


COMMUNITY
Austria, formally the Republic of Austria,] is a landlocked country in Central Europe, lying in the Eastern Alps. It is a federation of nine states, one of which is the capital, Vienna, the most populous city and state. Austria is bordered by Germany to the northwest, the Czech Republic to the north, Slovakia to the northeast, Hungary to the east, Slovenia and Italy to the south, and Switzerland and Liechtenstein to the west. The landlocked country occupies an area of 83,879 km2 (32,386 sq mi) and has a population of around 9 million.
The nation of Austria has a two-tier health care system in which virtually all individuals receive publicly funded care, but they also have the option to purchase supplementary private health insurance. Care involving private insurance plans (sometimes referred to as “comfort class” care) can include more flexible visiting hours and private rooms and doctors. Some individuals choose to completely pay for their care privately.
Healthcare in Austria is universal for residents of Austria as well as those from other EU countries. Students from an EU/EEA country or Switzerland with national health insurance in their home country can use the European Health Insurance Card. Self-insured students have to pay an insurance fee of EUR 52.68 per month.
Source: https://en.wikipedia.org/wiki/Austria
- GLOBAL PRETERM BIRTH RATES – Austria
- Estimated # of preterm births: 7.3 per 100 live births/Global Average: 10.6
- Source- WHO Preterm Birth Rate (Per 100 Live Births)
- World Population Review
Reflecting on the compelling needs of our preterm birth community and all communities worldwide, we turn our focus toward the greater good. As the dawn of a new year approaches, what will it bring? With hope and determination, we eagerly anticipate remarkable possibilities and transformative progress.
Kat and I are highlighting our healthcare provider community who is in need of international and regional support, our respect, our awareness of their challenges and strengths, and acknowledgement of their humanity. Without our diverse and competent health/medical provider community and their ancillary supportive partners there will continue to be a decline in our maternal and child health globally. The Covid pandemic accelerated the medical provider shortages that were already expanding globally when the pandemic hit.
Long story short: Our global healthcare provider community deserves our best intentions and actions. To deliver adequate—and especially life-saving—healthcare, we must prioritize developing, protecting, and supporting our healthcare provider family.
The World Health Organization (WHO) estimates that there is a global shortage of 4.3 million physicians, nurses, and other health professionals. The shortage is often starkest in developing nations due to the limited numbers and capacity of medical schools in these countries. Additionally, rural and remote areas also commonly struggle with a physician shortage the world over. While among the leading countries in the development of healthcare technology and medical research, the USA is a significant underachiever in providing health care access to the US population at large.
Infant mortality is the death of an infant before his or her first birthday. The infant mortality rate is an important marker of the overall health of a society. In 2022, the infant mortality rate in the United States was 5.6 deaths per 1,000 live births (https://www.cdc.gov/maternal-infant-health/infant-mortality/index.html). The infant mortality rate for Austria in 2022 was 2.476 deaths per 1000 live births.(Austria Infant Mortality Rates, 1950-2024)
In 2022, there were 22 maternal deaths for every 100,000 live births in the U.S. — more than double, sometimes triple, the rate for most other high-income countries in this analysis. In half of the countries, there were less than five maternal deaths per 100,000 live births (Commonwealth Fund,2024)
Each and every global citizen requires and deserves healthcare access to treatment and that includes the preterm birth community at large.
Addressing the Physician Shortage in the USA: A Call for Systemic Change
The United States faces a critical shortage of physicians, nurses, and other healthcare specialists. The medical doctor workforce is driven in large part by congressional limits on the number of medical residencies funded through Medicare. This artificial cap stifles the growth of our healthcare workforce, leaving millions underserved. One solution lies in embracing free-market principles and implementing reforms that prioritize the expansion of medical training opportunities.
Our healthcare providers are overworked and undervalued. The practice of requiring medical residents to endure 24-36 hour shifts is not only inhumane but also counterproductive to delivering safe and effective patient care. Requiring trauma surgeons and other medical providers to call insurance carriers to gain authorization for emergency treatment is ludicrous. Employment laws must evolve to respect the humanity of those we entrust with our health and lives. Healthcare professionals deserve fair treatment and work conditions that enable them to thrive, not just survive.
Moreover, the elitist funding structures of academic institutions perpetuate inequities, prioritizing financial privilege over talent and potential. It is imperative to create accessible pathways for aspiring doctors who possess not only the intellectual aptitude but also the emotional intelligence necessary for patient-centered care. These individuals often bring unique perspectives that can enhance the quality of healthcare delivery, especially in underserved communities.
To address the root causes of our physician shortage, we must scrutinize the financial and political forces influencing the system. By following the money, it becomes clear that vested interests have prioritized profits over people. Reforms rooted in free-market/supply and demand economic principles, coupled with a commitment to equity and sustainability, may help resolve the undersupply of medical practitioners and ensure a healthier future for all.
Cheers to all of you “BROAD” thinkers out there! Your passions are cherished. Best Regards and much love, Kathy and Kat

