Guyana, officially the Co-operative Republic of Guyana, is a country on the northern coast of South America, part of the historic British West Indies. Georgetown is the capital of Guyana and is also the country’s largest city. Guyana is bordered by the Atlantic Ocean to the north, Brazil to the south and southwest, Venezuela to the west, and Suriname to the east. With a land area of 214,969 km2 (83,000 sq mi), Guyana is the third-smallest sovereign state by area in mainland South America after Uruguay and Suriname, and is the second-least populous sovereign state in South America after Suriname; it is also one of the least densely populated countries on Earth. The official language of the country is English, although a large part of the population is bilingual in English and the indigenous languages. It has a wide variety of natural habitats and very high biodiversity. The country also hosts a part of the Amazon rainforest, the largest and most biodiverse tropical rainforest in the world.
The region known as “the Guianas” consists of the large shield landmass north of the Amazon River and east of the Orinoco River known as the “land of many waters”. Nine indigenous tribes reside in Guyana: the Wai Wai, Macushi, Patamona, Lokono, Kalina, Wapishana, Pemon, Akawaio and Warao. Historically dominated by the Lokono and Kalina tribes, Guyana was colonised by the Dutch before coming under British control in the late 18th century. It was governed as British Guiana with a mostly plantation-style economy until the 1950s. It gained independence in 1966 and officially became a republic within the Commonwealth of Nations in 1970. The legacy of British colonialism is reflected in the country’s political administration, lingua franca and diverse population, which includes Indian, African, Indigenous, Chinese, Portuguese, other European, and various multiracial groups.
Guyana is the only mainland South American nation in which English is the official language. However, the majority of the population speak Guyanese Creole, an English-based creole language, as a first language. In 2017, 41% of the population of Guyana lived below the poverty line. Guyana’s economy has been undergoing a transformation since the discovery of crude oil in 2015 and commercial drilling in 2019, with its economy growing by 49% in 2020, making it, by some accounts, currently the world’s fastest-growing economy. As it is said to have 11 billion barrels in oil reserves, the country is set to become one of the largest per capita oil producers in the world by 2025. The discovery of over 11 billion barrels of oil reserves off the coast of Guyana since 2017 is the largest addition to global oil reserves since the 1970s. Guyana is now ranked as having the fourth-highest GDP per capita in the Americas after the United States, Canada, and The Bahamas. According to the World Bank in 2023, very significant poverty still exists and the country faces significant risks in structurally managing its growth.
Health:
Compared with other neighbouring countries, Guyana ranks poorly in regard to basic health indicators. Basic health services in the interior are primitive to non-existent, and some procedures are not available at all. Although Guyana’s health profile falls short in comparison with many of its Caribbean neighbours, there has been remarkable progress since 1988, and the Ministry of Health is working to upgrade conditions, procedures, and facilities.
Source:https://en.wikipedia.org/wiki/Guyana


COMMUNITY

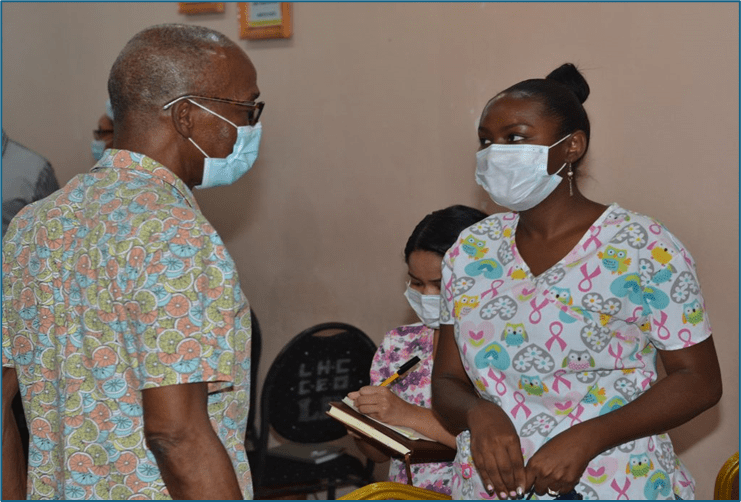
LESS than three months after its launch, President, Dr Irfaan Ali’s Newborn Cash Grant initiative is already transforming lives across Guyana, bringing hope, relief and a stronger sense of security to thousands of families.
