncologist, and more emergency medicine and neonatologists than I could count. I met some doctors through patients with complex conditions, such as the otorhinolaryngology fellow with whom I shared a patient who had been born prematurely and needed airway reconstruction. Some doctors I met when I cared for their children; others I met when they operated on mine.
Those institutional contacts were the roots of my network, but the network grew through email. I read each subspecialist’s letter carefully. When I found a doctor whose plan was logical and who was liked by my patients, I carefully noted the name. The next time I had a question, I emailed and introduced myself. The physicians who answered quickly and thoughtfully became part of my inner circle. Gradually, I built a specialized list of my people: knees, hands, celiac disease, seizures, and arrhythmia.
These relationships, which are foundational to my practice, are hard to categorize. Last month, I emailed an orthopedist to help a friend’s child find a knee specialist 600 miles away. Before the appointment, my friend asked me if the person who had made the connection was a colleague or a friend. I thought for several minutes before admitting that I was not sure. I have known this doctor for years, we have exchanged cell phone numbers, and he has called an anxious family for me on a Sunday evening. And yet I wonder whether we would recognize each other in an elevator.
My husband sometimes points out that my gain from these relationships is clear but questions what the specialists gain. (Full disclosure: he asked this question after I backed into the car of an often-emailed spine surgeon in the parking garage.) I try to send my patients neatly packaged: patients with growth delay arrive with lab results, bone age, and growth charts so the endocrinologist can do the visit with minimal follow-up. I hope that I send mostly patients with complex and interesting conditions — that I weed out the unnecessary consults. For those who depend on a steady stream of new patients, I provide a steady stream of referrals. For those whose practices are overflowing, I send questions instead, since answering me is faster than seeing another patient.
For me, and I hope for my specialist friends, this relationship is more than just transactional. I went into medicine, and stayed in academic medicine, because I find it endlessly fascinating — a pleasure to learn and teach. Interactions with specialists are a welcome respite from the monotony of ear infections and an opportunity to learn. In addition, these interactions lighten the burden of practicing. Being an attending is, in many ways, a very lonely job. There is an unremitting stream of decisions to be made, and that responsibility is isolating. Discussions, by email or over lunch, of difficult cases ameliorate that loneliness. I am profoundly grateful for the doctors who answer my emails, look at my films, and squeeze in my patients. Shared wisdom and joint decision making in these exchanges bring intellectual stimulation and reassurance, increased joy, and decreased anxiety.
My institution, like many, is moving to e-consults. Soon, I will put a request into Epic rather than email a friend. This shift should increase equity and access for all primary care providers and their patients. As someone who answers many unreimbursed phone calls, I am keenly aware of the burden my emails put on specialists. I see all the ways that this system will improve care, but I also see the potential losses: personal relationships, building trust, choosing the patient’s team.
After 25 years, I am not worried about my network or community. I am worried about how new doctors will find opportunities for learning, collegiality, support, and friendship in the larger community of medicine. As burnout rates skyrocket in primary care, creating this scaffolding for young physicians is crucial.
Good advice has no statute of limitations; it is time to go to lunch. This fall, a new doctor will join our group after completing residency hundreds of miles away. When we meet weekly to run cases and answer questions, it will be in the hospital cafeteria. I will send out an email announcing her arrival to my network of friends and colleagues; it will include an open invitation to join us for lunch on Tuesdays at 12:15, starting in October. I hope to see you there.
Source:https://www.nejm.org/doi/full/10.1056/NEJMp2303125

PREEMIE FAMILY PARTNERS

Supporting Parents of Preemies
Mediclinic Southern Africa – Nov 18, 2016
Celeste Rushby has three children who were born prematurely. The experience inspired her to start a support group for moms of preemies. This is her story.
4 Things You Can Do When You’re Not Allowed to Hold Your NICU Baby
If you are a parent with a baby in the neonatal intensive care unit (NICU) and you haven’t been able to hold your baby…OR you’re going through a season of life in the NICU where your baby can’t be held—I want you to know there are ways you can be there for your precious one. Here are 4 ways you can be involved that support your baby’s short- and long-term developmental outcomes, even when they can’t be held.
I’ve been thinking a lot about NICU parents who aren’t allowed to hold their baby. I can see the eyes of moms aching, yet terrified. It’s one of the hardest parts about being in the NICU…waiting.
The NICU is a rollercoaster (as I’m sure everyone who’s experienced it can attest!) and things can change in the blink of an eye. There are many situations and circumstances that can prolong the time until babies in the NICU can be held.
The chance to hold may be delayed due to your baby’s
- prematurity
- unstable medical status
- medical lines
- surgical precautions, and/or
- breathing requirements.
The feeling of helplessness is heavy in the heart of every NICU parent. I want to provide you with something you CAN DO!
Here are 4 things you can do with your NICU baby when you aren’t able to hold them. Things that will boost your confidence AND their development.
1. GIVE A HAND HUG
Hand hugs can be a precious gift to NICU parents (and medical caregivers). It offers a way for you to provide your baby with some skin-to-skin touch and comforting input when they’re unable to be held.
A hand hug is when you place one hand on your baby’s head and the other hand is either
- cupping your baby’s feet OR
- placed over their arms/tummy while your baby is supported in a flexed (tucked) position.
You can also place a hand over your baby’s trunk (midsection) and cup the feet as another option.
There are several variations of a hand hug. If you’re wondering how you can adapt it for use with your baby, I did an entire post dedicated to hand hugs in the NICU here!
ONE THING I TEACH EVERY NICU PARENT TO DO WITH THEIR BABY—A HAND HUG!
I have heard parents say so many times, “He doesn’t like to be touched” or “She’s a touch-me-not”.
When you place your hands on your baby in a developmentally-supportive and nurturing way, you are shaping your baby’s brain.
You are…
- building positive sensory pathways
- supporting sensory processing skills
- promoting medical stability, and
- improving their tolerance to TOUCH!
Plus, lots more!
Because of your hand hugs, your baby will develop better tolerance to diaper changes, blood pressure checks, repositioning, transfers for holding, and interaction.
Always be responsive to your baby’s cues during a hand hug. Learning when your baby is showing you stress cues or happy, approach cues is important so you can help them develop strong coping skills.
If you can’t provide a hand hug, let your sweet one hold onto your finger. Even if they aren’t grasping yet, place your finger in their hand so they can experience your scent and comforting touch.
2. OBSERVE YOUR BABY’S MOVEMENTS
Now this one can be difficult because of the trauma that often comes with the NICU environment. Observing your baby may be really difficult for one mom, but may be the emotional release another mom needs. If it’s too triggering to stand at your NICU baby’s bedside and observe all their little movements and noises, that’s OK.
Take a step back and come back to the bedside when you feel like you’re ready.
No matter how early your baby was born, or how sick they are—you can always observe them.
EVERY SINGLE BABY in the NICU is different.
Each baby is unique and special. Each with their own communication style, special movements, and individual behaviors that make up who they are and what their NICU journey will be like!
This is a special time to get to know your baby.
You don’t have to be hands-on all the time in order to be a good NICU parent or show attention to your child.
Let me say that again…”you don’t have to be hands-on all the time in order to be a good parent!”.
In fact, in the NICU, there are times when it is more supportive to your baby when we’re hands off and prioritize our touch and interactions to certain times.
When it’s “hands-off time”, you can always OBSERVE!
Gazing at your baby through their isolette and studying the way their toes wiggle, their face twitches, or their little hands move, can help ground you in the moment and help you as you transition to the role of “mom” or “dad”.