Mirror, Mirror 2024: A Portrait of the Failing U.S. Health System
Comparing Performance in 10 Nations
THE COMMONWEALTH FUND
David Blumenthal, Evan D. Gumas, Arnav Shah, Munira Z. Gunja, Reginald D. Williams II
Abstract
- Goal: Compare health system performance in 10 countries, including the United States, to glean insights for U.S. improvement.
- Methods: Analysis of 70 health system performance measures in five areas: access to care, care process, administrative efficiency, equity, and health outcomes.
- Key Findings: The top three countries are Australia, the Netherlands, and the United Kingdom, although differences in overall performance between most countries are relatively small. The only clear outlier is the U.S., where health system performance is dramatically lower.
- Conclusion: The U.S. continues to be in a class by itself in the underperformance of its health care sector. While the other nine countries differ in the details of their systems and in their performance on domains, unlike the U.S., they all have found a way to meet their residents’ most basic health care needs, including universal coverage.
Source: https://www.commonwealthfund.org/publications/fund-reports/2024/sep/mirror-mirror-2024

In Memory of Mildred T. Stahlman, MD
Joseph Philips, MD

Dr. Mildred T. Stahlman, known to all as Millie, died June 29, 2024, at 101 years of age. The attached biographic articles and obituaries detail much of her life and groundbreaking achievements. She was one of only four women in her medical class of 50 and was elected into AOA. Upon completing training, including a foundational time with John Lind at the Karolinska Institute in Stockholm, Sweden, she established herself at Vanderbilt University and created one of the first modern NICUs anywhere in the world. She made fundamental observations regarding respiratory physiology in the newborn, as detailed in the attached references . She was among the first to mechanically ventilate an infant with RDS, using a negative pressure ventilator as diagramed in reference 3. Back in the 1980s, we had one here at UAB that, I suppose, went to the warehouse and was never to be seen again. It was awkward to use, especially when one needed to enter it to do something with the baby, as one’s hands were repeatedly sucked in and out with each cycle of the machine.
Dr. Stahlman was among the early investigators who used neonatal lambs to study the physiology of the newborn. Millie also established one of the first regional neonatal transport systems in the US, pioneering the regionalization of neonatal intensive care. The first “Angel” transport vehicle was a converted old bread delivery truck, as pictured below. She was among the first to publish follow-up studies of former premature infants . The ethics of newborn intensive care was another of her interests, about which she wrote and spoke often . In her later years, she collaborated with Dr. Jeffrey Whitsett, with whom she published many seminal manuscripts on various aspects of lung development and surfactant biology. Together, they made additional groundbreaking discoveries regarding pulmonary surfactant and lung development.
Dr. Stahlman also trained and mentored numerous fellows and young faculty, many of whom pursued distinguished academic careers. She received both the Virginia Apgar Award from the American Academy of Pediatrics and the Howland Award, the highest award given by the American Pediatric Society in 1996, which she had previously served as President. She was elected into the Institute of Medicine for her groundbreaking scientific contributions, now officially known as the National Academy of Medicine. Dr. Stahlman’s multiple contributions to neonatology, neonatal biology, and physiology were truly profound and enduring.

A Call for Change: Fixing A Broken Medical Training System | Jake Goodman | TEDxUGA
May 22, 2023
Medical training practices in the United States haven’t changed much since formal residency programs were first introduced in 1897. A series of unaddressed problems within these practices have perpetuated mental health challenges within the medical profession. In this talk, Dr. Jake Goodman brings awareness and promotes advocacy to further the discussion on medical training improvements that are necessary to better protect the mental health and care of both physicians and patients. Jake Goodman is a Miami-based psychiatry resident physician. With more than 2.1 million followers, Dr. Goodman is a mental health activist and social media content creator focused on fighting stigma and discrimination while empowering those experiencing mental health challenges to seek help. This talk was given at a TEDx event using the TED conference format but independently organized by a local community.

Kaleen – What It Feels Like (Official Musicvideo)
Jul 6, 2023


Andrew & Kristyn Beam | Can AI Transform the NICU? | Delphi 2023
The Incubator Channel Oct 23, 2023
Kristyn Beam is a neonatologist at Beth Israel Deaconess Medical Center in Boston, MA. She is also an Instructor at Harvard Medical School. Her research interests are aimed at investigating how machine learning and artificial intelligence can utilize large data sources in the neonatal intensive care unit to create new prediction models and ultimately improve neonatal outcomes. She is joined on stage by her husband and fellow researcher Dr. Andrew Beam, an assistant professor in the Department of Epidemiology at the Harvard T.H. Chan School of Public Health who also studies the clinical applications of machine learning.


