

North Korea, officially the Democratic People’s Republic of Korea (DPRK), is a country in East Asia. It constitutes the northern half of the Korean Peninsula and borders China and Russia to the north at the Yalu (Amnok) and Tumen rivers, and South Korea to the south at the Korean Demilitarized Zone. The country’s western border is formed by the Yellow Sea, while its eastern border is defined by the Sea of Japan. North Korea, like its southern counterpart, claims to be the legitimate government of the entire peninsula and adjacent islands. Pyongyang is the capital and largest city.
Officially, North Korea is an “independent socialist state” which holds democratic elections; however, outside observers have described the elections as unfair, uncompetitive, and pre-determined, in a manner similar to elections in the Soviet Union. The Workers’ Party of Korea is the ruling party of North Korea. According to Article 3 of the constitution, Kimilsungism–Kimjongilism is the official ideology of North Korea. The means of production are owned by the state through state-run enterprises and collectivized farms. Most services—such as healthcare, education, housing, and food production—are subsidized or state-funded.
North Korea has a life expectancy of 72.3 years in 2019, according to HDR 2020. While North Korea is classified as a low-income country, the structure of North Korea’s causes of death (2013) is unlike that of other low-income countries. Instead, it is closer to worldwide averages, with non-communicable diseases—such as cardiovascular disease and cancers—accounting for 84 percent of the total deaths in 2016.
In 2013, cardiovascular disease as a single disease group was reported as the largest cause of death in North Korea. The three major causes of death in North Korea are stroke, COPD and Ischaemic heart disease. Non-communicable diseases risk factors in North Korea include high rates of urbanization, an aging society, and high rates of smoking and alcohol consumption amongst men.
Maternal mortality is lower than other low-income countries, but significantly higher than South Korea and other high income countries, at 89 per 100,000 live births. In 2008 child mortality was estimated to be 45 per 1,000, which is much better than other economically comparable countries.
https://en.wikipedia.org/wiki/North_Korea
GLOBAL PRETERM BIRTH RATES –North Korea
- Preterm Birth Rate North Korea – 10%
- (Global Average: 10.6)
- Source- Daily NK-North Korea

COMMUNITY

Relaxation Therapy and Human Milk Feeding Outcomes
A Systematic Review and Meta-Analysis
Ilana Levene, BM, BCh1; Nurul Husna Mohd Shukri, PhD2; Frances O’Brien, MB, BS3; et alMaria A. Quigley, MSc4; Mary Fewtrell, MD5 – May 6, 2024
Key Points
Question What is the association between the provision of a relaxation intervention and lactation outcomes?
Findings In this systematic review and meta-analysis including 1871 participants, heterogeneous relaxation interventions (including music, meditation, mindfulness, and guided relaxation) were compared with standard care. Results suggest that provision of relaxation was associated with an increase in human milk quantity and infant weight gain and a slight reduction in stress and anxiety.
Meaning Relaxation interventions can be offered to lactating parents who would like to improve milk supply and increase well-being.
Abstract
Importance Human milk feeding is a key public health goal to optimize infant and maternal/parental health, but global lactation outcomes do not meet recommended duration and exclusivity. There are connections between lactation and mental health.
Objective To appraise all available evidence on whether the provision of relaxation interventions to lactating individuals improves lactation and well-being.
Data Sources Embase, MEDLINE, CINAHL, Allied and Complementary Medicine Database, Web of Science, and the Cochrane Library were searched on September 30, 2023, and topic experts were consulted.
Study Selection Two independent reviewers screened for eligibility. Inclusion criteria were full-text, peer-reviewed publications with a randomized clinical trial design. Techniques that were entirely physical (eg, massage) were excluded. A total of 7% of initially identified studies met selection criteria.
Data Extraction and Synthesis Two independent reviewers extracted data and assessed risk of bias with the Cochrane Risk of Bias 2 tool. Fixed-effects meta-analysis and Grading of Recommendations, Assessment, Development, and Evaluations guidelines were used to synthesize and present evidence.
Main Outcomes and Measures Prespecified primary outcomes were human milk quantity, length and exclusivity of human milk feeding, milk macronutrients/cortisol, and infant growth and behavior.
Results A total of 16 studies were included with 1871 participants (pooled mean [SD] age for 1656 participants, 29.6 [6.1] years). Interventions were music, guided relaxation, mindfulness, and breathing exercises/muscle relaxation. Provision of relaxation was not associated with a change in human milk protein (mean difference [MD], 0 g/100 mL; 95% CI, 0; 205 participants). Provision of relaxation was associated with an increase in human milk quantity (standardized mean difference [SMD], 0.73; 95% CI, 0.57-0.89; 464 participants), increased infant weight gain in breastfeeding infants (MD, z score change = 0.51; 95% CI, 0.30-0.72; 226 participants), and a slight reduction in stress and anxiety (SMD stress score, −0.49; 95% CI, −0.70 to −0.27; 355 participants; SMD anxiety score, −0.45; 95% CI, −0.67 to −0.22; 410 participants).
Conclusions and Relevance Results of this systematic review and meta-analysis suggest that provision of relaxation was associated with an increase in human milk quantity and infant weight gain and a slight reduction in stress and anxiety. Relaxation interventions can be offered to lactating parents who would like to increase well-being and improve milk supply or, where directly breastfeeding, increase infant weight gain.