That’s your baby.
I want to encourage you to observe your baby, but I also encourage caution and awareness as you peek into your baby’s isolette.
When observing any baby in the NICU, it’s important to be aware of their sensory environment.
The sensory environment relates to all of the touch, smells, sounds, movement, tastes, and interactions occurring in your baby’s surroundings. Such as:
- medical equipment beeping
- lights on overhead
- the medical team talking
- mom’s voice
- the smell of hand sanitizer
- being contained with a positioning device
- feeling their arms and legs move in space
- reflux or belly distress
Here’s a trick: if your baby has a cover over their isolette and/or is in a stage of development where their eyes need to be protected from direct light (babies younger than 35 weeks), open the isolette cover near the end of your baby’s bed. That way, you can observe without disrupting their environment or sleep.
I don’t want your baby to be overstimulated by their environment when we move their isolette cover and allow light into their healing space.
Let me know how your observations go! What sweet things does your baby do?
3. READ TO YOUR BABY
Yep, that’s right. You can read to your baby while they’re growing in the NICU. The beautiful thing about this, is that reading slowly and quietly at their bedside supports language, socio-emotional, and cognitive development.
You are providing your baby with positive listening experiences that help regulate their medical status and teach them to process the world around them .
Parents have told me they feel silly doing this. It can feel strange at first. Especially when you are in an open bay NICU environment, meaning there are multiple bed spaces next to each other instead of private rooms.
Mom…Dad…nothing is silly if it supports the development and medical stability of your baby.
The isolette walls will muffle your voice similar to the womb. There’s no need to open the port holes of the incubator, your voice will carry to your baby in a developmentally-supportive way.
What if your NICU doesn’t let you bring items (like books!) into the unit? Don’t let that stop you! Go ahead and…
- make a story up,
- tell your baby a story about somewhere you’ve been,
- tell a popular story from memory,
- read a children’s story/nursery rhyme from your phone.
There’s an entire organization that focuses on supporting parents by encouraging reading in the NICU. It’s called NICU Book Club. Check them out on Facebook to hear from other NICU families who are reading to their babies or donate in support of their mission.
Here are a couple of testimonials they share on their page.
**Testimonials copied from the NICU book club Facebook page.
- “Reading to my daughter gives me relief, especially when she reacts to my voice. It strengthens our bond and brings us even closer. Not to mention the benefits she receives with brain development. It’s a tradition I plan on continuing outside of the NICU. Thank you for the opportunity and new routine!! “
- “We would read books with him every day. Doctor Seuss was our favorite. His sats were always perfect while we cuddled and read together. It added some normalcy to our days in the NICU. For that moment, it was just me reading my favorite stories to my son.”
YOU’RE NOT ALONE.
Parents are reading to their NICU babies around the world. Your sweet baby is thankful knowing you are there.
4. PARTICIPATE IN THEIR CARE
Even if you’re not able to get your baby out to hold them, you can still participate in their care.
Your baby will still need their diaper changed, their temperature taken, baths, and oral care.
Ask questions and get hands-on, so you can learn how to do some of these tasks. Your baby’s bedside nurse is happy to help you learn to parent in a new way.
If you are a parent with a baby in the neonatal intensive care unit (NICU) and you haven’t been able to hold your baby…OR you’re going through a season of life in the NICU where your baby can’t be held—I want you to know there are ways you can be there for your precious one. Here are 4 ways you can be involved that support your baby’s short- and long-term developmental outcomes, even when they can’t be held.
I’ve been thinking a lot about NICU parents who aren’t allowed to hold their baby. I can see the eyes of moms aching, yet terrified. It’s one of the hardest parts about being in the NICU…waiting.
The NICU is a rollercoaster (as I’m sure everyone who’s experienced it can attest!) and things can change in the blink of an eye. There are many situations and circumstances that can prolong the time until babies in the NICU can be held.
The chance to hold may be delayed due to your baby’s
- prematurity
- unstable medical status
- medical lines
- surgical precautions, and/or
- breathing requirements.
The feeling of helplessness is heavy in the heart of every NICU parent. I want to provide you with something you CAN DO!
Here are 4 things you can do with your NICU baby when you aren’t able to hold them. Things that will boost your confidence AND their development.
1. GIVE A HAND HUG
Hand hugs can be a precious gift to NICU parents (and medical caregivers). It offers a way for you to provide your baby with some skin-to-skin touch and comforting input when they’re unable to be held.
A hand hug is when you place one hand on your baby’s head and the other hand is either
- cupping your baby’s feet OR
- placed over their arms/tummy while your baby is supported in a flexed (tucked) position.
You can also place a hand over your baby’s trunk (midsection) and cup the feet as another option.
There are several variations of a hand hug. If you’re wondering how you can adapt it for use with your baby, I did an entire post dedicated to hand hugs in the NICU here!
ONE THING I TEACH EVERY NICU PARENT TO DO WITH THEIR BABY—A HAND HUG!
I have heard parents say so many times, “He doesn’t like to be touched” or “She’s a touch-me-not”.
When you place your hands on your baby in a developmentally-supportive and nurturing way, you are shaping your baby’s brain.
You are…
- building positive sensory pathways
- supporting sensory processing skills
- promoting medical stability, and
- improving their tolerance to TOUCH!
Plus, lots more!
Because of your hand hugs, your baby will develop better tolerance to diaper changes, blood pressure checks, repositioning, transfers for holding, and interaction.
Always be responsive to your baby’s cues during a hand hug. Learning when your baby is showing you stress cues or happy, approach cues is important so you can help them develop strong coping skills.
If you can’t provide a hand hug, let your sweet one hold onto your finger. Even if they aren’t grasping yet, place your finger in their hand so they can experience your scent and comforting touch.
2. OBSERVE YOUR BABY’S MOVEMENTS
Now this one can be difficult because of the trauma that often comes with the NICU environment. Observing your baby may be really difficult for one mom, but may be the emotional release another mom needs. If it’s too triggering to stand at your NICU baby’s bedside and observe all their little movements and noises, that’s OK. Take a step back and come back to the bedside when you feel like you’re ready.
No matter how early your baby was born, or how sick they are—you can always observe them.
EVERY SINGLE BABY in the NICU is different.
Each baby is unique and special. Each with their own communication style, special movements, and individual behaviors that make up who they are and what their NICU journey will be like!
This is a special time to get to know your baby.
You don’t have to be hands-on all the time in order to be a good NICU parent or show attention to your child.
Let me say that again…”you don’t have to be hands-on all the time in order to be a good parent!”.
In fact, in the NICU, there are times when it is more supportive to your baby when we’re hands off and prioritize our touch and interactions to certain times.
When it’s “hands-off time”, you can always OBSERVE!
Gazing at your baby through their isolette and studying the way their toes wiggle, their face twitches, or their little hands move, can help ground you in the moment and help you as you transition to the role of “mom” or “dad”.
That’s your baby.
I want to encourage you to observe your baby, but I also encourage caution and awareness as you peek into your baby’s isolette.
When observing any baby in the NICU, it’s important to be aware of their sensory environment.
The sensory environment relates to all of the touch, smells, sounds, movement, tastes, and interactions occurring in your baby’s surroundings. Such as:
- medical equipment beeping
- lights on overhead
- the medical team talking
- mom’s voice
- the smell of hand sanitizer
- being contained with a positioning device
- feeling their arms and legs move in space
- reflux or belly distress
Here’s a trick: if your baby has a cover over their isolette and/or is in a stage of development where their eyes need to be protected from direct light (babies younger than 35 weeks), open the isolette cover near the end of your baby’s bed. That way, you can observe without disrupting their environment or sleep.