Supporting a Family After the Death of a Child or Adolescent
11/27/23

A child’s death, whether from illness or sudden loss, is always traumatic and stressful, and those affected may grieve in different ways.
The pediatrician can play a critical role in helping families, caregivers and the child’s community navigate the loss of a child, according to an updated clinical report published by the American Academy of Pediatrics.
The report, “Supporting the Family After the Death of a Child or Adolescent,” published in the December 2023 Pediatrics, draws on the latest evidence on grief, bereavement and mourning on ways to provide support and practical information.
How pediatricians can help a grieving family
“A pediatrician can provide comfort, compassion and a listening ear. They can also offer practical information, like where to find a community bereavement program or grief counseling,” said Meaghann S. Weaver, MD, PhD, MPH, FAAP, lead author of the report.
“If there are siblings, each child may process grief in their own way, based on their age and maturity level. There are no easy paths through the grieving process. But having support from a variety of places, including the medical provider, is critical.”
The AAP Committee on Psychosocial Aspects of Child and Family Health and the Section on Hospice and Palliative Medicine wrote the clinical report, which replaces a 2016 report, noting that families cannot be expected to “move on” or “get over” the death of a child.
“The grief process is unpredictable. It does not unfold in a straight line. Emotions may wax or wane from one day to another,” said Arwa Nasir, MBBS, MSc, MPH, FAAP.
“After families absorb the inevitable shock of the death, they may move into
new phases of their grief,” Dr. Nasir said. “We can encourage family members to be gentle with each other as they adjust to their loss and the impact on their lives.”
The most common causes of death in children
The report breaks down the most common causes of death in children. It shows how the COVID-19 pandemic revealed the vulnerability of even pediatric patients. By March 2022, approximately 355 children ages 4 and below and 737 ages 5 through 18 died from a COVID infection and related causes in the United States.
Although American Indian/Alaska Native, Black, and Hispanic children represent 41% of the US population under age 20, they accounted for 78% of COVID-19-related deaths in this age cohort, according to research cited.
Sudden and unexpected infant deaths, including SIDS, accidental suffocation deaths, and ill-defined deaths represent 3,400 deaths per year in the United States and are the largest category of sudden and unexpected deaths in childhood.
Motor vehicle crashes were cited as the leading cause of pediatric deaths for over half a century. Beginning in 2017, firearms now represent the number one cause of death among persons ages 1 to 19 years old.
AAP’s recommendations for pediatricians include:
- Respect that compassion is a universal language of care and can be expressed through taking the time to listen and provide emotional support to a family.
- Realize how knowledge about the structure of a family and its support systems may be important in recognizing each family’s unique needs.
- Consult with sources and family to learn about the cultural and religious traditions surrounding death and bereavement to include culturally appropriate parental roles of grieving.
- Pediatricians should consider visiting their seriously ill or dying patients in the emergency department or pediatric intensive care unit, as able. Consider a phone call or face-to-face meeting with the child’s caregiver.
- Follow-up with and provide guidance to surviving siblings who are still patients.
“It’s important to understand that grieving the loss of a child is longer than many expect,” Dr. Weaver said. “Families often hold a cherished, forever connection to the child.”
More information
- Coping With a Child’s Death: AAP Policy Explained
- Source:https://www.healthychildren.org/English/news/Pages/supporting-a-family-after-the-death-of-a-child-or-adolescent.aspx

HEALTHCARE PARTNERS

The Effect of Swaddling and Oropharyngeal Colostrum During Endotracheal Suctioning on Procedural Pain and Comfort in Premature Neonates
A Randomized Controlled Trial

Karadede, Huriye MSc, RN, Lecturer; Mutlu, Birsen PhD, RN Editor(s): Dowling, Donna PhD, RN; Newberry, Desi M. DNP, NNP-BC; Parker, Leslie PhD, APRN, FAAN, Section Editors
Abstract
Background:
Endotracheal suctioning (ES) is a painful procedure frequently performed in the neonatal intensive care unit. This procedure negatively affects the comfort level of premature neonates.
Purpose:
To determine the effect of 2 nonpharmacologic methods, swaddling and the administration of oropharyngeal colostrum, on the pain and comfort levels of preterm neonates during ES.
Methods:
This randomized controlled experimental study comprised 48 intubated premature neonates (swaddling group n = 16; oropharyngeal colostrum group n = 16; and control group n = 16) at 26 to 37 weeks of gestation. The neonates were swaddled with a white soft cotton cloth or administered 0.4 mL of oropharyngeal colostrum 2 minutes before ES, according to the group in which they were included. Two observers evaluated the pain levels (Premature Infant Pain Profile-Revize [PIPP-R]) and comfort (Newborn Comfort Behavior Scale [COMFORTneo]) of the infants by observing video recordings of before, during, and after the procedure.
Findings/Results:
A significantly lower mean PIPP-R score was found in the swaddling group during ES compared with the control group (P = .002). The mean COMFORTneo scores of the swaddling and oropharyngeal colostrum groups during ES (P < .01, P = .002) and the mean PIPP-R and COMFORTneo scores immediately after ES and 5, 10, and 15 minutes later were significantly lower than the control group (P < .005).
Implications for Practice and Research:
Swaddling was effective both during and after the procedure, while oropharyngeal colostrum was effective only after the procedure in reducing ES-related pain in premature neonates. Swaddling and oropharyngeal colostrum were effective in increasing comfort both during and after the procedure.