The Current Status in Obstetrics in North Korea and Strategies for Establishing a Better Healthcare System

Joseph J. Noh – Published online 2021 Dec 24
Abstract
The women’s healthcare in North Korea is in poor condition. The present study explored the current state of women’s healthcare, especially in the field of obstetrics, in the region with a number of considerations in regards to establishing a better healthcare system. Peer-reviewed journal articles and reports from intergovernmental organizations were reviewed. Data show that many healthcare facilities suffer from shortages of basic amenities. The maternal mortality ratio was 82 deaths per 100,000 live births. The leading cause of maternal death was postpartum hemorrhage. It was also found that many hospitals were unable to provide adequate obstetrical emergency care such as anticonvulsants, antibiotics, and blood products. A long-term roadmap that is sustainable with clear principles and that is not disturbed by political tensions should be established.

Full Article https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2021.744326/full

Kim Ok-Ju – Shining Motherland (빛나는 조국) | 4K 50fps
Sep 27, 2023
The grand final performance by the great 김옥주, her vocal might radiating throughout Pyongyang. After a brief hiatus, this rendition removes all doubt of her place at the very top – Korea’s most legendary singer of the 2020s. (So far..) 빛나는 조국 is seen somewhat as the DPRK’s second national anthem, even replacing it at times, though the lyrics are rarely sang aloud. Every KCTV Broadcast concludes with this song, making it the perfect bookend to the 75th Anniversary Concert.


HEALTHCARE PARTNERS

Quality Improvement Methods Centered on Pain Management Lead to Better Outcomes in the NICU
Apr. 19, 2024 – A Switch to Tylenol Leads to Fewer Unplanned Intubations and Improved Mortality

A quality improvement (QI) initiative to standardize care for babies in the NICU following surgery at the University of Rochester Medical Center (URMC) correlated with fewer unplanned intubations and improved mortality rates.
The study, “Reducing Unplanned Intubations in the Neonatal Intensive Care Unit After Children’s Surgery: A Quality Improvement Project,” streamlined care following surgery in 2019 through routine use of acetaminophen (Tylenol) for pain control, rather than opioids, and use of a checklist to ensure patients were ready for extubation. To understand the impact of these changes, the authors observed the rate of unplanned intubations over time using statistical process control charts.
Following these changes, the number of unplanned intubations decreased more than 75%, resulting in 11 fewer unplanned intubations each year in the NICU. The percent of infants receiving acetaminophen following surgery increased from 25% to 90%, which resulted in a significant decline in opioid exposure during the post-operative period. These improvements have been sustained for more than two years, and in addition, the 30-day mortality rate for postoperative patients in the NICU significantly declined from 6.5% to 0.7%, a nearly 90% decrease.
Surgeries for pre-term babies can occur for a variety of reasons, including addressing congenital defects as well as helping the development of systems that are typically immature at the time of delivery.
Using opioids for pain management after neonatal surgery had been standard practice in hospitals, but increases the risk of respiratory depression, which can then lead to unplanned intubations. “Reducing unplanned intubations matters to patients, because they are associated with increased length of stay, additional complications, and mortality,” said study co-author Jeffrey Meyers, MD, neonatologist and Associate Chief Quality Officer at UR Medicine Golisano Children’s Hospital (GCH).
A multidisciplinary team involving surgeons, neonatologists, anesthesiologists, pharmacists, and other improvement experts engaged in this QI project after noticing that a higher number of infants were experiencing unplanned intubations after surgery relative to peer institutions. The team responded by applying a standardized approach, including a post-operative huddle and checklist to document and communicate what happened in each case in order to create best practices.
After applying these standards, it soon became clear that opioid use was highly correlated with the increase in unplanned intubations.
“Babies are already prone to not breathing normally, and opioids can cause apnea and respiratory depression,” said Derek Wakeman, MD, co-author and surgeon at GCH. “We transitioned to maximizing non-opioid medication.”
Most babies in the NICU need Tylenol to be given through an IV, as alternative routes such as rectal are less effective. IV Tylenol, however, had limited availability until the last 5-10 years, and this improved availability helped facilitate the transition in the GCH NICU.
While there were initial concerns about Tylenol providing the correct amount of pain management, most babies in the NICU responded well to treatment, according to Wakeman.
The GCH NICU has now transitioned to using Tylenol as the first-line option following surgery. This is the first documented QI initiative to successfully reduce unplanned intubations in neonates, and one of the first to link opioid stewardship with improved post-operative outcomes. Wakeman and Meyers hope that this will help facilitate a more rapid transition to Tylenol in NICUs across the country.
Wakeman and Meyers credit Peter Juviler, MD, surgical resident, for data compilation, analysis, and drafting the manuscript.
“Opioid stewardship is an important topic across all parts of the health care system, and it’s important for these practices to be examined in the NICU,” said Meyers. “Pain management is important, but we should continue to critically examine how and where we use medications that have risks, such as opioids, and seek alternatives that can provide appropriate analgesia. This project speaks to the importance of using self-assessment to improve outcomes.”


In this episode Michelle J. White MD, MPH, FAAP, explains the concept of a “built environment” and how the infrastructure where people live can affect their health. Hosts David Hill, MD, FAAP, and Joanna Parga-Belinkie, MD, FAAP, also speak with Henry Lee, MD, FAAP, about new suggested changes to the Neonatal Resuscitation Program.