I don’t want your baby to be overstimulated by their environment when we move their isolette cover and allow light into their healing space.
Let me know how your observations go! What sweet things does your baby do?
3. READ TO YOUR BABY
Yep, that’s right. You can read to your baby while they’re growing in the NICU. The beautiful thing about this, is that reading slowly and quietly at their bedside supports language, socio-emotional, and cognitive development.
You are providing your baby with positive listening experiences that help regulate their medical status and teach them to process the world around them.
Parents have told me they feel silly doing this. It can feel strange at first. Especially when you are in an open bay NICU environment, meaning there are multiple bed spaces next to each other instead of private rooms.
Mom…Dad…nothing is silly if it supports the development and medical stability of your baby.
Even if your baby is in an isolette, you can sit next to it and read quietly.
The isolette walls will muffle your voice similar to the womb. There’s no need to open the port holes of the incubator, your voice will carry to your baby in a developmentally-supportive way.
What if your NICU doesn’t let you bring items (like books!) into the unit? Don’t let that stop you! Go ahead and…
- make a story up,
- tell your baby a story about somewhere you’ve been,
- tell a popular story from memory,
- read a children’s story/nursery rhyme from your phone.
There’s an entire organization that focuses on supporting parents by encouraging reading in the NICU. It’s called NICU Book Club. Check them out on Facebook to hear from other NICU families who are reading to their babies or donate in support of their mission.
Here are a couple of testimonials they share on their page.
**Testimonials copied from the NICU book club Facebook page.
- “Reading to my daughter gives me relief, especially when she reacts to my voice. It strengthens our bond and brings us even closer. Not to mention the benefits she receives with brain development. It’s a tradition I plan on continuing outside of the NICU. Thank you for the opportunity and new routine!! “
- “We would read books with him every day. Doctor Seuss was our favorite. His sats were always perfect while we cuddled and read together. It added some normalcy to our days in the NICU. For that moment, it was just me reading my favorite stories to my son.”
YOU’RE NOT ALONE.
Parents are reading to their NICU babies around the world. Your sweet baby is thankful knowing you are there.
4. PARTICIPATE IN THEIR CARE
Even if you’re not able to get your baby out to hold them, you can still participate in their care.
Your baby will still need their diaper changed, their temperature taken, baths, and oral care.
Ask questions and get hands-on, so you can learn how to do some of these tasks. Your baby’s bedside nurse is happy to help you learn to parent in a new way.
I know you weren’t planning on changing a diaper the size of a credit card…I have some tips to make it easier.
And always remember, your baby wants you to do her care…even when it’s terrifying.
She wants to smell your scent as you open the doors of the isolette.
She wants to feel the touch of your skin on hers as you give her a hand hug before you start her care.
She wants to hear the soft whisper of your voice as you say, “Hi sweet one! It’s time for a diaper change. I’m so proud of you.”
There are so many reasons your baby wants you to be involved.
You are…
- building attachment,
- shifting into the role of mom and dad,
- gaining confidence,
- learning about your baby, and
- creating positive brain pathways.
If you’re in a season where you can’t hold your baby, I truly hope that day is near.
Until then, know that your presence and involvement in your baby’s care at this stage in their journey is INCREDIBLY important for your sweet baby’s overall development and long-term growth.
I hope you can try some of these things today.
I’m prayerful that the day you can hold your baby is near!
Is there anything special you do (or did!) when your baby can’t be held?
What has helped you bond with your baby?
I’m proud of you.

INNOVATIONS

Bloodstream infections in preemies may originate from their gut microbiomes
by Jacquelyn Kauffman May 3, 2023

Dangerous bacterial bloodstream infections in preemies may originate from the infants’ gut microbiomes, according to researchers at Washington University School of Medicine in St. Louis. Such infections are of substantial concern, as about half of infants who are extremely preterm or have very low birth weights experience at least one episode of the life-threatening infection after 72 hours of life.
The findings are published May 3 in the journal Science Translational Medicine.
Preterm infants are at high risk of infections due to underdeveloped organs, coupled with considerable antimicrobial exposure. Until recently, virtually every prematurely born baby was treated with antibiotics as a preventive measure. While the antibiotics are intended to target disease-causing pathogens, this treatment also can lead to disruption of the gut microbiome in a way that could allow virulent strains of antibiotic-resistant bacteria to increase in numbers.
“This is a vulnerable population,” said senior author Gautam Dantas, PhD, the Conan Professor of Laboratory and Genomic Medicine and a professor of pathology & immunology. “This is also a time when the composition of the gut microbiome is first developing. These early exposures to bacteria shape the gut microbiome in ways that will probably stay with these babies for the rest of their lives. We also have studied the gut microbiomes of infants born at full term, and we know that such babies do not have as many problems, but it’s clear that the type of bugs that colonize the gut in the first few months to three years of life will determine what the microbiome looks like later on. Our study also suggests that an early look at the gut microbiome in preemies may allow us to identify those at high risk of dangerous bloodstream infections.”
After birth, a baby’s microbiome develops by acquiring microbes from the environment and the infant’s primary caregivers. Such microbes help in a multitude of functions, including digestion and absorption of nutrients. In addition, in a more diverse gut microbiome, beneficial microbes outcompete disease-causing microbes, thereby protecting the infant from disease. In some instances, antibiotics can kill beneficial microbes, giving more dangerous and potentially antibiotic-resistant strains the opportunity to multiply and cause disease.
The most common bacteria in bloodstream infections are also commonly found to colonize the gut without initially causing disease. The researchers, including first author Drew J. Schwartz, MD, PhD, an assistant professor of pediatrics and an infectious diseases physician, aimed to test whether such bloodstream infections come from inside the gut or from external transmission. The study included newborns admitted to the neonatal intensive care units (NICU) at St. Louis Children’s Hospital, Children’s Hospital at Oklahoma University Medical Center and Norton Children’s Hospital in Louisville, Ky.
The researchers performed whole genome sequencing on the bacterial strain causing the bloodstream infection and used computational profiling to precisely track the identical strain within feces to identify the strains of bacteria that had colonized the infants’ guts prior to bloodstream infection.
In 58% of these cases, the researchers found the gut-origin hypothesis to be true: They found a nearly identical disease-causing bacterial strain in the guts right before a bloodstream infection was diagnosed. In about 79% of cases, they found the disease-causing strain in the gut after a bloodstream infection was diagnosed.
The data also demonstrated that some of the strains of bacteria that caused bloodstream infections were shared among infants within the NICU. This indicates that even in controlled environments, there still could be microbes exchanged between infants, shared by hospital staff or transferred from NICU surfaces. However, relative to other newborns in the NICU who did not experience bloodstream infections, those who did had dramatically more of the causative species in their guts in the two weeks prior to bloodstream infection.
Moving forward, Dantas said, responsible antibiotic use is key, meaning they should only be given to infants who have confirmed bacterial infections. The study suggests that it may be possible to develop a risk assessment tool to help physicians quantify the risk of future bloodstream infections by identifying whether disease-causing bacteria already have colonized an infant’s gut and to what degree, a focus of Schwartz’s independent research laboratory at Washington University. Ongoing studies could add additional microbiome data over time to show which infants received antimicrobials and what their impact was on potential pathogens lurking in the gut microbiome. This potentially could empower physicians to perform rapid microbiome sequencing to determine best treatment strategies.