The knowledge, attitude and behavior on the palliative care among neonatal nurses: what can we do
Yilan Yan1†, Jiahui Hu1†, Fei Hu1† and Longyan Wu1
BMC Palliative Care
Abstract
Background
Neonatal nurses should provide timely and high-quality palliative care whenever necessary. It’s necessary to investigate the knowledge, attitude and behavior of palliative care among neonatal nurses, to provide references and evidences for clinical palliative care.
Methods
Neonatal intensive care unit (NICU) nurses in a tertiary hospital of China were selected from December 1 to 16, 2022. The palliative care knowledge, attitude and behavior questionnaire was used to evaluate the current situation of palliative nursing knowledge, attitude and behavior of NICU nurses. Univariate analysis and multivariate logistic regression analysis were used to analyze the influencing factors.
Results 122 nurses were finally included. The average score of knowledge in neonatal nurses was 7.68±2.93, the average score of attitude was 26.24±7.11, the score of behavior was 40.55±8.98, the average total score was 74.03±10.17. Spearman correlation indicated that score of knowledge, attitude and behavior of palliative care in neonatal nurses were correlated with the age(r=0.541), year of work experience(r=0.622) and professional ranks and titles(r=0.576) (all P<0.05).
Public contribution
NICU nurses have a positive attitude towards palliative care, but the practical behavior of palliative care is less and lack of relevant knowledge. Targeted training should be carried out combined with the current situation of knowledge, attitude and practice of NICU nurses to improve the palliative care ability and quality of NICU nurses.
Source:https://link.springer.com/content/pdf/10.1186/s12904-024-01470-y.pdf

Dr. Fumihiko Namba, MD | Care of Extremely Preterm Infants in Japan
Sep 11, 2023 The Incubator Channel
Dr. Namba is an Associate Professor of Pediatrics at Saitama Medical Center, Saitama Medical University, one of the largest NICUs in Japan. He is an active researcher in the field of BPD, PDA and ROP. At Delphi this year, Dr. Namba shared with us the unique approach of our Japanese colleagues toward caring for extremely low birth weight infants in the neonatal intensive care unit. From management in the delivery room to day-to-day care in the NICU. This approach is at the root of the impressive outcomes of ELBW infants born in Japan. We are so proud to bring you this amazing talk.

Strategies to recognize and mitigate mistreatment of medical students
Jonnae Atkinson Lizzeth Alarcon Emilio Blair David Chartash Chantel Clark Amy Clithero-Eridon Adrian George
Shira Goldstein Joseph Luzarraga Rebecca Cantone
DOI: 10.62694/efh.2024.128Sun, 08 Sep 2024 in Education for Health