Growth of Preterm and Small Infants: Dispelling Myths
May 22, 2024 by Eric Graber
Advances in Nutrition review notes that most preterm infants catch up to full-term infant growth patterns within three years
“Several myths surround the growth of preterm and small infants,” according to Expected and Desirable Preterm and Small Infant Growth Patterns, the scientific review published in Advances in Nutrition: An International Review Journal, a publication of the American Society for Nutrition. According to the authors, Dr. Tanis R. Fenton et. al., these myths are “often founded in the prevalent misconceptions that fetal and infant growth patterns solely and strongly predict future risks of obesity, cardiovascular disease, and metabolic disorders.”
In order to dispel these myths and shed an objective light on the subject, this review examined the full spectrum of infant growth expectations, focusing on how preterm infants’ growth may be similar to or different from full-term infants’ growth. Moreover, the authors emphasized how science should inform how nutritionists and healthcare providers talk to and counsel parents.
A common concern among neonatologists has been that if the diets and treatment plans for preterm and small infants lead them to grow too quickly, catching up to the growth expectations for full-term babies, they will have higher risks of obesity and cardiovascular disease in later life. This review, however, found that preterm and small infants are not necessarily at higher risk for obesity and cardiovascular disease in the long term, but rather “the long-term risks for obesity and cardiovascular disease is influenced by a combination of modifiable and nonmodifiable factors, including genetics, social determinants of health, prenatal history and nutrition, as well as later life lifestyle choices, including physical activity, nutrition and energy balance.”
Adequate nutrition and growth are both necessities for neurodevelopment. However, just as the authors pointed to a more complex relationship between preterm infants and obesity and cardiovascular disease, they also pointed to a similarly complex relationship between preterm infants and long-term neurodevelopment. According to the authors, “in neonatal intensive care units that provide good nutrition support as well as nutrition services post-discharge, the causes of poor cognitive outcomes are less likely mediated by poor growth as there are other more influential directly contributing causes.”
An editorial accompanying this review, Revolutionizing Neonatal Nutrition: Rethinking Definitions and Standards for Optimal Care, noted how the review “significantly contributes to our understanding of growth patterns in preterm infants and provides valuable guidance to rethink definitions and standards for optimal nutritional care.” In particular, the author of the editorial, Ariel A. Salas, notes that “the call for the development of individualized growth trajectories due to multicausality in growth outcomes is insightful.”
Individual growth variability is a biological phenomenon influenced by genetics, prenatal growth, morbidities, and nutrition. Thus, it is important to recognize that preterm and full-term infants with healthy outcomes exhibit a wide range of growth variability. Nonetheless, the authors recognize that parents are concerned about children who plot low on growth charts. They stress the importance of avoiding the commonly used word “failure” when discussing an infant’s growth. Even if an infant’s growth is faltering, it can be very harmful and alarming for parents to hear the word “failure” about their child. Similarly, it can be harmful for parents and children to hear the words “obese” or “fat” when used to describe their family member or themselves. Finally, the authors stress that “no specific percentile should be set as a growth goal; individual variability should be expected.”
Overall, “while there may be some challenges and concerns related to preterm growth during the neonatal period, these risks are not necessarily predetermined by an infant’s preterm birth or neonatal intensive care unit course.” In fact, the majority of uncomplicated preterm infants tend to catch up in head circumference, weight, and length measurements between 0 and 36 months.
If you’re interested in learning more about this review and delving more deeply into the many factors that can influence infant growth and health outcomes throughout the lifespan, tune into Dr. Tanis Fenton on Desirable Preterm Infant Growth Patterns. This podcast is Episode Two of the recently launched podcast series Advances in Nutrition: An International Review Journal—The Podcast.
https://nutrition.org/growth-of-preterm-and-small-infants-dispelling-myths/

Infant Health Safety

CALL TO ACTION
We urge hospital administrators, health care providers and policymakers to take steps to ensure the optimal health and safety of infants and young children by heeding three important calls to action.
When hospital procurement decisions are focused on cost, patients pay the price.
Hospitals must include NICU and PICU clinicians in the procurement process for medications, devices, supplies and services to ensure vulnerable infants and young children receive the safest care possible.
Hospital procurement is the process of purchasing medications, devices, and other supplies and services for use at the hospital. Procurement is a long process, usually completed by teams of doctors, nurses and other hospital staff. The process can be a determining factor in health outcomes for patients.
Some hospital procurement teams face pressure to keep costs low, so clinical staff have less input in the process than administrators. This can lead to the hospital purchasing products and services that present safety issues for certain patient populations.
INFANTS AND CHILDREN ARE NOT LITTLE ADULTS.
The problem is especially pressing in neonatal and pediatric intensive care units. For example, the hospital may procure a large inventory of tubing and syringe systems to be used across all hospital units. But these tubing and syringe systems can present serious safety issues for NICU patients.
Inefficient procurement processes can force clinicians to find workarounds, causing them to lose time with their patients. Inventory imbalances in the NICU and PICU can also force hospitals to delay or cancel procedures or treatments.
NICU and PICU clinical staff members know the unique needs of their patients. Ensuring they are part of hospital procurement processes will promote the safest and best care possible for infants and young children.
Infants need medications and devices that are specifically designed and tested for them.
CALL TO ACTION
Policies must prioritize and incentivize companies to develop medications and devices specifically for the neonatal and pediatric populations to ensure safe and optimal care.
Infants and young children need care that is tailored to their needs and size. Infants are not tiny adults, yet they are often given smaller doses of adult medications or smaller sized adult medical devices.
ADULT MEDICATIONS AND DEVICES THAT ARE ALTERED FOR BABIES CAN PRESENT SAFETY CONCERNS.
This practice can result in medication dosing errors or device safety issues, which can lead to poor patient outcomes.
For example, the pulse oximeter was made for adults but was often used on infants. Although the device saved many adult lives, it was not reliable when used on infants and children because they have reduced blood flow to their fingers and toes, which makes it harder to accurately measure oxygen saturation with the oximeter.
Clinicians recognized infants needed technology specifically for their size, and since then, innovators have developed new oxygen monitoring technologies specifically for infants.
But innovation for new medications and devices faces barriers. Innovation for this small group of patients can be costly and time consuming, and enrolling infants and children in clinical trials can be challenging. Providers also need to be willing to become early adopters of new technology.
It is important to ensure each patient in the NICU and PICU receives the highest quality of care during their hospital stay, which includes devices and medications that are specifically designed for their size and unique needs.
Policies that incentivize and prioritize innovation, like patent extensions, priority review vouchers or tax credits, will ensure more innovation to meet the needs of infants and young children.
Suitable hospital staffing leads to positive patient outcomes.
CALL TO ACTION
States should adopt policies that clearly outline acuity-based staffing guidelines, include nurses in decisions about staffing and support their mental health and well-being.
Patients in the NICU and PICU require a high level of care from clinicians, including nurses and nurse practitioners. But when there are not enough clinicians in a unit, it presents a safety risk to patients and affects the mental well-being of clinicians.
Hospitals across the U.S. are facing severe nursing shortages for several reasons, including an aging nursing workforce, burnout, the COVID-19 pandemic, high turnover, lack of clinical educators and even understaffing itself.
BUT STEPS CAN BE TAKEN TO ADDRESS THESE SHORTAGES.
The American Nurses Association’s Principles for Nurse Staffing, for example, guides hospitals and other decision-makers in developing the processes and policies needed to improve nurse staffing. Nursing workforce development programs are also essential to ensuring there are enough nurses to treat patients. The Title VIII Nursing Workforce Reauthorization Act, which has not been reauthorized by Congress, supports important workforce development programs, strengthens nursing education at all levels and provides funding to increase nurse practice in rural and underserved communities.
Mental health support is also important to overcoming nursing shortages. Hospitals should consider mentorship programs, longer orientation sessions and mental health support to help prepare and support nurses for their critical role in patient care. Adequate nurse staffing is vital for patient safety, the health care system and the well-being of nurses themselves.
Adopting policies that set standards for staffing guidelines, including nurses in creating staffing plans and supporting the mental health and mentorship of nurses will ensure patients receive safe, personalized and high-quality care.

