The Czech Republic, also known as Czechia and historically known as Bohemia, is a landlocked country in Central Europe. The country is bordered by Austria to the south, Germany to the west, Poland to the northeast, and Slovakia to the southeast.]The Czech Republic has a hilly landscape that covers an area of 78,871 square kilometers (30,452 sq mi) with a mostly temperate continental and oceanic climate. The capital and largest city is Prague; other major cities and urban areas include Brno, Ostrava, Plzeň and Liberec.
The Czech Republic has a universal health care system, based on a compulsory insurance model, with fee-for-service care funded by mandatory employment-related insurance plans since 1992. According to the 2018 Euro Health Consumer Index, a comparison of healthcare in Europe, the Czech healthcare is ranked 14th, just behind Portugal and two positions ahead of the United Kingdom.
- GLOBAL PRETERM BIRTH RATES – Czech Republic
- Estimated # of preterm births: 7 per 100 live births
- (Global Average: 10.6)
- Source- WHO Preterm Birth Rate (Per 100 Live Births)

COMMUNITY

Stories of preterm birth are stories of joy and heartbreak, faith and love. Moving and uplifting. They have the power to inspire. This montage is an all-time favourite of ours and reflects the true heart and face of our work to prevent preterm birth. The Australian Preterm Birth Prevention Alliance is eternally grateful to these wonderful women, these mothers of premature babies, for sharing their very powerful stories.



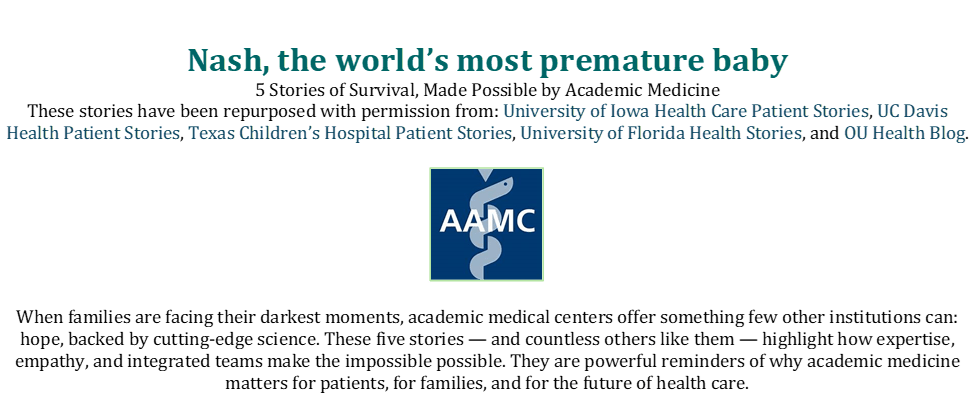
Abstract: The World Health Organization has named climate change as the greatest threat to public health. In the United States, the healthcare sector accounts for 8.5% of greenhouse gas (GHG) emissions. Neonatal Intensive Care Units (NICUs) and the patients and families who rely on their medical interventions and overall guidance are uniquely impacted by climate change. So, what should NICU professionals know, and what should NICU professionals do? NICU clinicians and designers should recognize that healthcare contributes to climate change, which in turn worsens health issues, especially for vulnerable groups affected by social determinants of health. NICU professionals are well-positioned to understand and influence health equity, having participated in related efforts. Insights gained from addressing health equity can inform strategies for approaching climate change. Individuals should advocate within their organization for climate-forward policies and can counsel patients on climate-forward behavior, implementing education programs where possible. NICUs can transition to reusable surgical gowns and linens safely. Additionally, NICU professionals should advocate for decarbonized building systems whenever new construction or renovations are proposed. Hospitals should advocate for integrating sustainability into their operations and culture. Decarbonization plans should be developed and implemented to reduce climate impacts. Healthcare systems should strive to decarbonize their operations and also consider influencing their supply chain. The NICU has a unique opportunity to make a difference.
Introduction: Our most difficult and stressful challenges all end up at the hospital, and especially in the Neonatal Intensive Care Unit. NICU professionals, such as neonatologists, nurses, therapists, administrators, environmental services staff, and facilities staff, intimately know the details of their most challenging cases. The impact on families is profound. . Families do not want others to experience what they have experienced.
Nevertheless, climate change exacerbates health challenges and may ultimately lead to increased NICU admissions, This represents a vicious cycle: providing NICU care produces carbon emissions that lead to environmental harm, which in turn increases NICU admissions. The implications are clear. The NICU must deliver excellent care while reducing its environmental footprint. NICUs, in particular, have a moral imperative and an opportunity to minimize carbon and other environmental impacts. To achieve this goal, what should neonatologists know, and how can they help?
This paper provides an informational overview, citing literature on the climate crisis, the role of healthcare, and the role of the NICU in contributing to the crisis. It briefly considers health equity as a model for both how societal challenges impact the NICU and how NICUs have responded to address these challenges. Then it identifies some practical ways NICUs can reduce their impact on climate change while buttressing the resilience of the patients and families they serve.