Abstract
Mistreatment of learners in medical education is a significant problem affecting more than half of all trainees worldwide. This mistreatment can lead to severe consequences, including burnout, post-traumatic stress disorder symptoms, substance misuse, and decreased self-esteem, impacting not only future physicians but also the broader educational community. Despite increased awareness of such harms associated with mistreating medical learners, these behaviors have continued to persist over the years. We aim to equip medical educators and learners with practical strategies to recognize and mitigate mistreatment in the educational setting. We offer examples and concrete advice to help educators and institutional leaders classify mistreatment, navigate various scenarios, and create optimal reporting structures. Additionally, we provide recommendations for dismantling toxic environments and enhancing reporting transparency to build learner trust. Addressing mistreatment will require multifaceted collaboration between learners, educators, and institutions. This advice will help foster a shared commitment to establishing a culture of respect and support among all in the medical learning environment.
INTRODUCTION
A comprehensive view of medical education from the perspectives of educators, anthropologists, and trainees reveals that professional identity formation and clinical training are often overshadowed by a facade of mistreatment. As physicians training the next generation, it is crucial to avoid perpetuating cycles of mistreatment or harmful student learning experiences in pursuit of our goal of training the most competent physicians.
This article offers practical advice for medical school educators, leaders, and other health professionals to recognize, address, and dismantle mistreatment in educational settings. We also provide strategies to improve reporting and foster a healthy learning environment. Key advice is bolded, and scenarios are italicized to illustrate situations experienced by our student authors.
Classify the Mistreatment Type
The first step in addressing mistreatment is to classify the type. Is the occurrence discrimination, harassment, or general mistreatment? Each of these issues can be investigated at the institutional level. However, discrimination and harassment may have legal protections and implications at a higher level.
On inpatient rounds during a family medicine sub-internship, a third-year medical student is assigned a patient who presents to the ED with acute pancreatitis. The student prepares to admit the patient to the floor with a resident on the team. The student makes errors when attempting to calculate the rate of IV fluids. The resident smiles and says, “I would have expected someone like you to be good at math.”
This scenario could be mistreatment or discrimination, depending on the context. To begin, review definitions of mistreatment relevant to your context. In the U.S., The AAMC defines mistreatment as, “intentional or unintentional behavior that disrespects the dignity of others and unreasonably interferes with the learning process.” Reference your institutional code of conduct for guidance. Mistreatment should be assessed if the behavior unreasonably interfered with the learning process. To help make this judgment, ask the reporter to share how they would classify the event.
Address Toxic Environments that Allow for Mistreatment
Worldwide, more than half of all medical trainees experience mistreatment and harassment.4 Mistreatment in medical students can lead to burnout, post-traumatic stress disorder symptoms, substance misuse, and decreased self-esteem. This issue extends beyond future physicians. Therefore, advocating for safe learning environments for all medical learners is essential. Beyond the direct harm to students, a learning environment filled with mistreatment can degrade the quality of education, affecting instruction, assessment, and overall learning.
The family medicine inpatient team student is admitting a patient with chest pain. After presenting to the team, the plan is to consult cardiology. The student calls the cardiology fellow to discuss the consult. When the student cannot answer a question posed by the cardiology fellow, the fellow becomes upset and says on the phone, “You clearly have not read this patient’s chart, and you do not know this patient. Tell your resident to call me to discuss this consult” and hangs up. The resident is seeing another patient, and only the attending is around.
Encourage reporting in a safe environment to address individual incidents and to empower students to dismantle toxic environments in their future workplaces. In order of severity, a step-wise approach to addressing mistreatment begins with providing direct feedback to the perpetrator. Inform them of the allegations, solicit their viewpoints, review policies if warranted, provide constructive criticism, and create an individual improvement plan. If an entire cohort has engaged in inappropriate behavior, conduct a group feedback and teaching session.
If the transgression is severe or there is a pattern of poor behavior, it may be necessary to separate the parties involved by removing the teacher from the learner, or vice versa. The most extreme response involves escalating the issue to human resources to place the transgressor on administrative leave or to terminate employment. It is important to set realistic expectations for potential outcomes for both parties. Consequences should be fair and consistent, and a step-wise approach should be used to resolve the issue. Keep the outcome confidential to avoid exacerbating psychological harm to the person who reported the incident. The resolution of the incident should not be constructed solely by either party. Instead, a consensus-driven conclusion should be reached as part of a comprehensive process.
Recognize Public Embarrassment as a Form of Mistreatment
A team finishes long rounds and wants coffee together before the next admission. They ask the student to pick up the coffee because everyone else on the team has ‘real responsibilities.’
Minimizing a student’s role on the healthcare team interferes with their education, causing them to question their place in the profession. Imposter syndrome, a relatively well-recognized phenomenon, occurs when highly successful individuals attribute their success to external factors, such as luck or knowing the right people. These feelings can lead to a decrease in self-confidence and may escalate to substance abuse, depression, and suicidal ideation.
Recognize that Students Experience Mistreatment by Patients
A third-year medical student sees an ambulatory family medicine patient individually, and the patient comments, “I don’t want to talk to you. I don’t trust medical students, especially students who look like you.” The student then tells the faculty, and the faculty sees the patient independently without debriefing with the student or discussing more with the patient.
Mistreatment of healthcare professionals by patients is a notable problem. Students may be at increased risk for mistreatment by patients because of their training status and exposure to patients in various clinical settings. Fnais et al. examined harassment and discrimination in medical training in studies performed in multiple countries. They found discrimination was most prevalent based on gender, ethnicity, and race. Additionally, they found that patients and their families constitute the second most common source of harassment and discrimination toward medical trainees.
Despite awareness of reporting processes for mistreatment, students often refrain from reporting due to practical or ethical concerns. Students wonder whether reporting will significantly change patient behavior or impact their grades. Data suggest that trainees who experience mistreatment report increased anxiety, avoidance of specific patient types, and, in some cases, reconsideration of their career choices or practice locations.
To effectively address the mistreatment by patients towards healthcare trainees, it is crucial to implement policies that specifically address such incidents and provide guidelines for handling patient accommodation requests. Equally important is the training of faculty and staff to support and debrief students who encounter mistreatment from patients. Integrating mixed curricula featuring case-based scenarios, often in video format, can educate faculty, staff, and trainees on recognizing and responding to mistreatment. Workshops structured for discussion and role-playing offer practical, real-time experience managing mistreatment incidents. Faculty development may also emphasize appropriate patient screening practices to prevent placing students in challenging situations without adequate support.
Recognize the Effect of Reporting on Faculty
Assuming the majority, if not all, medical educators approach their teaching responsibilities with good intent and enthusiasm, it can be surprising, demoralizing, and anxiety-inducing for an educator to learn they are the subject of a student mistreatment report. Once a medical educator is notified about their involvement in a report, several steps can be taken to facilitate a positive outcome. Initially, scheduling a prompt meeting can address immediate faculty concerns, alleviate anxiety, and assess the educator’s emotional state. The meeting can also define outcome goals and structure ongoing communication to monitor progress toward achieving goals. Pairing the educator with a colleague in the department for regular check-ins can provide additional support and mentorship to enhance the probability of a successful outcome. Recognizing and affirming the faculty’s commitment to becoming a better educator upon achievement of their goals is essential. It is important for medical educators to understand that how they respond to student mistreatment and complaints can underscore their ability to accept constructive feedback, effectively handle criticism, and demonstrate a growth mindset, all qualities valued in successful teachers, and learners.
Value the Role of the Graduate Medical Learner
Postgraduate trainees (e.g., junior doctors, house officers, interns, registrars, and residents) play a significant role in the education of medical students. They are closer in age to medical students and thus often serve as role models for student behavior. Therefore, training this cohort to become better teachers is crucial to optimizing the student learning experience. For example, properly equipping them with skills such as giving and receiving feedback can significantly enhance the learning environment.
Additionally, as integral members of the educational team and clinical environment, postgraduate learners must understand the processes for reporting mistreatment and discrimination at their institution, and their responsibilities as witnesses or involved parties. Ensuring that postgraduate trainees are well-informed and engaged in these processes can positively influence the culture of the learning environment.
Ensure Follow-up is Complete
Ensure a proper procedure is in place for comprehensive follow-up after an incident of mistreatment. A follow-up protocol that concludes the process will help the mistreated party feel heard and ensure their incident was addressed. Put measures in place to protect the mistreated party and the accused from retaliation. The integrity and character of all parties should be safeguarded throughout the reporting process. While reporting may be anonymous, essential details about the incident should be included to ensure a thorough understanding of the situation.
Transparency is also critical. Informing the students of the outcome can empower them to speak up if they experience or witness inappropriate behavior. Additionally, de-identified and broad reports should be shared with student groups, faculty, and leadership. Reporting can drive cultural change within the profession by validating student experiences and reinforcing that certain behaviors are unacceptable. Without reporting, students may become disengaged and disillusioned and perpetuate negative behaviors.
CONCLUSION
Finally, don’t wait for incidents to be reported. Take a proactive approach to prevent student mistreatment. Strategies include creating a positive working environment with uplifting visuals in the workspace, and conducting simulations to train individuals—including bystanders—on proper responses to various mistreatment scenarios. Providing new students, faculty, and staff with an overview of policies related to student mistreatment and reporting can promote a culture of awareness, recognition, and intervention. Creating spaces for critical reflection allows students and faculty to discuss recent challenges, brainstorm helpful strategies, and identify growth areas.
Emphasize building a culture of solutions rather than focusing on problems. Training and policies alone are insufficient, without a culture of proactive engagement, to ensure a shared language and understanding of the desired outcomes related to delivering quality medical education in a respectful and safe environment.
Education for Health disseminates work consistent with the mission of The Network: Towards Unity for Health (TUFH), a global consortium of health professions schools and individuals committed to improving education of the health workforce and focused on responsiveness to the needs of communities they serve.
Source:https://educationforhealthjournal.org/index.php/efh/article/view/128/134