PREEMIE FAMILY PARTNERS

Newborns, Hospitalization and PTSD
Premature babies can have a form of post-traumatic stress after staying in the neonatal intensive care unit (NICU).
By Ruchi Kaushik, MD, MPH-Medical Director, ComP-CaN (Comprehensive Peds for Complex Needs)-Medical Director, CHRISTUS Children’s Blog-Assistant Professor, Pediatrics, Baylor College of Medicine

*** June 27 is Post-traumatic Stress Disorder Awareness Day; PTSD is a mental health diagnosis that you have likely heard, particularly among the men and women who have served in the armed services.
But did you know that premature babies can have a form of post-traumatic stress after staying in the neonatal intensive care unit (NICU)? The trauma, or “early adverse experiences,” from a NICU stay can affect your premature baby’s health, development, and behavior.
Why is a NICU stay traumatic?
NICU stays can be traumatic for a variety of reasons:
Stimulation: Babies do not tolerate being overstimulated. Flashing lights, beeping monitors, constant alarms sounds in the NICU can cause a premature baby to suddenly pause in breathing and also result in frequent increases and decreases in heart rate, blood pressure, and oxygen levels.
Procedures: The procedures performed in the NICU are life-saving, but they do have consequences. In addition to having a tube placed in the airway to help a baby breathe, there are many procedures that cause pain such as placing an IV or undergoing surgery. These “skin-breaking” procedures can affect a baby’s normal development.
Separation from Mom: Although necessary, separating a premature baby from mom interferes with bonding and can affect the baby’s normal stress responses. This means that a premature baby’s response to stress may be excessive (prolonged crying, more severe separation anxiety, etc.) compared to that of a baby who was not premature and in the NICU.
What can I do to lessen the effects of this trauma?
The best studied technique to improve the impact of trauma on a premature baby in the NICU is skin-to-skin (or kangaroo) care. To perform skin-to-skin care, the baby is wearing only a diaper and is held upright on her belly against mom’s chest. Indeed, in animals, being sensitively touched soon after having been born results in less production of the body’s stress hormones (steroids).
Other methods to decrease stimulation include covering incubators with blankets to reduce light exposure, removing noisy equipment from the area if not necessary, and using sound-absorbing panels if they are available.
Although the NICU experience is necessary to help save a premature baby’s life, as a parent, you can do their part to lessen the effects of this trauma by being aware that this is a problem, providing skin-to-skin care as often as possible, and always responding quickly to your baby’s needs so your baby feels safe and secure with you once you go home.
Newborns Can Experience PTSD Following Hospitalization | CHRISTUS Health