What You Should Know
Humans Impact Climate Change
The scientific foundation of climate change is unequivocal. The Intergovernmental Panel on Climate Change (IPCC), in its Sixth Assessment Report confirmed that human activity—primarily the combustion of fossil fuels and deforestation—is responsible for the observed rise in global average temperatures since the pre-industrial era. The Earth’s surface has already warmed by 1.1°C, with current trajectories placing the planet on track to exceed 1.5°C of warming within the next two decades unless emissions are drastically curtailed.
This warming is driving a cascade of systemic changes, including the increasing frequency and severity of heatwaves, wildfires, droughts, storms, and floods; rising sea levels and coastal erosion; ocean acidification; and biodiversity loss. The climate system’s destabilization is not only an environmental phenomenon— it has become a structural determinant of human health.
The IPCC warns that without immediate and drastic reductions in GHG emissions, the world is likely to exceed 2°C of warming by mid-century, a threshold associated with widespread agricultural collapse, mass displacement, and infrastructure failure (6). For healthcare systems, this future portends interrupted services, overwhelmed emergency rooms, supply shortages, and soaring demand for mental health and infectious disease care. Thus, climate action is foundational to public health preparedness and systems resilience.
Climate Change Impacts Health
From the standpoint of healthcare, climate change poses a comprehensive threat to public health, affecting every organ system, population, and location. The World Health Organization (WHO) has called it “the single biggest health threat facing humanity”. Key health impacts include heat-related illnesses and deaths, vector-borne diseases, including malaria, dengue, Lyme disease, and West Nile virus , respiratory conditions: from exposure to fine particulate matte , increasing asthma exacerbations, COPD flare-ups, and cardiovascular morbidity. Climate change poses significant risks to agriculture in a world where 2 billion people lack essential micronutrients . Climate-related trauma, such as displacement, economic instability, and environmental grief, can increase anxiety, depression, PTSD, and substance use disorders, as well as food and water insecurity. These mental health impacts fall most heavily on low-income groups, communities of color, Indigenous peoples, children, and the elderly, who already face structural barriers to healthcare.
Climate Change Particularly Impacts Neonatal and Perinatal Health
Children are among the most vulnerable populations to the health effects of climate change. They are not only physically more susceptible to environmental hazards since they breathe more air and consume more food and water per kilogram of body weight than adults, but also developmentally dependent on the stability of ecological, social, and healthcare systems. Furthermore, exposures during critical developmental windows, particularly in utero and during the neonatal period, can have lifelong implications for respiratory health, neurodevelopment, immune function, and cardiovascular risk . A systematic review found that maternal exposure to extreme heat is associated with a statistically significant increased risk of adverse pregnancy outcomes.
Particulate matter (especially PM2.5) from traffic, fossil fuels, and increasingly wildfires, which are more common due to a changing climate, is associated with increased risk of low birth weight and preterm birth.
Climate Change puts demands on NICU Operations
The climate crisis also poses increasing operational and ethical challenges to neonatal intensive care units (NICUs). Facilities themselves are vulnerable to climate disruptions, including flooding, wildfires, supply chain interruptions, and power outages. Clinicians must now consider climate resilience as a core function of the NICU. This includes investments in redundant power systems, emergency planning for neonatal transport, and sustainable design to ensure uninterrupted care delivery.
The carbon footprint of neonatal care, caused by single-use plastics, energy-heavy incubators, and anesthetic gases, prompts questions about how NICUs can cut emissions while ensuring safety.
Structural/Social Determinants of Health impact NICU Admissions and NICU outcomes Structural and social determinants of health (SDOH) significantly influence neonatal outcomes, especially in NICUs, where medical vulnerability intersects with systemic inequities. Social determinants of health include access to and quality of education, healthcare, neighborhood and built environment, social and community context, and economic stability (15). Recent studies offer strong empirical evidence linking race, socioeconomic status, geography, and language to disparities in NICU experiences and clinical outcomes (16–19). Addressing these determinants is crucial not only for equity but for clinical excellence in neonatal care.
Climate Change Intensifies the Inequitable Impact of Social Determinants of Health
Climate change exacerbates the social determinants of health that already affect children. Infants born into poverty, homelessness, or marginalized communities face a triple threat: they are more exposed to environmental risks, less likely to access high-quality healthcare, and more affected by systemic racism. For example, historically redlined neighborhoods in US cities are more likely to be heat islands, characterized by fewer green spaces and higher rates of air pollution, which correlates with higher rates of chronic disease.
Indigenous children face disproportionate health risks from water insecurity, wildfire displacement, and food system collapse. Worldwide, children in the Global South will bear the most significant disease burden despite contributing the least to the climate crisis.
For neonatologists, these inequities are not abstract. They show up in disparities in preterm birth rates, NICU admissions, and developmental outcomes, trends that will worsen without targeted intervention.
Healthcare is a major contributor to Greenhouse Gas Emissions (GHG)
While healthcare systems are at the frontlines of climate impact, they are also major contributors to the crisis. Globally, healthcare is responsible for 4.4% of net GHG emissions . In the United States, the sector emits roughly 8.5% of national emissions, making it one of the largest institutional sources of pollution.