PREEMIE FAMILY PARTNERS

Episode 50: The NICU View: Mom & Baby (Part 1)

Jul 31, 2024 #pediatrics #kidshealth #health
We begin our four-part series “Hot Topics in Neonatology” with the story of author and preemie family advocate Deb Discenza. Deb was 30 weeks pregnant when she gave birth to her daughter, Becky. In this episode, she shares their NICU story of persistence and resilience, and how she is paying it forward by helping and supporting other pregnant people and their pre-term babies. Guest: Deb Discenza, Founder & Executive Director, PreemieWorld Foundation Inc. Producer, Host: Carol Vassar

Surgeon General Advisory is Clear: Parents are Languishing Under Unprecedented Pressure

Nearly half of parents say they are “completely overwhelmed” by raising kids most days, with four in 10 reporting that the stress keeps them from functioning. These statistics paint the bleak picture of parenting today as delineated in “Parents Under Pressure,” a recent advisory from U.S. Surgeon General Vivek H. Murthy.
Many Concerns for Modern Parent:
Parents’ pressure has risen steadily over the past decade, with a spike during COVID-era lockdowns. Even though that period has passed, the general state of overwhelm shows no sign of receding. Parental stress now qualifies as a public health issue, according to the advisory.
Almost three-quarters of parents say parenting is more difficult now than 20 years ago. Constant scrutiny from other parents, primarily via social media, contributes to parents’ mental health struggles. Other top stressors include economic instability, job pressures, long to-do lists and too little time, difficulty managing their kids’ exposure to technology, and social isolation.
Personal Mental Health Among Parents’ Worries:
While parents are juggling the stressors of the role, many are also concerned about how best to manage their mental health challenges. Almost a quarter of parents had a documented mental illness, and a quarter of those were classified as “serious.” Parents of children with special health care needs were especially likely to report “fair or poor mental health.” Nearly one in five children under 17 have such needs.
A Multifaceted Solution
However, the outlook does not have to be as forbidding.
“We can do better,” according to Murthy, who recalled his “moments of feeling lost and exhausted.” Calling attention to the stress and mental health concerns facing parents and caregivers allows for the opportunity to “lay out what we can do to address them.”
Individual efforts to reduce parental stress and prioritize mental health can offer some relief, including building relationships with parenting peers, getting enough sleep, making time for self-care, and exercising regularly. However, broader policy changes have the potential to impact more parents positively. Increased paid parental leave and endorsing flexible work schedules, along with reduced taxes for families with children and more affordable childcare alternatives, are all mentioned in the report.
The report also includes a section that outlines opportunities for government to contribute to solutions. Recommendations include:
- Promoting and expanding funding for programs that support parents and caregivers
- Establishing a national paid family and medical leave program
- Addressing the barriers that contribute to the disproportionate impact of mental health conditions for certain parents and caregivers
- Ensuring parents and caregivers have access to mental health care
It is likely to take contributions from governments, employers, communities, and schools to reduce parenting stress in America. Allowing it to remain unchecked harms the parents, their kids, and society.