Launched on March 8, 2025, at the Arthur Chung Conference Centre, the initiative provides $100,000 for every child born to a Guyanese mother on or after January 1, 2025.
President Ali, who has led a people-first development agenda since taking office, described the grant as a long-term investment in the future of our nation and a commitment to nurturing the next generation of leaders.
Mothers who have already benefitted from the programme shared their gratitude and explained how the grant has positively impacted their lives.
Region Four resident Aranza Krishna said she is “whole-heartedly thankful to the government and the Ministry of Health for this appreciated initiative.”
“This grant has benefitted me a lot, because it helped me to buy formula, which is very expensive; pampers which is [sic] very expensive, and it also help [sic] me to save because instead of taking out that money from my pocket, the government made that possible for me to be able to save,” she shared.
Another beneficiary, Hasyah Dodson, also from Region Four, expressed similar sentiments. “It helped me to get certain things, to put in an early savings for the baby,” she stated.
Dodson further stressed the importance of continued support, particularly for young mothers who may lack a strong support system.
“I think that the government should continue giving; in relation to young mothers that do not have the support,” she posited.
With more than 17,000 births projected for 2025, the government has reaffirmed its commitment to ensuring each newborn receives this financial start in life.
The initiative, which was first announced during the presentation of the 2025 National Budget, is part of a broader effort to enhance family welfare and social development. In total, approximately $1.3 billion will be allocated annually to facilitate the grant.
Source:https://guyanachronicle.com/2025/06/03/a-brighter-future-begins-at-birth/

At the 78th World Health Assembly (WHA), countries endorsed World Prematurity Day as an official global health campaign – part of a decision that highlights the urgent need for investment to prevent preterm births and expand access to lifesaving care for babies born early or small.
Preterm births – defined as births that occur before 37 completed weeks of pregnancy – are the leading cause of death amongst children aged under 5 years. Complications such as difficulties breathing, infections and hypothermia are common, while survivors can face significant and long-term disability and ill health.
The WHA decision document urges countries to expand access to proven, high-impact interventions, like special newborn care units, support for affected families and kangaroo mother care (KMC), which combines exclusive breastfeeding and skin-to-skin contact. For prevention, the document highlights the need to strengthen antenatal services and more broadly, improve women’ underlying health.
“Recognizing this is a crucial issue increasingly shaping child health and survival, WHO welcomes the decision to incorporate World Prematurity Day into its official calendar,” said Dr Anshu Banerjee, Director of Maternal, Newborn, Child and Adolescent Health and Ageing. “It will be an important opportunity to educate, raise awareness and advocate for action to tackle this leading cause of child mortality, while highlighting the need for additional practical, financial and policy support for affected families.”
In 2022, WHO released new clinical guidelines for care of preterm and low birthweight infants, with new guidance to help countries expand kangaroo mother care expected later this year. Alongside partners, the Organization also supports countries to deliver comprehensive newborn care packages, including special services for small and sick babies.
World Prematurity Day has been observed for over a decade, driven by advocacy from families, civil society, and health professionals. Its formal recognition by WHO is expected to further galvanize global attention and action to this critical issue for maternal and child health.
The decision was agreed following discussions on the Global Strategy for Women’s, Children’s and Adolescents’ Health (2016–2030). It aligns with the 2023 WHA Resolution to accelerate progress in maternal, newborn, and child survival, as well as the 2025 World Health Day theme: “Healthy beginnings, hopeful futures.”
World Prematurity Day will be officially marked by WHO, Member States, and partners on November 17, starting in 2025.