Healing the Trauma of Premature Birth

Ira Hillman leads Einhorn Collaborative’s Bonding strategy. Learn more about our work in Bonding and more about Ira. Sign up to receive our monthly newsletter and be the first to read Ira’s blog posts.
My husband and I remember the phone call vividly.
“We were contacted by your son’s birth mother. She gave birth again and reached out to us about placing the child with an adoptive family. We told her that you were already working with us to adopt a second child, and she was happy to hear that this might work. The baby is a girl. She was born in July. At 26 weeks.”
Our jaws dropped. We knew nothing about premature birth other than that it wasn’t ideal. We soon found out that the baby girl who would become our daughter had actually been born at 28 weeks and 5 days. Her birth weight was 2.5 pounds.
The panic, fear, and anxiety we felt is what many families experience in association with the birth of their child. In fact, nearly 1 in 10 children each year in the US are born before 37 weeks gestation.
Since 2008, an alliance of health organizations from around the world has commemorated World Prematurity Day on November 17 in order to shine a light on preterm birth and support the families and communities affected by it.
Premature babies are often born with immediate health issues that require special care in a Neonatal Intensive Care Unit (NICU). They also face developmental challenges that lead to long-term neurological, mental, behavioral, and physical health risks, like cerebral palsy, asthma, and hearing or vision loss.
When babies are born, they need the nurturing relationships of parents and caregivers in order to thrive. But, because their fragile bodies need medical support, babies in the NICU are by necessity separated from their families. And it’s not just physical separation that gets between infants and parents; the sadness, fear, and guilt parents may be experiencing after a premature birth can make it even more challenging for them to provide nurturing care to their babies.
Family Nurture Intervention
All of these challenges can be addressed through a new approach to NICU care known as Family Nurture Intervention (FNI). Developed by the Nurture Science Program at Columbia University, FNI is a novel approach that centers emotional expression and the mother-child relationship.
The goal of FNI is to get a mother and baby connected so they can regulate each other’s bodies, in spite of the obstacles created by the NICU environment.
The approach, facilitated by a trained Nurture Specialist, involves a combination of sensory calming activities between the two while emotional communication happens. This means that while engaging in activities such as kangaroo care, eye contact, and scent cloth exchange (activities fairly common in the NICU), mothers are also encouraged to express their feelings to their babies.
When the mothers express their feelings – often in response to prompts like, “Tell your baby the story of your pregnancy and birth,” or “Tell your baby the story of how you chose their name” – they notice that their child’s attention turns to them, and they feel connected. The combined approach is not just about improving physiological outcomes, it is about building the kind of parent-child relationship that is crucial for lifelong health and wellbeing.
The feelings expressed by a mother of twin boys born at 26 weeks are similar to those felt by many parents, who often bear the burden of commuting an hour or more each way to visit their newborn children, in addition to the emotional trauma they have experienced.
“I didn’t feel like they were my babies because they were in the hospital, and I didn’t know if they were going to make it or not,” the mother of twins confessed.
Another mother of a girl born three months early said, “It took us months before I actually even saw her face, because she had so many tubes in. And when your baby is in that kind of situation, it’s almost like you can’t let your guard down to really bond with them. Because you’re scared of losing them.”
But, after experiencing Family Nurture Intervention, that same mother shared, “It’s like therapy for both of us. I’m telling you, that was the first time I felt like I could breathe, and I could bond with my baby.” And another mother agreed, “I actually come in now, and I can take a deep breath and be like, ‘I’m alright. And she’s alright.’”
Positive effects for babies and mothers
A clinical trial of FNI was conducted in the NICU at Columbia University with 150 preterm infants and their mothers, and it showed that they indeed are “alright.”
Compared to families who received standard care in the NICU, the babies who were part of FNI showed better sleep and improved brain development, particularly in the prefrontal cortex which is critical for executive function. They also showed better physiological regulation, which is an important marker of stress resilience.
At 18 months of age, those same children also scored better on measures of language, attention, and cognition, and had lower risks for behavioral and socio-emotional problems.
Importantly, given the dyadic nature of the intervention, there were benefits for the mothers as well, including reduced maternal depression and anxiety four months after giving birth, compared to mothers who did not receive the intervention, as well as healthier cardiac function.
The clinical trial is also the first NICU study to demonstrate long-term positive effects on both the mother and child; a recent follow-up study documents improved cardiac function and stress resilience, even five years later – for both the child and the mother.
My husband and I weren’t a part of this study. We weren’t even in the NICU or in contact with our daughter for the first two months of her life. But the lasting effects of FNI showed us that there’s no time limit on the healing power of nurture and emotional connection. Through emotional expression and mutual calming, we are moving through the developmental challenges that came from our daughter’s premature birth, together. On top of that, the emotional connection shared by each of us with her has helped all of us heal from the traumas of premature birth and its effects on our whole family.
Healing the Trauma of Premature Birth (einhorncollaborative.org)

PAYING FOR YOUR BABY”S NICU STAY

KEY POINTS
Contact your health insurance company to find out what medical costs are covered by your plan.
If your baby isn’t already on your insurance plan, call the company to add her.
If your insurance doesn’t cover all of your baby’s care, you may be able to apply for more insurance or financial aid.
How do you know what NICU costs are covered by your health insurance?
You may start getting bills for your baby’s stay in the newborn intensive care unit (also called NICU) while he’s still in the hospital. This may add to the stress that you’re already feeling about your baby’s health and care. Finding out what your insurance covers can help you manage your stress so you can focus on taking care of your baby.
Health insurance helps pay for medical care. You may get health insurance from your employer, or you may get it from the government or buy it on your own. Contact your insurance company to ask what costs are covered and what costs you need to pay. You can find the company’s phone number on your insurance card or on its website. If your baby’s not already on your plan, call the company to add her.
When you talk to a representative from your health insurance company, ask these questions:
• Does my plan pay for all of my baby’s medical expenses in the NICU?
• Are there services that the plan does not pay for?
• How do we pay the remaining cost?
Take notes when you talk to your health insurance representative. Write down the date of your calls and the names of the people you talk to. Many parents find it helpful to start a folder of letters and bills related to the cost of their baby’s medical care. Keeping everything together in one place can help you stay organized so you can focus on your baby’s care.
What if your health insurance doesn’t cover all of your baby’s care?
If your insurance doesn’t cover all services for your baby, ask the NICU social worker or case manager what to do. A social worker is a person who is trained to help families cope with their baby’s NICU stay. A social worker helps families find resources and services to help them care for their baby. A case manager is a person who may oversee a baby’s discharge from the hospital and help set up home-care services and supplies.
One or both of these staff can help you work with your insurance company and help plan for your baby’s transition home. They may suggest you apply for more insurance or financial aid, like Medicaid or the Supplemental Security Income Program (also called SSI) offered by Social Security. Your baby may qualify for SSI based on her medical need and your financial resources. For more information about SSI, call 800-772-1213. Having more insurance or financial aid may reduce the amount of money you pay for your baby’s medical bills.
If your insurance doesn’t cover all your bills, talk to someone from the hospital’s finance department about setting up a payment plan.
https://www.marchofdimes.org/find-support/topics/neonatal-intensive-care-unit-nicu/paying-your-babys-nicu-stayhttps://www.marchofdimes.org/find-support/topics/neonatal-intensive-care-unit-nicu/paying-your-babys-nicu-stay