Tips to Support you Dad, in the NICU
Canadian Preemies
CANADIAN PREMATURE BABIES FOUNDATION official channel. Videos, LIVE education sessions (Preemie Chats), and presentations for NICU families, researchers and health care professionals. Learn more about the Canadian Premature Babies Foundation at our website: http://www.canadianpreemies.org.

*** Wonderful Resources For Providers and Families Experiencing Loss

INHA
The INHA is Ireland’s first collaborative platform and network to represent the interests of preterm infants, ill infants in the Neonatal Intensive Care Units (NICU) and their families.

Booklets
Source: https://inha.ie/resources-for-bereaved-parents/ https://inha.ie/resources-for-staff/

INNOVATIONS

Parental attitudes and perceptions towards the recruitment of children to clinical trials: a cross-sectional survey
Front. Pediatr., 12 November 2024 Front. Pediatr., 12 November 2024
Ibrahim Farhan Safra1Shaikha Jabor Alnaimi2*Gehad Gad3Aliamma Abraham1Ahmad Hassan Al-Hammadi4Mohammad A. A. Bayoumi1*Fawziya Alyafai5Ashraf Gad1
Background: Clinical trials (CTs) in children are critical for understanding and treating childhood diseases. However, there trials require prior permission from parents. We evaluated parental attitudes and perceptions regarding the recruitment of their children in CTs.
Methods: We used a cross-sectional survey questionnaire targeting parents of children admitted to the neonatal and pediatric departments in two tertiary hospitals in Qatar. The survey was administered by investigators and was composed of two domains to assess the knowledge and attitude of parents regarding children’s enrollment in CTs, in addition to the participant’s demographics domain.
Results: Of the 167 questionnaires offered to parents, we received a total of 138 responses, resulting in a response rate of 82.6%, with the majority being women (72%). Many parents (75%) expressed willingness to enroll their children in CTs. However, 66% opposed new experimental treatments for their child, while 41% agreed to new treatments if they had previously been used in the medical field. Logistic regression analysis revealed key predictors influencing parents’ decisions to include their children in CTs, including having a newborn (aOR = 17.651, p < 0.001), families with five or more members (aOR = 3.293, p = 0.012), collecting blood samples (aOR = 8.602, p = 0.003), performing additional tests on collected samples (aOR = 4.115, p = 0.046), belief in helping others (aOR = 8.744, p = 0.002), and the option of home therapy (aOR = 7.090, p = 0.004).
Conclusion: Many parents are open to enrolling their children in CTs, particularly when treatments have been previously used. Factors like having a newborn, large family size, blood collection, additional tests, and home therapy influence their decisions. Clear communication can enhance recruitment in pediatric trials.
This concept holds strong potential, as it fosters meaningful engagement that could significantly enhance parent/caregiver confidence and improve baby health outcomes. When effectively implemented, it may also contribute to a measurable reduction in hospital revisits and emergency department visits, benefiting parents, babies, and medical providers alike.
Source:https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2024.1490274/full
Advancing child health and pediatric specialty care through clinical discovery, multidisciplinary research and innovation
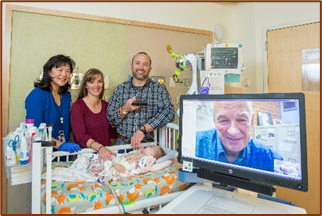
Telehealth Handoffs Help Ensure Smooth Transition of Care
4/18/2024