HEALTHCARE PARTNERS





Source:https://neonatologytoday.net/newsletters/nt-may25.pdf




PREEMIE FAMILY PARTNERS



Source:https://hiehelpcenter.org/2024/04/04/advocating-nicu-baby-7-tips-former-obstetrical-nurse/

INNOVATIONS



https://www.sciencedirect.com/science/article/pii/S2772628224000451
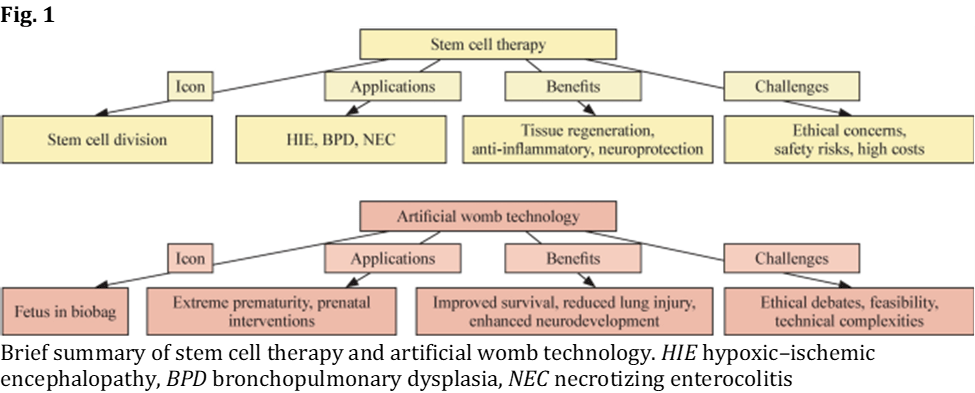
Recent decades have seen transformative advancements in neonatal care, significantly improving survival rates for preterm and critically ill neonates. From the introduction of neonatal intensive care units (NICUs) to advances in ventilation techniques and surfactant therapy, the field has evolved to meet the growing needs of vulnerable newborns . Despite these achievements, neonatal care remains a rapidly advancing specialty driven by ongoing research and technological innovation. The twenty-first century has introduced groundbreaking tools and approaches, such as stem cell therapy , artificial womb technology, and telehealth applications, which have the potential to redefine the standard of care.
Despite the above-mentioned advancements, neonatal morbidity and mortality rates remain alarmingly high, particularly in low- and middle-income countries (LMIC). Neonatal mortality remains a significant global burden, with an estimated 2.3 million neonatal deaths occurring annually worldwide. Preterm birth, a leading cause of neonatal mortality and long-term complications, affects about 15 million infants each year. Conditions such as prematurity, low birth weight, and birth asphyxia continue to pose significant challenges, contributing to long-term neurodevelopmental and physical disabilities . Neonatal hypoxic–ischemic encephalopathy (HIE) occurs in 1 to 8 per 1000 live births in high-income settings and has an even higher incidence in low-resource areas, where access to therapeutic hypothermia is limited. Similarly, bronchopulmonary dysplasia (BPD) affects nearly 40% of infants born before 28 weeks of gestation who require prolonged oxygen therapy, whereas necrotizing enterocolitis (NEC) has an incidence of 2%–5% among very low birth weight infants and is a major contributor to neonatal morbidity and mortality. In addition, the burden of neonatal care extends beyond clinical concerns, encompassing ethical dilemmas, resource allocation, and disparities in healthcare access. The economic burden associated with preterm birth and its complications is immense, with direct medical costs and long-term care requirements placing significant strain on healthcare systems globally. These persistent issues demand innovative solutions to bridge the gap between current practices and unmet needs in neonatal care.
Technological breakthroughs have emerged as powerful tools in tackling these challenges. Stem cell therapy holds promise for treating conditions, such as hypoxic–ischemic encephalopathy and bronchopulmonary dysplasia], whereas artificial womb technology offers a potential solution for extreme prematurity, enabling the continuation of fetal development outside the maternal womb. Telehealth applications have revolutionized neonatal care delivery, especially during the COVID-19 pandemic, by increasing accessibility, facilitating parental education, and enabling remote monitoring. These innovations not only aim to improve immediate clinical outcomes but also focus on enhancing long-term quality of life for neonates and their families.
This paper aims to provide a comprehensive examination of three major innovations in neonatal care: stem cell therapy, artificial womb technology, and telehealth applications. By exploring their clinical applications, potential benefits, and associated challenges, this study seeks to highlight the transformative potential of these advancements [13]. Furthermore, it emphasizes the need for continued research and interdisciplinary collaboration to optimize these technologies and address existing gaps in care delivery [14]. Ultimately, the study underscores the importance of integrating these innovations into routine neonatal practice to improve outcomes and ensure equitable healthcare for all neonates.
Stem cell therapy in neonatology
Stem cell therapy has emerged as a promising approach in neonatal care, offering potential treatments for conditions that previously lacked effective solutions. Among these are HIE, BPD, and NEC.