INNOVATIONS

Children After Neonatal Patent Ductus Arteriosus

Front. Pediatr., 08 April 2020 Sec. Neonatology Volume 8 – 2020 | https://doi.org/10.3389/fped.2020.00150 Merete S. Engeseth1,2* Mette Engan2,3 Hege Clemm2,3 Maria Vollsæter2,3 Roy M. Nilsen1 Trond Markestad2 Thomas Halvorsen2,3 Ola D. Røksund1,3
Objective: To investigate voice characteristics and exercise related respiratory symptoms in extremely preterm born 11-year-old children, focusing particularly on associations with management of a patent ductus arteriosus (PDA).
Study design: Prospective follow-up of all children born in Norway during 1999–2000 at gestational age <28 weeks or with birthweight <1,000 g. Neonatal data were obtained prospectively on custom-made registration forms completed by neonatologists. Voice characteristics and exercise related respiratory symptoms were obtained at 11 years by parental questionnaires.
Result: Questionnaires were returned for 228/372 (61%) eligible children, of whom 137 had no history of PDA. PDA had been noted in 91 participants, of whom 36 had been treated conservatively, 21 with indomethacin, and 34 with surgery. Compared to the children treated with indomethacin or conservatively, the odds ratio (95% confidence interval) for the surgically treated children were 3.4 (1.3; 9.2) for having breathing problems during exercise, 16.9 (2.0; 143.0) for having a hoarse voice, 4.7 (1.3; 16.7) for a voice that breaks when shouting, 4.6 (1.1; 19.1) for a voice that disturbs singing, and 3.7 (1.1; 12.3) for problems shouting or speaking loudly. The significance of surgery per se was uncertain since the duration of mechanical ventilation was associated with the same outcomes.
Conclusion: Extremely preterm born children with a neonatal history of PDA surgery had more problems with voice and breathing during exercise in mid-childhood than those whose PDA had been handled otherwise. The study underlines the causal heterogeneity of exercise related respiratory symptoms in preterm born children.
https://www.frontiersin.org/articles/10.3389/fped.2020.00150/full
Genetic Discovery Reveals Who Can Benefit from Preterm Birth Therapy
UCSF researchers call for precision-medicine approach that could identify targets for novel treatments.
By Victoria Colliver January 24, 2024
A UC San Francisco-led study has for the first time identified genetic variants that predict whether a patient is likely to respond to treatment for preterm birth, a condition that affects 1 in 10 infants born in the United States.
The findings are critical because no medication is available in the U.S. to treat preterm birth. Last year, the Food and Drug Administration (FDA) pulled the only approved therapy to help reduce the likelihood of preterm births, citing ineffectiveness. The drug, a synthetic form of progesterone, was sold under the brand name Makena.
The new research found that pregnant individuals with high levels of mutations in certain genes — specifically those associated with involuntary muscle contraction — were less likely to respond to the treatment. Screening for the mutations could allow doctors to target Makena and other potential medications to those most likely to benefit, the authors suggest.
“This study calls for a precision framework for future drug development,” said the study’s senior author, Jingjing Li, PhD, associate professor in UCSF’s Department of Neurology and the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research. “In addition to understanding drug effects based on population averages, we also need to take into account the drug response of each individual patient and ask why some respond and some don’t.”
The study, which was done in collaboration with Stanford University, appears Jan. 19, 2024, in the journal Science Advances.
New genes associated with preterm birth
Preterm birth — babies born alive prior to 37 weeks of gestation instead of at the standard 40 weeks — is the leading cause of infant mortality and affects some 15 million pregnancies worldwide each year. Preterm birth also leads to a range of long-term health consequences including breathing problems, neurological impairments such as cerebral palsy, developmental disabilities, visual and hearing impairments, heart disease and other chronic illnesses.
To conduct the study, researchers developed a machine-learning framework to analyze genomes of 43,568 patients that had spontaneous preterm births. The approach uncovered genes that had not previously been known to be associated with preterm birth.
They examined mutations in the genes among those who had received the progesterone treatment Makena. The FDA approved the drug in 2011 after a single clinical trial but took it off the market last spring after concluding the drug didn’t work.
The decision left doctors without an approved medication to prevent preterm births and frustrated those who had found it effective for a subset of their patients. This posed the question: Could there be a genetic reason why progesterone therapy worked for some, but not for others?
The researchers discovered that patients in the group with low levels of mutations in the genes associated with muscle contractions were more likely to respond to Makena, but those with higher levels tended not to respond. About 19% patients in the study group had high mutation levels in those muscle genes, and none of those individuals responded to Makena.
The findings suggest a personalized medicine approach involving genetic screening could lead to successful results in patients without a high burden of those mutations.
“Progesterone therapy was the only treatment for recurrent preterm birth over the past decade, and its recent withdrawal by the FDA has left a void in the medication options available for preterm birth patients,” said the study’s first author, Cheng Wang, PhD, a postdoctoral scholar at UCSF.
“In previous clinical practice, we did see that many patients benefited from progesterone therapy,” Wang said. “We probably should reevaluate its efficacy, if we can identify those who respond positively to the treatment.”
The researchers included a cohort of African American patients in the study to determine whether the findings applied broadly across different races. Black women in the U.S. are almost twice as likely to give birth prematurely than white women.
They found the genetic burden did not vary by race. This suggests the high rate of preterm birth among Black mothers may be due primarily to environmental factors such as elevated stress hormones, health care biases and lack of prenatal care.
A new type of precision medicine
The researchers went beyond that finding to identify new targets and potential therapies to treat preterm birth by screening more than 4,000 compounds. They homed in on 10 predicted to interact with the genes associated with preterm birth.
Many of these therapeutic compounds are already being used to treat cancer and other diseases, which means that these drugs could possibly be repurposed to help prevent preterm labor. A top candidate is the small molecule RKI-1447, a drug that is currently being used to treat cancer, glaucoma and fatty liver disease. Additional study of the potential of these molecules in treating preterm birth is needed.