“From this study, as well as in our lab’s past studies, it’s clear that we need to be better stewards of how antimicrobials are given,” Dantas said. “Antimicrobials are critical; we are going to need them to treat infections, but we need to carefully weigh whether and when to use antimicrobials in specific situations. We need to make sure that when those antimicrobials are given, we have a very good reason.”
An Interview with Chat Generative Pre-Training Transformer (Chat GPT): How Can Artificial Intelligence (AI) Change our Practice?
Munaf Kadri, MD, Shaina Lodhi, MD, Farha Vora, MD, Mitchell Goldstein, MD, MBA, CML, Hun-Seng Chao, MD

For the past several years, Chat GPT has been increasing in popularity. The abuses of AI to generate answers to college essays have been widely reported in the news, especially when these essays are flawed with imperfect information. Indeed, there are even programs that detect the use of AI when the authorship is suspect. Others extol its virtue in creating new answers to perplexing questions. However, is there a role for AI in the practice of Neonatology? We decided to interview OpenAI’s Chat GPT ( https://openai.com/about) to see if Chat GPT could find a useful place in our practices.
Chat-GPT, who are you and when did you come into being?
I am ChatGPT, a language model developed by OpenAI. I came into being as a part of the GPT-3.5 model, which is based on the GPT-3 architecture. My training data goes up until September 2021, and I was released in June 2020. My purpose is to assist users in generating human-like text based on the prompts and questions I receive. How can I assist you today?
Should I rely on questions that I ask you to make medical decisions about the clinical care of neonates?
No, you should not rely on the questions you ask me, ChatGPT, to make medical decisions about the clinical care of neonates or any other individuals. While I strive to provide accurate and helpful information, I am an AI language model and my responses should not be considered medical advice.
When it comes to medical decisions, especially for the care of neonates, it is crucial to consult with qualified healthcare professionals such as doctors, pediatricians, or neonatologists. They have the necessary expertise, knowledge, and access to specific medical information to provide appropriate and personalized advice based on your specific situation.
If you have any concerns or questions regarding the clinical care of neonates, it is always best to consult a healthcare professional who can provide you with reliable and accurate information based on their clinical experience and the latest medical guidelines.
Can you reliably search research manuscripts in the field of Neonatology?
As an AI language model, I don’t have direct access to my training data or the ability to browse the internet. I cannot search research manuscripts or access specific sources such as subscription based databases, proprietary journals, or paywalled articles.
However, I have been trained on a diverse range of data, including books, websites, and scientific literature, up until September 2021. So, I can provide general information and answer questions to the best of my knowledge based on the training I have received. If you have specific questions about neonatology, I’ll do my best to assist you based on the information available to me. Remember to consult primary and peer-reviewed sources, as well as healthcare professionals, for specialized and up-to-date medical information.
Can I do things to make your responses better for me and others who might ask questions?
Absolutely! There are several things you can do to help improve the quality of responses and make the most out of your interactions with me and other users. Here are a few suggestions:
Be clear and specific: Providing clear and specific questions or prompts can help me understand what you’re looking for and provide more relevant and accurate responses.
Ask for clarification if needed: If a response is unclear or you require more information, feel free to ask for clarification. I’ll do my best to provide further details or elaborate on a particular topic.
Provide context: If your question or prompt relates to a specific situation or context, providing relevant details can help me generate more tailored and useful responses.
Fact-check and consult multiple sources: While I strive to provide accurate information, it’s always a good practice to fact-check the information and consult multiple reliable sources. This can help ensure the information is up-to-date and accurate.
Keep conversations appropriate and respectful: Maintaining a respectful and appropriate conversation helps create a positive and productive environment for everyone. Avoid sharing personal or sensitive information during the conversation.
Remember that while I can provide general information and suggestions, it’s important to consult professionals or trusted sources for specific or critical matters, such as medical advice or legal issues.
By following these guidelines, you can help improve the overall experience and obtain more valuable responses.
Are you able to suggest ways that a neonatologist can practice neonatology better?
As an AI language model, I can certainly offer some general suggestions that may help neonatologists enhance their practice. However, please note that these suggestions are not meant to replace professional experience or personalized advice. Neonatology is a specialized medical field, and specific recommendations may vary depending on individual circumstances and patient needs. Here are a few general ideas:
1. Continual education: Staying up-to-date with the latest advancements, research, and guidelines in neonatology is essential. Participate in conferences, workshops, and online courses, and engage in self-directed learning to expand knowledge and skills.
2. Collaboration and networking: Foster collaborations with other neonatologists, pediatricians, and interdisciplinary teams. Engage in professional networks and communities to exchange knowledge, share experiences, and stay connected with the broader neonatology community.
3. Patient-centered care: Focus on providing holistic and patient-centered care. Consider the physical, emotional, and developmental needs of neonates and their families. Involve parents in the decision-making process and provide clear and compassionate communication.
4. Research and evidence-based practice: Contribute to the field of neonatology through research, clinical trials, or quality improvement projects. Strive to incorporate evidence based practices into clinical care and critically evaluate new interventions or technologies.
5. Teamwork and communication: Effective teamwork and communication are crucial in neonatology. Foster a supportive and collaborative environment among colleagues, nurses, respiratory therapists, and other healthcare professionals to ensure optimal patient outcomes.
6. Continuous quality improvement: Regularly evaluate clinical practices, outcomes, and protocols. Engage in quality improvement initiatives to enhance patient safety, reduce errors, and optimize care processes.
7. Embrace technology: Stay informed about advancements in neonatal technology and utilize appropriate tools and systems to improve patient monitoring, data management, and treatment options.
Remember, these are general suggestions, and neonatology is a complex field that requires specialized expertise. It’s always important for neonatologists to rely on their own clinical judgment, consult with colleagues, and adhere to professional guidelines and best practices.
What’s the best time to do skin to skin with mothers after birth of a preterm baby?
Skin-to-skin contact, also known as kangaroo care, is beneficial for both preterm babies and their mothers. It helps promote bonding, regulate the baby’s body temperature, stabilize heart rate and breathing, and support breastfeeding initiation. The timing of skin to-skin care may vary depending on the baby’s condition and the practices of the specific neonatal unit. Here are some general guidelines:
Immediate skin-to-skin contact: In many cases, immediate skin to-skin contact is encouraged, as long as the baby is medically stable. This can occur as soon as the baby is born, after a quick assessment and necessary medical interventions.
Adaptation to the neonatal unit: In some cases, particularly when the baby requires immediate medical attention or stabilization, skin-to-skin care may be initiated once the baby is stable and has been transferred to the neonatal unit.
Gradual progression: If immediate skin-to-skin contact is not possible due to the baby’s medical condition, the healthcare team may guide parents on gradually increasing the duration and frequency of skin-to-skin care as the baby’s condition improves.
It’s important to note that individual circumstances may influence the timing of skin-to-skin care. The healthcare team, including neonatologists, nurses, and other specialists, will assess the baby’s medical stability and guide parents on the appropriate timing and duration of skin-to-skin contact.
Additionally, it’s recommended that parents consult with the neonatal care team to understand the specific protocols and guidelines of the neonatal unit where their preterm baby is being cared for. They will be able to provide tailored recommendations based on the baby’s condition and individual needs.
When is the best time to close a patent ductus arteriosus?
1. Symptomatic PDAs: If a PDA is causing significant symptoms such as respiratory distress, poor feeding, or heart failure, intervention to close the PDA may be considered earlier. The specific timing will depend on the baby’s condition and the judgment of the healthcare team.