Current applications and clinical trials are listed as follows. Mesenchymal stem cells (MSCs) derived from bone are widely studied but require invasive harvesting procedures. Umbilical cord blood MSCs offer collection, low immunogenicity, and anti-inflammatory properties, making them ideal for HIE. Placental/Wharton’s jelly–derived MSCs are ethically and provide abundant cell yields. Induced pluripotent stem cells (iPSCs) constitute patient-specific therapies but face challenges, such as genetic instability and high production costs. Adipose-derived stem cells are easily accessible via liposuction but exhibit variability in quality depending on donor age and health . Among these, MSCs have demonstrated potential in preclinical and early clinical trials for conditions, such as HIE, BPD, and NEC
.
HIE is a leading cause of neonatal morbidity and mortality, often resulting in long-term neurodevelopmental impairments . Traditional interventions, such as therapeutic hypothermia, have shown efficacy in reducing mortality, but many infants still experience residual disabilities. HIE contributes significantly to neonatal deaths worldwide, with an estimated incidence of 1 to 8 per 1000 live births in developed countries and a much greater incidence in resource-limited settings. Stem cell therapy, particularly the use of MSCs, has demonstrated potential in preclinical and early clinical trials. These cells, derived from bone marrow, umbilical cord blood, or placental tissue, have neuroprotective effects, promoting tissue repair and reducing inflammation in animal models
.
BPD is a chronic lung disease predominantly affecting preterm infants requiring prolonged mechanical ventilation. It remains a major cause of long-term respiratory complications in preterm infants, affecting up to 40% of extremely preterm neonates who require supplemental oxygen. The role of MSCs in modulating inflammation and enhancing lung repair has been investigated. Several preclinical studies have reported improved alveolarization and reduced fibrosis following stem cell administration. Early phase clinical trials, such as the CARE–BPD trial, have evaluated the safety and feasibility of MSC transplantation, with promising initial results. In addition, the PNEUMOSTEM clinical trial in South Korea investigated the use of allogeneic umbilical cord-derived MSCs for BPD, and reported a reduction in the incidence of severe BPD among extremely preterm infants.
NEC, a severe inflammatory condition of the gastrointestinal tract, remains a significant cause of neonatal mortality. Preclinical studies suggest that stem cells can restore intestinal barrier integrity, reduce inflammatory responses, and enhance tissue regeneration. Clinical trials investigating the efficacy of stem cell-based interventions for NEC are ongoing, with early results showing reduced disease severity and improved survival rates. However, challenges remain in optimizing stem cell delivery for NEC, including timing, dosage, and the most effective cell source for therapy.
Potential benefits and challenges
Stem cell therapy holds significant promise for neonatal care by promoting tissue repair, modulating inflammation, and providing neuroprotection. Stem cells possess the ability to differentiate into various cell types, contributing to the regeneration of damaged tissues. For instance, in bronchopulmonary dysplasia (BPD), stem cells have been shown to restore lung architecture through the promotion of alveolar and vascular growth. Their immunomodulatory properties enable them to suppress proinflammatory pathways and release anti-inflammatory cytokines, thereby mitigating inflammatory damage in conditions, such as necrotizing enterocolitis (NEC) and BPD. In cases of hypoxic–ischemic encephalopathy (HIE), stem cells exert neuroprotective effects by secreting trophic factors that enhance neuronal survival, stimulate axonal growth, and support synaptic repair, as demonstrated in both preclinical and early clinical trials.
Despite these promising therapeutic effects, several challenges remain in translating stem cell therapy into widespread clinical practice. Obtaining adequate cell sources, ensuring Good Manufacturing Practice (GMP) compliance, and maintaining quality during cell processing represent major logistical and financial barriers. Ethical considerations regarding cell sourcing and infrastructure limitations, particularly in LMICs, further complicate equitable access. Long-term data on safety, efficacy, and potential adverse effects, such as immune reactions or ectopic tissue formation, remain limited and require ongoing surveillance. In addition, the absence of harmonized regulatory frameworks for stem cell isolation, characterization, and clinical application impedes broader implementation.
In conclusion, while stem cell therapy represents a transformative advancement with the potential to address critical neonatal conditions, such as HIE, BPD, and NEC, sustained research efforts and international collaboration are necessary to optimize its clinical translation and ensure global accessibility.