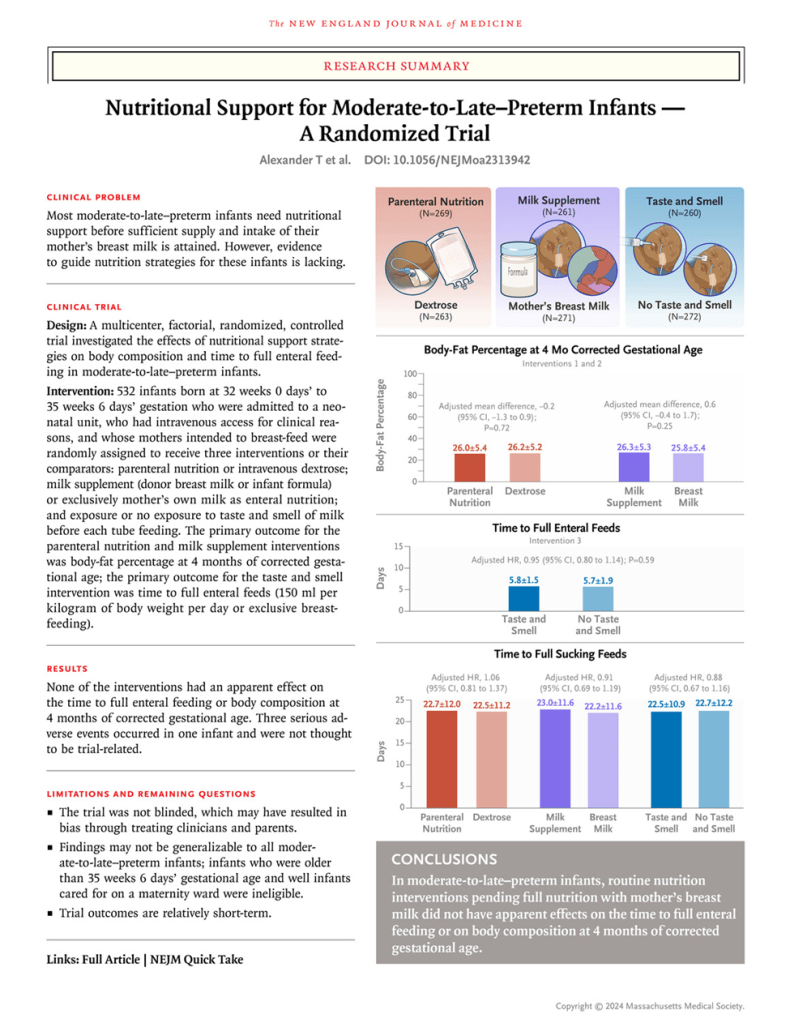
Nutritional Support for Moderate-to-Late–Preterm Infants — A Randomized Trial

Authors: Tanith Alexander, Ph.D., Sharin Asadi, Ph.D., Michael Meyer, M.D., Jane E. Harding, D.Phil., Yannan Jiang, Ph.D., Jane M. Alsweiler, Ph.D. https://orcid.org/0000-0002-0874-6654, Mariana Muelbert, Ph.D., and Frank H. Bloomfield, Ph.D. https://orcid.org/0000-0001-6424-6577, for the DIAMOND Trial Group – Published April 24, 2024
ABSTRACT
BACKGROUND
Most moderate-to-late–preterm infants need nutritional support until they are feeding exclusively on their mother’s breast milk. Evidence to guide nutrition strategies for these infants is lacking.
METHODS
We conducted a multicenter, factorial, randomized trial involving infants born at 32 weeks 0 days’ to 35 weeks 6 days’ gestation who had intravenous access and whose mothers intended to breast-feed. Each infant was assigned to three interventions or their comparators: intravenous amino acid solution (parenteral nutrition) or dextrose solution until full feeding with milk was established; milk supplement given when maternal milk was insufficient or mother’s breast milk exclusively with no supplementation; and taste and smell exposure before gastric-tube feeding or no taste and smell exposure. The primary outcome for the parenteral nutrition and the milk supplement interventions was the body-fat percentage at 4 months of corrected gestational age, and the primary outcome for the taste and smell intervention was the time to full enteral feeding (150 ml per kilogram of body weight per day or exclusive breast-feeding).
RESULTS
A total of 532 infants (291 boys [55%]) were included in the trial. The mean (±SD) body-fat percentage at 4 months was similar among the infants who received parenteral nutrition and those who received dextrose solution (26.0±5.4% vs. 26.2±5.2%; adjusted mean difference, −0.20; 95% confidence interval [CI], −1.32 to 0.92; P=0.72) and among the infants who received milk supplement and those who received mother’s breast milk exclusively (26.3±5.3% vs. 25.8±5.4%; adjusted mean difference, 0.65; 95% CI, −0.45 to 1.74; P=0.25). The time to full enteral feeding was similar among the infants who were exposed to taste and smell and those who were not (5.8±1.5 vs. 5.7±1.9 days; P=0.59). Secondary outcomes were similar across interventions. Serious adverse events occurred in one infant.
CONCLUSIONS
This trial of routine nutrition interventions to support moderate-to-late–preterm infants until full nutrition with mother’s breast milk was possible did not show any effects on the time to full enteral feeding or on body composition at 4 months of corrected gestational age. (Funded by the Health Research Council of New Zealand and others; DIAMOND Australian New Zealand Clinical Trials Registry number, ACTRN12616001199404.)
https://pubmed.ncbi.nlm.nih.gov/38657245/
https://pubmed.ncbi.nlm.nih.gov/38657245/