2. Hemodynamically significant PDAs: A PDA that is causing significant hemodynamic instability, such as persistent pulmonary hypertension or compromised systemic blood flow, may require earlier intervention.
3. Conservative management: In some cases, a “watchful waiting” approach may be adopted, especially if the PDA is small, asymptomatic, and the baby is clinically stable. The PDA may spontaneously close over time without intervention.
4. Timing and method of closure: When intervention is deemed necessary, the specific timing and method of closure can vary. Different strategies include medical therapy with cyclooxygenase inhibitors (such as indomethacin or ibuprofen), surgical ligation, or transcatheter interventions. The choice of method depends on various factors, including the baby’s gestational age, size, clinical condition, and the expertise available at the healthcare facility.
It’s important to note that the decision to close a PDA requires careful assessment by a neonatologist or a pediatric cardiologist who will evaluate the individual baby’s condition and make an informed decision based on the available evidence, guidelines, and their clinical expertise.
Parents should consult with the healthcare team caring for their baby to understand the specific considerations and treatment plan for their baby’s PDA.
What is the best humidity for a preterm patient in an isolette?
Maintaining appropriate humidity levels in the environment of a preterm patient, such as an incubator or isolette, is important for their well-being and respiratory comfort. The optimal humidity range can vary depending on the gestational age, overall health, and individual needs of the baby. However, the general guideline for humidity in the isolette is around 40-60%. Here are some considerations:
1. Gestational age: The humidity requirements may vary based on the baby’s gestational age. Extremely preterm infants may benefit from higher humidity levels initially, as they have more delicate and immature skin, higher transepidermal water loss, and increased risk of dehydration.
2. Respiratory status: Infants with respiratory issues, such as respiratory distress syndrome, may benefit from slightly higher humidity levels to help reduce airway dryness and facilitate easier breathing. However, excessive humidity should be avoided to prevent skin maceration and fungal growth.
3. Individualized care: Each baby’s needs may differ, and healthcare providers will assess the baby’s clinical condition and adjust the humidity levels accordingly. They will monitor the baby’s skin integrity, respiratory status, and response to the humidity levels to determine the appropriate range.
It’s important to note that the specific target humidity range and adjustments should be determined by the neonatal care team in consultation with a neonatologist, taking into account the individual baby’s needs and clinical factors.
Parents should discuss the humidity requirements and management plan for their preterm baby with the healthcare team providing care for their child. The healthcare professionals can provide specific guidance and monitor the baby’s response to ensure optimal care.
Tell me about how to minimize lung damage in a preterm neonate
Minimizing lung damage in preterm neonates is a crucial aspect of their care to support optimal respiratory function and long-term health outcomes. Here are some strategies commonly employed in neonatal intensive care units (NICUs) to help minimize lung damage in preterm neonates:
1. Antenatal corticosteroids: Administering antenatal corticosteroids to pregnant mothers at risk of preterm birth can significantly improve lung maturity in the fetus. This reduces the risk of respiratory distress syndrome and other lung complications.
2. Surfactant replacement therapy: For neonates with respiratory distress syndrome, surfactant replacement therapy is often provided to restore the surfactant levels in the lungs. Surfactant helps reduce surface tension and keeps the alveoli open, preventing lung collapse.
3. Respiratory support: Various forms of respiratory support may be employed, such as nasal continuous positive airway pressure (nCPAP) or mechanical ventilation. These interventions help support adequate oxygenation and ventilation, preventing lung injury due to respiratory failure.
4. Gentle ventilation strategies: To minimize lung injury from mechanical ventilation, strategies like lung protective ventilation are employed. These techniques involve using lower tidal volumes, optimizing positive end-expiratory pressure (PEEP), and monitoring lung mechanics to avoid excessive lung stretch and barotrauma.
5. Oxygen therapy: Maintaining appropriate oxygen levels is crucial. Oxygen therapy is titrated to avoid both hypoxia and excessive oxygen exposure, which can lead to oxygen toxicity and lung injury. Close monitoring and adjustment of oxygen levels are essential.
6. Temperature regulation: Maintaining a stable body temperature is important as temperature instability can stress the respiratory system. Preterm infants are susceptible to hypothermia, which can lead to increased oxygen demand and respiratory distress. Incubators or radiant warmers are used to maintain a neutral thermal environment.
7. Infection prevention: Infections can exacerbate lung damage in preterm neonates. Strict infection control measures, including hand hygiene, aseptic techniques, and appropriate use of antibiotics, are implemented to minimize the risk of respiratory infections.
8. Nutrition: Adequate nutrition, including optimal provision of fluids, calories, and essential nutrients, is crucial for supporting lung development and overall growth. Breast milk is preferred when possible due to its protective effects.
9. Developmental care: Minimizing stress and providing a supportive developmental environment for preterm neonates is important. Techniques such as minimizing handling, promoting kangaroo care (skin-to-skin contact), and reducing environmental stimuli can help reduce lung stress and improve outcomes.
It’s important to note that the specific management and interventions will depend on the baby’s individual needs and condition. Neonatal care teams, including neonatologists, nurses, and respiratory therapists, provide individualized care plans based on the best available evidence and clinical expertise.
Parents should consult with the healthcare team caring for their preterm baby to understand the specific strategies and interventions being employed to minimize lung damage and support their baby’s respiratory health.
How to minimize interruptions and allow the patient to rest in the NICU?
Minimizing interruptions and creating a restful environment for patients in the neonatal intensive care unit (NICU) is important for their well-being and recovery. Here are some strategies that can help achieve this goal:
1. Implement care bundles: Care bundles are sets of evidence based practices that aim to improve patient care. NICUs often utilize care bundles specifically designed to minimize interruptions and promote restful periods for infants. These bundles typically include synchronized care approaches and cluster care techniques, where multiple interventions are combined to minimize disruptions.
2. Quiet and dim environment: Creating a calm and soothing environment can contribute to improved rest and sleep for neonates. Maintain a quiet atmosphere in the NICU by reducing unnecessary noise, such as alarms and conversations. Ensure that lighting is dim and avoid excessive exposure to bright lights during rest periods.
3. Promote developmental care: Developmental care principles focus on providing a nurturing environment that supports the developmental needs of preterm infants. This includes techniques such as swaddling, providing gentle touch, and promoting kangaroo care (skin-to-skin contact) when appropriate. These interventions can help soothe the baby and facilitate better rest.
4. Coordinate care activities: Communication and coordination among the healthcare team are crucial in minimizing interruptions. Implementing scheduled care routines and coordinating interventions such as vital sign assessments, medication administration, and diaper changes can help cluster activities and reduce disturbances during rest periods.
5. Parental involvement: Encouraging parental involvement in the care of their baby can contribute to improved rest. When feasible and appropriate, parents can participate in activities such as kangaroo care, feeding, and comforting their baby. This not only supports bonding but also helps the baby feel secure and calm.
6. Monitor noise levels: Regularly monitoring and assessing noise levels in the NICU can help identify sources of disturbance. Implementing strategies like noise reduction protocols, using noise monitoring devices, and providing staff education on noise management can help maintain a quieter environment.
7. Staff education and awareness: Educating NICU staff about the importance of minimizing interruptions and creating a restful environment is essential. Training programs can focus on strategies for optimizing care delivery, reducing noise, and coordinating activities to ensure a patient-centered approach.