Artificial womb technology
The concept of ex utero gestation has long been a topic of scientific exploration, aiming to replicate the intrauterine environment to support fetal development outside the maternal womb. Significant progress has been made in recent years, culminating in prototypes such as the Biobag, a system designed to simulate amniotic fluid and uteroplacental exchange crucial for fetal survival . Notably, researchers have successfully sustained fetal lambs equivalent to 22–24-week-old human infants for several weeks in such systems, demonstrating feasible extrauterine support through a pumpless oxygenation circuit and fluid-filled environment. These proof-of-concept studies underscore the potential of artificial wombs to bridge the current viability gap for extreme prematurity, although the technology has not yet been tested in humans and remains in the experimental stage. Multiple teams worldwide are now refining these systems—from the Children’s Hospital of Philadelphia to groups in Europe, Japan, and Australia—in preparation for first-in-human trials targeting 22–24-week preterm infants once safety and efficacy criteria are met. Such efforts reflect a growing consensus that we are closer to clinical application than ever, even as critical engineering and biological challenges continue to be addressed.
Key advancements and potential impacts
Advanced extracorporeal membrane oxygenation (ECMO) technologies ensure efficient gas exchange without damaging immature lungs. Innovative vascular interface techniques (e.g., ultrashort cannulas attached to the umbilical cord) harness the fetus’s own heart to drive circulation, providing stable blood flow through the external oxygenator without introducing damaging pressure pulses. This refinement improves hemodynamic stability during ex utero support and is critical in the prolonged support achieved in animal models. Simulating amniotic fluid provides mechanical protection and promotes lung and gastrointestinal development. Innovative methods to replicate placental nutrient transfer support optimal growth. These advancements represent a paradigm shift in neonatal care, moving closer to clinical application for human neonates.
Extreme prematurity remains a leading cause of neonatal mortality, with survival rates plummeting for infants born before 24 weeks of gestation. Artificial womb technology offers a means to extend gestational age artificially, enabling these infants to complete critical developmental milestones outside the womb. The potential to improve survival rates for these vulnerable infants is unprecedented, potentially reducing neonatal mortality in high-risk populations. Early preclinical successes lend support to this optimism—for instance, fetal lambs supported ex utero showed normal growth and organ maturation over a four-week period—suggesting that, in the future, infants born at the edge of viability might be sustained until they are mature enough to thrive outside an artificial environment.
Preterm infants are highly susceptible to a range of complications due to underdeveloped organ systems. Artificial wombs could mitigate these issues by replicating the natural intrauterine environment. For example, a controlled environment reduces exposure to external mechanical stressors, minimizing the risk of intraventricular hemorrhage (IVH). Similarly, avoiding mechanical ventilation during early lung development can significantly reduce the incidence of BPD and other chronic respiratory conditions. Furthermore, sustained exposure to a controlled, nurturing environment supports optimal brain development, potentially reducing long-term cognitive and motor impairments. From a broader perspective, artificial womb technology could alleviate the emotional and financial burden on families by improving survival rates and reducing NICU stays while also lowering societal healthcare costs associated with prematurity-related complications.
In addition to bridging viability, artificial wombs may enable new treatment avenues for fetuses with congenital conditions. By temporarily transferring a fetus into an artificial environment, doctors can perform critical surgical interventions or therapies earlier in pregnancy than currently possible and then continue gestation in the device. This approach, which is still speculative, offers hope for improving outcomes in cases where treating a fetus in utero is challenging. These potential benefits highlight that artificial womb technology is not only about saving premature infants but could also transform fetal medicine by providing a stable platform for intervention while maintaining fetal development (Fig. 1).
Challenges and barriers
Artificial womb technology presents complex ethical, technical, and logistical challenges that must be carefully addressed before clinical application. Ethically, redefining the threshold of viability—potentially lowering it significantly from the current standard of around 24 weeks—raises profound questions about the beginning of life, parental autonomy, and reproductive rights. These debates intersect with broader legal and moral frameworks surrounding abortion and fetal rights, highlighting the need for clear guidelines that balance maternal autonomy with fetal interests. Ensuring that parents make fully informed decisions and addressing concerns about long-term quality of life for survivors are critical ethical priorities.