Tommy’s National Centre for Premature Birth Research Launch

Mar 19, 2024 Tommy’s
1 in 13 babies born in the UK are premature. Here at Tommy’s, we know more needs to be done to stop babies being born too soon. That’s why, we’re proud to announce the launch of our brand new National Centre for Preterm Birth Research today.


Preterm babies have a similar BMI at adolescence to peers born at term
By the time premature babies reach 14 to 19 years of age, they have, on average, a similar body mass index to peers born at term, according to an analysis of more than 250,000 people
By Jason Arunn Murugesu – 26 January 2023
People born prematurely are likely to have similar body mass indexes (BMIs) when they reach adolescence to people who were born at term.
To determine what effect the amount of time spent in the uterus has on a person’s body weight in childhood and adolescence, Johan Vinther at the University of Copenhagen in Denmark and his colleagues analysed data collected across 16 studies conducted in Europe, North America and Australia.
These studies included data on the gestation age of newborn children and follow-up data on their subsequent heights and weights over several years. A total of more than 250,000 children were included from across the studies, all born between 1985 and 2017.
Vinther and his colleagues took the height and weight data from each person and calculated their BMIs at various ages.
“Body size is a decent proxy for physical health,” says Vinther. “Though it’s not the only measure.”
The researchers found that while people born before 37 weeks of pregnancy, also known as preterm, were more likely to have a lower BMI in childhood than people born after 37 weeks, this difference disappeared between the ages of 14 and 19.
“Our study suggests that preterm individuals gain more weight in childhood, relatively, compared to people born at term,” says Vinther. It is unclear why, he adds.
The findings don’t necessarily mean children born preterm will always reach healthy body weights in adolescence, says Vinther. Other factors such as the BMI and education level of the mother will play a role, he says.
The results are based on people in high-income countries. “We don’t really know what this would look like in lower-income countries,” says Vinther. The team didn’t look at the specific effect of sex or ethnicity on the results.
Neena Modi at Imperial College London says the findings corroborate several long-running studies on this issue from across the world. However, recent work has shown that very preterm individuals are more likely to develop chronic conditions that are exacerbated by being overweight, she says.
“The critical health message is to ensure preterm individuals, and their parents and clinicians, are aware of the importance of maintaining a healthy body weight,” she says.


6 Daily Habits to Reduce Stress & Anxiety

At times, we can feel stress and anxiety reach new levels. You may have felt overwhelmingly stressed that you wouldn’t turn in an assignment on time, or you may have felt an abrupt feeling of anxiety wash over you as you walked over to a class podium for a presentation. Or perhaps your stress and anxiety seem constant and unrelenting. It may be difficult to do seemingly simple tasks all because you’re too overwhelmed by your anxious thoughts and stressful to-do list. Well, to help relieve some of your stress and anxiety, here are some daily habits that can reduce stress and anxiety.

Warrior Wisdom: Navigating Long-Term Outcomes and Managing Stress
Hello, Neonatal Womb Warriors!
This month, we’re focusing on a topic that hits close to home for many in our community: the long-term outcomes of preemie survivors and effective ways to manage anxiety and stress. Understanding these aspects is crucial for our continued growth and well-being.
As preemie survivors, we often carry the legacy of our early days in the NICU into adulthood. While we’ve overcome significant hurdles, the journey doesn’t end there. Many of us may experience ongoing health challenges such as respiratory issues, developmental delays, sensory processing disorders, anxiety, and PTSD.
Managing the stress and anxiety that can come with these long-term outcomes is equally important. Techniques such as mindfulness, meditation, spending time in nature, and engaging in physical exercise can serve as powerful tools to center/nourish our minds and bodies. Explore and find the activities that work best for you and incorporate them into your wellness routines.
Creating a supportive environment for and within yourself is KEY! Surround yourself with positive influences and nurturing relationships. Sharing experiences and coping strategies within our community can provide invaluable emotional support and practical advice. Online forums and local support groups can be great places to connect with others who truly understand our challenges and triumphs.
Lastly, don’t hesitate to seek professional help if you need it. Therapists and counselors who specialize in trauma and anxiety can offer tailored strategies to help you cope with your unique experiences. Sometimes, just having someone to talk to can make a significant difference in managing stress and fostering health.
We are incredibly strong and resilient. Let’s embrace our unique journeys and provide to ourselves the loving care we have long received from others.
Cheers!





Nov 26, 2021 nightyniteswithneli
Hi Friends! Welcome back to my channel! I’ve missed you guys so much! November is Prematurity Awareness Month so all month long we will be reading books by Preemie Authors, Parents, Siblings, and Healthcare workers who work with Preemies! On this episode of Nighty Nights with Miss Neli, we will be reading Faces of the NICU By: Shatoya Lewis & Latoya Lewis-Young Book Description: This book tells readers all about all of the different faces that work in the NICU with Preemie and NICU babies. Join Miss Neli as we learn about the different things they do!
Surfing in North Korea

Tiên Huyền Jun 17, 2017
DPRK’s East Sea is very clean, beautiful and pristine.