Neonatologist Jeanne Zenge, MD, facilitates a telehealth handoff to an infant’s pediatrician as part of the NICU discharge process.
Key takeaways
- Medically complex infants face a higher risk of readmission after neonatal intensive care unit (NICU) discharge, yet their discharge summaries are often incomplete or lack important details.
- In this case series, a multi-institutional collaboration sought to enhance NICU discharge communication and improve transition of care from the neonatologist to the pediatrician using telehealth handoffs.
- Telehealth handoffs provide an opportunity for the neonatal provider, pediatrician, family and relevant subspecialists to share information and ask questions.
- Scenarios where telehealth handoffs have been valuable include assisting with post-discharge care plan changes, demonstrating unique physical findings, making additional subspecialists available and coordinating care across long distances.
- While this approach is relatively easy to implement, more research is needed to evaluate the impact of telehealth handoffs on outcomes and patient and caregiver experiences.
Research study background
Infants discharged home from a neonatal intensive care unit (NICU) may face elevated risks due to factors such as prematurity, lingering medical issues, dependence on technology, and challenges within the family dynamic. These risks can lead to acute emergency department visits and hospital readmissions.
The transition of care from the neonatologist to the primary care provider typically relies on written summaries or phone handoffs, but recent surveys reveal pediatricians’ dissatisfaction due to incompleteness and lack of critical health details. Traditional methods may fail to convey unique findings and hinder discussions on post-discharge health issues, posing challenges for coordinated care.
Children’s Hospital Colorado was among three institutions collaborating on this case study as part of the Supporting Pediatric Research Outcomes Utilizing Telehealth (SPROUT) initiative. The project’s objective was to enhance discharge communication and hospital handoffs between neonatologists and PCPs using telehealth. This case series highlights four scenarios illustrating the benefits of this approach.
Case 1: Support for change in care plans after NICU discharge
Telehealth handoff coordination optimized home oxygen for a medically complex infant. Remote adjustments by PCP, neonatologist and pulmonologist averted readmission and improved oxygen saturation levels. The pulmonologist expedited follow-up and increased oxygen deliveries, ensuring the infant’s stability at home.
Case 2: Demonstration of physical findings
Telehealth handoff facilitated communication among the neonatologist, mother, pediatric surgery nurse practitioner (NP) and PCP for an infant with a large omphalocele and post-surgical epithelialization. This ensured a clear understanding of anomaly size, wound status and care instructions for an uncommon diagnosis. The NP provided guidance on when the PCP should contact pediatric surgery for timely intervention.
Case 3: Incorporation of additional subspecialties
A late preterm infant diagnosed with Hurler’s disease was treated for mild cardiomyopathy, weaned to low-flow oxygen and discharged from a level IV NICU. A telehealth handoff including the family clarified unique findings and disease complexities, empowering the PCP to coordinate timely enzyme replacements with insights from the NICU provider and metabolic consultant.
Case 4: Care coordination for remote patients
An infant born in a small rural mountain town was transferred to a level IV NICU for diaphragmatic repair. A handoff at discharge involving the NICU provider, surgical PA and family helped familiarize a new PCP with the infant’s mild tachypnea and clarified home oxygen delivery across state lines. The PA and PCP also discussed using telehealth to prevent an 11-hour drive for surgical follow-up.
Relevance to practice
Study authors noted that telehealth handoffs are relatively easy to implement. They underscored the need for more research to gather objective data on the provider and caregiver experience and how this approach can impact safety, health outcomes and quality of care.
Read the entire study Published in the March 2023 of Telemedicine and e-Health

New technology allows parents more access to babies in NICU care

Jul 9, 2024 InvestigateTV
This hospital shows us how new technology allows some families to feel close to their newborns even when they’re miles away.


Epigenetics Embedding of Oral Feeding Skill Development in Preterm Infants
A Study Protocol
Griffith, Thao PhD, RN; White-Traut, Rosemary PhD, RN, FAAN; Tell, Dina PhD; Green, Stefan J. PhD; Janusek, Linda PhD, RN, FAAN Editor(s): Dowling, Donna PhD, RN; Newberry, Desi M. DNP, NNP-BC; Parker, Leslie PhD, APRN, FAAN, Section Editors
Abstract
Background:
Preterm infants face challenges to feed orally, which may lead to failure to thrive. Oral feeding skill development requires intact neurobehaviors. Early life stress results in DNA methylation of NR3C1 and HSD11B2, which may disrupt neurobehaviors. Yet, the extent to which early life stress impairs oral feeding skill development and the biomechanism whereby this occurs remains unknown. Our team is conducting an NIH funded study (K23NR019847, 2022-2024) to address this knowledge gap.
Purpose:
To describe an ongoing study protocol to determine the extent to which early life stress, reflected by DNA methylation of NR3C1 and HSD11B2 promoter regions, compromises oral feeding skill development.
Methods:
This protocol employs a longitudinal prospective cohort study. Preterm infants born between 26 and 34 weeks gestational age have been enrolled. We evaluate early life stress, DNA methylation, cortisol reactivity, neurobehaviors, and oral feeding skill development during neonatal intensive care unit hospitalization and at 2-week post-discharge.
Results:
To date, we have enrolled 70 infants. We have completed the data collection. Currently, we are in the data analysis phase of the study, and expect to disseminate the findings in 2025.
Implications for Practice and Research:
The findings from this study will serve as a foundation for future clinical and scientific inquiries that support oral feeding and nutrition, reduce post-discharge feeding difficulties and lifelong risk of maladaptive feeding behaviors and poor health outcomes. Findings from this study will also provide further support for the implementation of interventions to minimize stress in the vulnerable preterm infant population.


From Preemie to Survivor

I’ve got something truly special for you in our latest episode. I sat down with the remarkable Christina Gagnon, a warrior who entered this world as a preemie with the odds stacked against her. Weighing just 1 pound and 8 ounces at birth, Christina’s resilience is nothing short of miraculous.



KIDS BOOK READ ALOUD ~ Splat the Cat Goes to the Doctor ~ Read Aloud ~ Doctors
Sometimes going to the doctor can be scary! Join Splat the Cat on his first visit to the doctor to see that it’s not so bad after all! Please like and subscribe!

SURFING ON SALZACH RIVER AUSTRIA RIVERSURF EXPERIENCE

Christian Strasser – Mar 2, 2016
When the glaciers send their ice cold waters down the river Salzach in Salzburg, Austria, its high time for the riversurfers to ride the natural wave crests in Kuchl between stone blocks. Watch the masters of the alpine ocean waves challenging the standing wave in the riverbreak of the European alps!