Financial and technical barriers further complicate the development and implementation of artificial wombs. These systems remain experimental, requiring substantial investment, sophisticated equipment, and specialized expertise [48]. Early clinical prototypes, supported by multimillion-dollar grants and private funding, demonstrate both the promise and the high costs associated with this technology. The integration of artificial wombs into neonatal intensive care units would demand dedicated sterile environments, continuous power supply, and around-the-clock skilled monitoring to prevent complications, such as infections or mechanical failures. Regulatory challenges also persist, as internationally harmonized standards for safety and ethical use have yet to be fully established.
Equitable access remains a major concern, as the initial deployment of artificial womb technology will likely be confined to well-resourced centers, risking disparities for patients in resource-limited settings. Overcoming these barriers will require coordinated efforts across clinical, ethical, logistical, and regulatory domains to ensure that this transformative technology benefits the broadest possible patient populations.
Telehealth applications in neonatology
Telehealth has emerged as a transformative tool in modern neonatal medicine, facilitating remote consultation, monitoring, and parental education. The COVID-19 pandemic accelerated the adoption of telehealth services, demonstrating their potential in reducing hospital visits, enhancing parental engagement, and improving neonatal outcomes. Advances in digital health technologies, including real-time video consultations, remote patient monitoring, and artificial intelligence (AI)-powered analytics, are shaping a new era of neonatal care.
Telehealth platforms provide parents of preterm or medically complex infants with virtual consultations, enabling them to access real-time guidance from neonatologists, lactation consultants, and specialists. Virtual coaching programs have been particularly effective in supporting breastfeeding initiation and adherence, as well as empowering parents to manage their infants’ medical needs post discharge.
Wearable sensors and home monitoring systems allow healthcare providers to track vital signs, such as oxygen saturation, heart rate, and respiratory patterns remotely. These innovations reduce the need for prolonged NICU stays by enabling early discharge with continued monitoring. AI-driven alert systems further increase safety by detecting early warning signs of deterioration.
In geographically remote or underserved areas, telehealth bridges gaps in access to neonatal subspecialists. Studies have shown that telehealth consultations significantly reduce the time to specialist intervention, improving clinical outcomes for neonates requiring urgent evaluation.
Potential benefits of telehealth
Providing continuous virtual access to neonatal specialists enhances parental confidence in caring for their infant at home, reducing anxiety and improving long-term adherence to care plans. By decreasing the need for in-person visits, hospital readmissions, and travel expenses, telehealth contributes to significant cost savings for both healthcare systems and families. Recent economic analyses indicate that telehealth interventions reduce overall neonatal care expenditures by up to 30% in well-integrated models. Studies suggest that remote monitoring and early intervention through telehealth can decrease complications associated with prematurity, including infections and rehospitalization rates.
Challenges and barriers
The integration of telehealth into neonatal care offers significant benefits, including improved accessibility, enhanced parental engagement, and better clinical outcomes. However, several barriers must be addressed to achieve equitable and sustainable implementation. Limited access to reliable internet infrastructure and disparities in digital literacy hinder telehealth adoption, particularly in low-income and rural communities. Variability in telehealth reimbursement policies across healthcare systems further complicates widespread use, while some regions have expanded coverage post-pandemic, others continue to impose restrictions that limit provider compensation for virtual neonatal consultations. Ensuring that telehealth platforms comply with Health Insurance Portability and Accountability Act (HIPAA) standards to safeguard sensitive neonatal health information is also critical.
Overcoming these challenges requires continued investment in digital health infrastructure, harmonization of reimbursement policies, and advancements in secure, AI-enhanced telehealth technologies. By addressing these barriers, telehealth holds the potential to revolutionize neonatal care delivery and promote global health equity.
Ethical and global health perspectives and future directions
Innovations such as stem cell therapy, artificial womb technology, and telehealth are poised to transform neonatal care. However, their successful integration requires addressing profound ethical, regulatory, and equity-related challenges.
One major concern is access and equity. Advanced neonatal technologies are predominantly concentrated in high-income countries (HICs), while LMICs struggle to provide even basic neonatal care.
Technologies such as artificial wombs and stem cell therapies are expensive and complex, potentially exacerbating disparities unless international efforts focus on affordability and scalability. Telehealth, while promising to bridge care gaps, risks widening inequities if digital infrastructure and training are not adequately developed.