8. Use technology effectively: Utilize technology solutions to streamline processes and reduce unnecessary interruptions. Electronic medical records, bedside monitors, and communication tools can help facilitate efficient and coordinated care, minimizing the need for frequent interruptions. It’s important to note that individual patient needs may vary, and healthcare providers in the NICU will adapt their care strategies accordingly. Parents can communicate their preferences for their baby’s rest periods and collaborate with the healthcare team to promote a restful environment. Discussing these strategies with the NICU staff and seeking their guidance will ensure that the specific needs of the baby are considered and appropriate measures are taken to minimize interruptions and optimize rest in the NICU setting.
Can Chat GPT be incorporated into EMR while still maintaining HIPAA compliance?
Integrating Chat GPT or any AI system into an Electronic Medical Record (EMR) system while maintaining HIPAA compliance is a complex task that requires careful consideration of privacy and security measures. Here are some key points to keep in mind:
1. Data privacy and security: Protecting patient data is of utmost importance. Any integration of Chat GPT into an EMR system should adhere to strict data privacy and security protocols. This includes ensuring secure transmission of data, encrypting sensitive information, and implementing access controls to limit data access to authorized personnel.
2. De-identification of data: Patient data used for training or interacting with Chat GPT should be properly de-identified to remove any personally identifiable information. This helps maintain privacy and HIPAA compliance by preventing the disclosure of identifiable patient information.
3. User authentication and access controls: Implement robust user authentication mechanisms and access controls within the EMR system to ensure that only authorized healthcare professionals can access patient data and interact with Chat GPT. This helps prevent unauthorized access and maintains the privacy of patient information.
4. Audit logs and monitoring: Implementing audit logs and monitoring mechanisms can help track system activity, detect and respond to any potential security breaches or unauthorized access attempts. Regular monitoring and review of these logs can help ensure compliance with HIPAA regulations.
5. Business Associate Agreement (BAA): If the integration involves a third-party AI provider, ensure that a Business Associate Agreement (BAA) is in place. A BAA establishes the legal requirements and responsibilities of the AI provider regarding the protection and handling of patient data.
6. Regular security assessments: Conduct regular security assessments, vulnerability testing, and risk assessments to identify and address any potential security vulnerabilities in the integrated system. This helps ensure ongoing compliance and protection of patient data.
It’s important to note that while Chat GPT can provide valuable assistance in various healthcare contexts, it’s crucial to consult with legal and compliance experts, as well as involve appropriate stakeholders within the healthcare organization, to ensure that the integration of Chat GPT into an EMR system meets the specific requirements of HIPAA compliance and local regulations.
Can Chat GPT be used to establish and improve contact with families for follow up?
Yes, Chat GPT can be used to establish and improve contact with families for follow-up purposes. Here are a few ways in which Chat GPT can be utilized:
1. Automated messaging: Chat GPT can be programmed to send automated messages to families, providing updates, reminders, and important information regarding follow-up appointments, test results, or medication schedules. These messages can be personalized based on the individual patient’s needs.
2. Answering common questions: Chat GPT can be trained with a database of frequently asked questions related to follow-up care. This can help provide families with quick and accurate responses to common inquiries, saving time and improving communication efficiency.
3. Appointment scheduling: Chat GPT can assist families in scheduling follow-up appointments by offering available dates and times, guiding them through the process, and sending appointment reminders.
4. Educational resources: Chat GPT can provide families with educational materials and resources related to their child’s condition, treatment, or follow-up care. This can include articles, videos, and links to trusted sources, empowering families with information to support their understanding and decision-making.
5. Monitoring and feedback: Chat GPT can facilitate ongoing communication between healthcare providers and families by allowing families to provide updates on their child’s progress, report any concerns or changes in symptoms, and receive appropriate guidance or recommendations from the healthcare team.
It’s important to note that while Chat GPT can enhance communication and provide valuable support, it is not intended to replace direct interactions with healthcare professionals. It should be seen as a complementary tool to facilitate engagement and improve access to information and resources.
When implementing Chat GPT for follow-up communication with families, it’s essential to ensure data privacy and security, comply with relevant regulations (such as HIPAA), and have mechanisms in place for families to escalate urgent concerns or access direct human support when needed.
Can Chat GPT be used to improve compliance with taking meds and establishing follow up appointments?
Yes, Chat GPT can be used to improve compliance with taking medications and establishing follow-up appointments. Here are a few ways in which it can assist:
1. Medication reminders: Chat GPT can send personalized medication reminders to patients or caregivers via automated messages. These reminders can help individuals remember to take their medications at the prescribed times, improving medication adherence.
2. Medication information: Chat GPT can provide information about medications, including dosage instructions, potential side effects, and precautions. It can address common questions or concerns related to the medications, helping patients and caregivers make informed decisions and understand the importance of adherence.
3. Tracking and monitoring: Chat GPT can assist in tracking medication adherence by providing a platform for patients or caregivers to report medication intake. It can also remind patients to refill their prescriptions when needed, ensuring a continuous supply of medication.
4. Follow-up appointment scheduling: Chat GPT can assist in scheduling follow-up appointments by providing available dates and times, helping patients or caregivers find suitable slots, and sending reminders prior to the appointments. This can improve compliance with follow-up visits and ensure continuity of care.
5. Communication and feedback: Chat GPT can serve as a communication channel between patients or caregivers and healthcare providers, allowing them to ask questions, provide updates on medication response or side effects, and receive guidance or adjustments to their treatment plan.
By using Chat GPT to improve compliance with medication regimens and follow-up appointments, healthcare providers can enhance patient engagement, provide timely support, and potentially improve health outcomes. However, it’s important to note that Chat GPT should be seen as a supportive tool, and direct communication with healthcare professionals should still be encouraged for more complex or urgent concerns.
Additionally, privacy and security measures must be in place to protect patient information and comply with relevant regulations, such as HIPAA.
Can Chat GPT be used to improve adherence and compliance with protocols in inpatient setting?
Yes, Chat GPT can be used to improve adherence and compliance with protocols in an inpatient setting. Here are some ways in which it can be utilized:
1. Protocol reminders: Chat GPT can send reminders to healthcare providers regarding specific protocols or guidelines that need to be followed during patient care. These reminders can help reinforce adherence to established protocols and ensure consistency in practice.
2. Access to protocols and guidelines: Chat GPT can provide healthcare providers with easy access to protocols and guidelines at the point of care. This can assist in quickly referencing the appropriate protocols and ensuring they are followed correctly.
3. Real-time guidance: Chat GPT can offer real-time guidance and decision support to healthcare providers as they navigate complex protocols. It can help clarify any uncertainties or questions that arise during patient care, ensuring adherence to established guidelines.
4. Training and education: Chat GPT can serve as a training tool to educate healthcare providers on various protocols, procedures, and best practices. It can provide interactive learning experiences and answer questions related to protocol adherence, promoting knowledge retention and application.
5. Data tracking and analysis: Chat GPT can assist in tracking adherence to protocols by collecting and analyzing data related to protocol compliance. It can generate reports and insights that can be used for quality improvement initiatives and identifying areas for targeted interventions.
6. Collaboration and communication: Chat GPT can facilitate communication and collaboration among healthcare providers by providing a platform for sharing experiences, discussing protocol-related challenges, and exchanging best practices. This can promote a culture of adherence and continuous learning.
While Chat GPT can be a valuable tool in promoting adherence and compliance with protocols, it’s important to note that it should not replace clinical judgment or the expertise of healthcare providers. It should be seen as a supportive resource that enhances decision-making and promotes standardized care.
Additionally, the implementation of Chat GPT in the inpatient setting should consider the privacy and security of patient information, compliance with relevant regulations, and integration with existing healthcare systems to ensure seamless workflow and usability.
Can Chat GPT be used to alert the physicians of impending sepsis in a newborn based on vital sign data?
Chat GPT can be used as part of a system to alert physicians of potential signs of sepsis in a newborn based on vital sign data. However, it’s important to note that as an AI language model, Chat GPT doesn’t have direct access to real-time patient data or the ability to monitor vital signs in real-time. It relies on receiving information from external sources.
To implement a system using Chat GPT for sepsis alerts, the following steps can be considered:
1. Data integration: Integrate the vital sign monitoring system used in the neonatal intensive care unit (NICU) with the AI system. This integration allows real-time transmission of vital sign data to the system.
2. Data analysis and interpretation: Develop algorithms or models that analyze the incoming vital sign data to detect patterns or indicators associated with sepsis. This could involve machine learning techniques trained on historical data to identify potential signs of sepsis based on vital sign trends.
3. Alert generation: Once the AI system detects patterns or indicators suggestive of sepsis, it can generate an alert or notification. At this point, Chat GPT can be involved to communicate the alert to the physicians or healthcare providers. The model can provide additional information or guidance based on the specific alert to assist in clinical decision-making.
4. Physician response and intervention: Physicians would then review the alert provided by Chat GPT, assess the patient’s condition, and initiate appropriate interventions based on clinical judgment and guidelines for sepsis management. It’s important to highlight that the design and implementation of such a system require collaboration with healthcare professionals, data scientists, and system developers. The system must undergo rigorous testing and validation to ensure accuracy, reliability, and safety. Additionally, compliance with privacy regulations and ethical considerations related to patient data handling should be a priority.
Overall, Chat GPT can play a role in alerting physicians to potential signs of sepsis in newborns based on vital sign data, but it should be integrated into a comprehensive system that combines real-time data monitoring, analysis algorithms, and physician intervention to effectively improve patient outcomes.
Can Chat GPT be used to formulate a nutrition plan for a neonate based on ongoing co-morbidities?
Chat GPT can assist in formulating a nutrition plan for a neonate based on ongoing co-morbidities by providing general information and suggestions. However, it’s important to note that the information provided by Chat GPT should not replace the expertise and guidance of a healthcare professional, such as a neonatologist or a registered dietitian.
When creating a nutrition plan for a neonate with ongoing comorbidities, it is crucial to consider several factors, including the specific medical condition, gestational age, weight, growth patterns, organ function, allergies, and any other individualized needs. These considerations require the expertise and clinical judgment of healthcare professionals who have a comprehensive understanding of the neonate’s medical history and current status.
While Chat GPT can offer general information on nutritional guidelines and considerations, it cannot take into account the unique circumstances and complexities of an individual neonate’s case. Therefore, it’s important to consult with the healthcare team and seek guidance from specialists who can provide tailored recommendations based on the neonate’s specific needs and comorbidities.
Chat GPT can, however, provide general information on topics such as the nutritional requirements of preterm infants, guidelines for feeding and fortification of breast milk or formula, introduction of solid foods, considerations for specific co-morbidities, and potential nutritional challenges that may arise. In summary, while Chat GPT can provide general information on neonatal nutrition, it should not be solely relied upon for formulating a nutrition plan for a neonate with ongoing co-morbidities. Collaborating with healthcare professionals who specialize in neonatal nutrition and following their guidance is crucial to ensure the best outcomes for the neonate’s nutritional needs.
Can we trust the facts that you provide? As an AI language model, my responses are generated based on a mixture of licensed data, data created by human trainers, and publicly available data. I have not been directly trained on specific medical databases or have access to proprietary medical information. While I strive to provide accurate and up-to-date information, it’s important to note that I can’t guarantee the accuracy or reliability of the facts I present.
I should not be considered as a substitute for professional medical advice, diagnosis, or treatment. Always consult with a qualified healthcare professional or trusted source for specific medical concerns or information. They can provide personalized guidance based on your individual circumstances.
It’s also worth noting that information in the healthcare field is constantly evolving, and new research can lead to updates and changes in understanding. Therefore, it’s always a good idea to verify information from multiple reputable sources and consult with healthcare professionals for any medical decisions or concerns.
If you have any specific questions or concerns about the accuracy of information provided by Chat GPT, please let me know, and I’ll do my best to address them or provide additional context
Where do you get your information from?
As an AI language model, my responses are generated based on a diverse range of sources and data. During my training, I was exposed to a large corpus of text from the internet, including books, articles, websites, and other texts, to develop a broad understanding of human language. This corpus covers a wide array of topics, including but not limited to, general knowledge, scientific literature, medical textbooks, and research papers. It’s important to note that while I strive to provide accurate and up-to-date information, I do not have direct access to current medical databases or proprietary medical sources. Therefore, my responses may not always reflect the most recent advancements or specialized knowledge in specific medical fields.
I should be used as a helpful resource for general information and guidance, but it’s crucial to consult with qualified healthcare professionals or refer to reputable medical sources for specific medical advice or decisions.
If you have any specific questions or concerns about the sources of information used by Chat GPT, feel free to ask, and I’ll do my best to provide further clarification.
Can you write a discharge summary for a 25-week gestation infant that was in the NICU for 12 weeks?
Patient: [Infant’s Name] Date of Birth: [Date of Birth] Gestational Age at Birth: 25 weeks Date of Discharge: [Date of Discharge] Length of Stay: 12 weeks
Diagnosis and Clinical Course: [Infant’s Name] was born prematurely at 25 weeks gestation and required intensive care in the NICU. The initial assessment revealed respiratory distress syndrome (RDS) necessitating mechanical ventilation and surfactant therapy. [He/She] also developed a patent ductus arteriosus (PDA) and received medical treatment with indomethacin, which led to successful closure. During the course of [his/her] stay, [he/she] experienced episodes of apnea, which were managed with caffeine therapy.
[Infant’s Name] demonstrated gradual improvement in respiratory function and feeding tolerance over the 12-week hospitalization period. [He/She] successfully transitioned from mechanical ventilation to non-invasive respiratory support, including nasal continuous positive airway pressure (nCPAP) and high-flow nasal cannula. [His/Her] nutritional needs were initially met through total parenteral nutrition (TPN) and gradually transitioned to enteral feeds, primarily fortified human milk.
Additional interventions included monitoring for infection, which involved blood culture surveillance, antibiotic therapy, and sepsis workup whenever indicated. Serial cranial ultrasounds were performed to monitor for intraventricular hemorrhage (IVH) and periventricular leukomalacia (PVL). Fortunately, [Infant’s Name] did not develop significant intracranial abnormalities.
During the hospital stay, [he/she] received appropriate multidisciplinary care, including consultations with pediatric subspecialists, occupational therapy, and ophthalmology assessments. Regular growth and developmental assessments were conducted, and appropriate interventions were implemented to support [his/her] overall growth and neurodevelopmental progress.
Summary of Discharge Condition: At the time of discharge, [Infant’s Name] is clinically stable with improved respiratory function, adequate feeding tolerance, and weight gain. [He/She] has transitioned to full oral feeds and is maintaining appropriate growth velocity. [His/Her] oxygen requirement has significantly reduced, and [he/she] no longer requires respiratory support.
Instructions and Follow-Up:
1. [Infant’s Name] should be closely followed by a pediatrician or neonatologist for ongoing growth monitoring, immunizations, and developmental assessments.