Ethical and regulatory challenges further complicate adoption. Innovations such as artificial wombs raise questions about viability definitions, parental autonomy, and reproductive rights. Stem cell therapies pose dilemmas around sourcing, manufacturing standards, and long-term safety. Telehealth applications must carefully balance data privacy concerns with the convenience of remote monitoring. Clear international guidelines and harmonized regulatory frameworks are urgently needed to ensure that emerging technologies are adopted safely and equitably.
Global collaboration will be pivotal to overcoming these barriers. Cross-border partnerships, supported by organizations such as the World Health Organization, can promote knowledge sharing, funding mechanisms, and capacity building. Engaging LMIC stakeholders will be essential to ensure that innovation benefits are distributed equitably and context-specific solutions are prioritized.
Future research must focus on optimizing and expanding the clinical applications of these innovations. Stem cell therapy has shown significant potential for treating conditions such as HIE and BPD by promoting tissue repair and neuroprotection. Priorities include improving delivery methods, scaling up production, and ensuring ethical application. Similarly, artificial womb technology represents a groundbreaking advancement in supporting extremely preterm infants. Prototype systems like the Biobag mimic the intrauterine environment and have demonstrated success in preclinical models. However, ensuring clinical safety, establishing ethical frameworks, and developing robust regulatory standards are essential steps before widespread implementation. Telehealth, which has proven effective in enhancing neonatal monitoring and early intervention, must continue to evolve with investments in infrastructure, provider training, and regulatory support. Overcoming barriers such as connectivity gaps, digital literacy disparities, and cost constraints will be critical to global telehealth equity.
Emerging technologies such as gene therapy and AI-driven care offer additional opportunities for improving neonatal outcomes. Gene-based interventions could correct congenital disorders early in life, while AI tools could optimize diagnosis, monitoring, and individualized care plans. Nevertheless, these advances must be implemented thoughtfully, with attention to the specific needs of vulnerable neonatal populations, especially in resource-limited settings. Successful integration of these technologies into neonatal practice will require updating clinical protocols, training healthcare providers, and ensuring that neonatal units are equipped with necessary resources. Strong regulatory and policy frameworks should be established to support safe and efficient adoption, including mechanisms for funding, access expansion, and outcome monitoring.
By addressing these multifaceted challenges, the neonatal care community can achieve transformative advancements that improve survival rates, enhance quality of life, and reduce global health disparities. In the long term, these innovations hold the potential to reshape neonatal and childhood outcomes, alleviating burdens on families and healthcare systems worldwide.
In conclusion, this manuscript highlights the transformative potential of innovations in neonatal care, emphasizing their role in addressing persistent challenges, such as high neonatal mortality, long-term morbidity, and healthcare disparities. Key findings demonstrate that stem cell therapy offers promising solutions for conditions such as HIE and BPD by promoting tissue repair and reducing inflammation. Similarly, artificial womb technology provides hope for improving outcomes for extremely preterm infants by replicating the intrauterine environment and enabling continued fetal development . Telehealth applications complement these advancements by expanding access to neonatal care, particularly in underserved regions while empowering families and reducing the burden on healthcare systems.
The importance of innovation in neonatal care cannot be overstated. These advancements have the potential to redefine the standard of care, improve survival rates, and enhance the quality of life for neonates and their families. However, their successful integration into clinical practice requires addressing ethical concerns, regulatory challenges, and inequities in access. A concerted effort to bridge these gaps will be critical in ensuring that these technologies benefit all populations, regardless of socioeconomic or geographic constraints. To achieve this vision, researchers, policymakers, and clinicians must collaborate closely. Researchers should prioritize translational studies that validate the efficacy and safety of these technologies, whereas policymakers should develop robust frameworks that address cost barriers and promote equitable access. Clinicians, as frontline implementers, play a pivotal role in integrating these innovations into routine practice while advocating for patient-centered approaches.
By fostering interdisciplinary collaboration and investing in global partnerships, the neonatal care community can overcome existing barriers and pave the way for a brighter future. The ultimate goal is to ensure that every neonate, irrespective of their circumstances, receives the highest standard of care. This collective commitment to innovation, equity, and compassion has the power to reshape neonatal medicine and improve outcomes for generations to come.
Source: https://link.springer.com/article/10.1007/s12519-025-00927-1

Source: https://pubmed.ncbi.nlm.nih.gov/40433702/