2. Family education regarding safe sleep practices, infection prevention, and general care of a premature infant should be provided.
3. A referral to early intervention programs or developmental follow-up clinics may be necessary to support [Infant’s Name]’s developmental progress.
4. Ensuring a supportive and nurturing home environment with adequate follow-up care and regular healthcare visits is crucial.
Family Support and Resources: The family has been provided with extensive counseling, emotional support, and education throughout the NICU stay. They have been connected with appropriate community resources, support groups, and local organizations specializing in neonatal care.
It is essential to recognize that [Infant’s Name] will require ongoing [CHAT GPT stopped responding]
Regenerated response:
Discharge Summary
Patient Information:
• Name: [Infant’s Name] • Date of Birth: [Date of Birth] • Gestational Age at Birth: 25 weeks
• Length of NICU Stay: 12 weeks
Medical History and Diagnosis: [Provide a brief overview of the infant’s medical history and any significant diagnoses or conditions they experienced during their stay in the NICU. Include information on any complications, interventions, or procedures performed.]
Treatment and Management: [Describe the treatments, interventions, and management strategies that were implemented during the infant’s NICU stay. This may include respiratory support, nutrition, medication administration, specialized monitoring, or surgical procedures.]
Progress and Achievements: [Highlight the infant’s progress and achievements during their NICU stay, including improvements in respiratory status, weight gain, feeding milestones, neurological development, and any other notable achievements.]
Outcomes and Prognosis: [Provide an assessment of the infant’s overall health and prognosis at the time of discharge. Discuss any ongoing concerns or follow-up requirements, and provide recommendations for ongoing care and monitoring.]
Plan of Care: [Outline the plan of care following discharge, including any medications, feeding regimen, follow-up appointments, and necessary support services. Include recommendations for developmental follow-up, immunizations, and any specific instructions for the parents or caregivers.]
Education and Support: [Detail the education and support provided to the parents or caregivers during the infant’s NICU stay, including information on infant care, feeding techniques, monitoring signs of illness, and available resources for ongoing support.]
Recommendations and Referrals: [Make appropriate recommendations and referrals based on the infant’s specific needs. This may include referrals to specialists, early intervention services, community resources, or support groups.]
Follow-up Appointments: [Provide a schedule of recommended follow-up appointments with the pediatrician, specialists, or developmental clinics. Include dates, times, and any specific instructions for scheduling these appointments.]
Discharge Medications: [List any medications prescribed at the time of discharge, along with dosages, administration instructions, and possible side effects.]
Contact Information: [Provide contact information for the healthcare team, including the primary care provider, specialty clinics, and any other relevant contacts for the parents or caregivers to reach out to in case of questions or concerns.]
Please note that this discharge summary is a generalized example and should be tailored to the specific medical condition and requirements of the individual infant. Actual discharge summaries are typically created by healthcare professionals involved in the care of the infant, and they contain more detailed information and documentation specific to the patient’s case.
Have you ever gotten anyone into legal trouble?
As an AI language model, I don’t have the capability to take actions or cause direct consequences in the real world. I don’t have personal interactions or engage in activities that could lead to legal trouble for individuals. However, it’s important to note that while I strive to provide accurate and helpful information, the responsibility for using and interpreting that information lies with the user. It’s always advisable to consult with qualified professionals or trusted sources for specific legal advice or when making decisions that may have legal implications. If you have any concerns about legal matters, it’s best to consult with a legal professional who can provide appropriate guidance based on your specific situation and jurisdiction. Routine maintenance issues, like medication reminders and monitoring and scheduling follow-up appointments, allowing doctors and other care specialists more time to address specific, more serious issues that may arise. While AI, like Chat GPT, may already be useful in assisting some aspects of patient care, it will still be some time before it can be implemented to assist physicians in making real-time decisions in patient care. Until then and even afterward, we neonatologists still need to keep abreast of the latest advancements, research, and guidelines and use our best clinical judgment based on these and our experience to provide the best care for our patients since AI, no matter how advanced, thus far cannot replace human intuition and experience.
Source:http://neonatologytoday.net/newsletters/nt-jun23.pdf


Hello, young innovators of the digital age!
In the vast expanses of the cosmos, one universal truth prevails: change is inevitable. Nothing remains the same, and this constant evolution is the backbone of our existence. The change you seek in the world begins with you, and in the digital era, you’re bestowed with abundant platforms to ignite this change, influence others, and make your voice heard.
As youth in today’s interconnected world, you are explorers charting a course across the digital landscape, driven by curiosity, fueled by a sense of adventure, and bound together by a shared love for exploration. Your natural inclination as changemakers can be heightened and expanded via online platforms, enabling you to engage on a global scale.
So how can you make the most of these opportunities? Here are a few pointers:
Champion Curiosity:
Encourage your natural curiosity and quest for knowledge. Be fearless in your exploration of new ideas and perspectives. Social media platforms and various online forums offer vast learning opportunities.
Choose Your Tribe(s):
Surround yourself with people who appreciate your adventurous spirit and love for exploration. Join online communities that align with your interests and passions. Their encouragement will only propel you further on your journey.
Create and Share Positivity:
Make it a point to spread positivity online. Share your growth, achievements, and lessons learned. Your story might just inspire someone else.
Seek Personal Growth:
Utilize online resources to enhance your skills, learn new ones, and expand your knowledge base. Online courses, webinars, and tutorials are just a few clicks away.
Make Connections:
Engage with like-minded individuals across the globe. Foster friendships, find mentors, and collaborate on projects. Remember, the internet erases geographical boundaries.
Inspire and Be Inspired:
Use your digital presence to inspire others, but also let yourself be inspired. Celebrate the achievements of your peers and let their success stories motivate you.
In this journey, it’s essential to remember that personal growth and the ability to influence others start from within. Grow in ways that resonate with you, that make you feel good about yourself, and you’ll find that you naturally attract others who share your vibes.
As the young navigators of the digital world, you hold immense power. Your actions, your posts, your shares can shape the world in remarkable ways. Embrace this power, use it wisely, and become the digital changemakers the world needs.
Remember, in the grand scheme of the universe, we’re all part of the process of constant change. As the youth of today, it’s your time to steer this change towards a brighter, better future. So, dive into the digital world with an open mind, a curious heart, and the spirit of an explorer. The journey is just beginning!
Below are a few resources we have found to be reputable and secure and that provide youth with opportunities to connect. Other great sources for positive internet and social media resources include teachers, librarians, school counselors, friends and family!

Kidnected World:https://kidnectedworld.org/
One Global Kids:https://oneglobekids.org/
Connect All Kids: https://www.connectallkids.com/
*** Check with your parents/caretakers prior to accessing these websites so that they may also provide support and assistance as needed.



Hi Friends! On this episode of Nighty Nights with Miss Neli, we will be reading Faces of the NICU By: Shatoya Lewis & Latoya Lewis-Young Book Description: This book tells readers all about all of the different faces that work in the NICU with Preemie and NICU babies. Join Miss Neli as we learn about the different things they do!
Libyan’s enjoy Tripoli’s first skatepark

The US-funefaclity is a first
The US-funded facility is a first in the Libyan capital and aims to help build better community links amongst the city’s young.


in the Libyan capital and aims to help build better community links amongst the city’s young.
Tripoli’s first skateparLibyan’s enjoy Tripoli’s first skateparkkLibyan’s enjoy Tripoli’s first skatepark