Emissions arise from energy use, high-impact anesthetic gases such as desflurane and nitrous oxide, pharmaceutical and medical supply chains, patient transportation, waste incineration, and water consumption.
Thus, the Act of Delivering Healthcare Can Cause Harm
Critically, these emissions pose a contradiction to the sector’s mission: the act of delivering care can simultaneously cause harm through environmental degradation. As such, climate mitigation must be reframed as a core component of healthcare quality, safety, and ethics.
Organizations can make a difference despite changing national-level policies.
In this context, a diverse array of actors, including healthcare organizations, nonprofits, local, provincial/state, and national governments, as well as international organizations, have mobilized in response. While the role of nations is important, climate action happens at the provincial/state, local, organizational, and even individual levels. At the time of this writing, several changes to United States federal policy were made. The Office of Climate Change and Health Equity was disbanded by executive order, eliminating one of the few federal bodies explicitly focused on climate equity in healthcare. Additionally, NIH climate and health research funding was paused or eliminated. Even during times of changing federal policy, other actors, including health care organizations, can continue to make progress.
Healthcare Systems Have Made or Maintained Commitments to Decarbonize
In 2025, the Health Sector CARES Pledge (Climate Action, Resilience, and Equity Solutions) was introduced to replace a repealed US Health and Human Services Health Sector Pledge. The CARES pledge invites hospitals and health systems to publicly commit to a 50% reduction in Scope 1 and 2 emissions by 2030, complete Scope 3 emissions inventories within one year, and embed climate resilience and equity into their operations.
Within months of its release, more than 60 systems, including CommonSpirit Health, Providence, and NYC Health + Hospitals, had signed on.
Additionally, the National Academy of Medicine (NAM) has continued to push for sector-wide decarbonization.
It is possible to Decarbonize Building Emissions.
Building utility decarbonization is possible, and several hospitals are making significant progress in their plans to decarbonize. Decarbonizing building and utility emissions involves three fundamental steps: 1. Reduce the consumption of electricity as much as possible; 2. Switch your systems (for example, heating, sterilizers, kitchen equipment, etc.) to run on electricity instead of fossil systems (natural gas, steam, etc.); and 3. Procure electricity from renewable sources. When you have electrified emissions and procured your electricity from renewable sources, you have effectively decarbonized. Reducing energy as a first step enables you to decrease the amount of energy that needs to be electrified, thereby lowering costs.
On the electricity production side, onsite- or offsite-owned zerocarbon energy (such as solar) reduces purchases of emissions from dirty sources. Organizations can enter contracts to procure renewable energy. Within renewable energy purchasing, there is CommonSpirit Health, Providence, and NYC Health + Hospitals, had signed on. Additionally, the National Academy of Medicine (NAM) has continued to push for sector-wide decarbonization.
It is possible to Decarbonize Building Emissions.
Building utility decarbonization is possible, and several hospitals are making significant progress in their plans to decarbonize. Decarbonizing building and utility emissions involves three fundamental steps: 1. Reduce the consumption of electricity as much as possible; 2. Switch your systems (for example, heating, sterilizers, kitchen equipment, etc.) to run on electricity instead of fossil systems (natural gas, steam, etc.); and 3. Procure electricity from renewable sources. When you have electrified emissions and procured your electricity from renewable sources, you have effectively decarbonized. Reducing energy as a first step enables you to decrease the amount of energy that needs to be electrified, thereby lowering costs. On the electricity production side, onsite- or offsite-owned zerocarbon energy (such as solar) reduces purchases of emissions from dirty sources. Organizations can enter contracts to procure renewable energy. Within renewable energy purchasing, there is a concept called additionality. Additionality refers to renewable energy contracts where the purchase results in an increase in the total amount of renewable energy. For example, a contract to purchase renewable electricity from an existing hydroelectric power plant is not additional, since the energy would be placed on the grid regardless of whether you made the purchase or not. An investment in a new wind farm would be additional, since the new wind farm would not exist without purchase. By purchasing additional renewable energy, you are actually reducing greenhouse gas emissions. Decarbonizing existing facilities can be challenging, but there are resources available to support the process. The Guidebook for Decarbonizing Healthcare (www.decarbhealthcare.com) provides helpful information. For new buildings, the ASHRAE/ASHE Decarbonizing Hospital Buildings Guidebook (24) provides a detailed guide focused on the design, construction, and operation of new hospital buildings and major renovations. This guidebook includes a treatment of embodied carbon—the carbon associated with a building’s construction (as opposed to operation), which is helpful. The healthcare industry is focused on decarbonization, and there are practical guides available to help achieve this goal.
What Can “You” Do?
Be Motivated by NICU-led Health Equity Work
You should also be aware of the progress made in thinking on NICU, health equity, and population health, as NICU professionals have played a unique role in this space.
The Neonatal Intensive Care Unit (NICU) plays a pivotal yet often underrecognized role in shaping population health trajectories. Traditionally viewed as acute care settings, NICUs are now being reimagined as launchpads for long-term developmental, social, and community health outcomes. Bold new ideas in design further this trend (25). A growing body of literature supports the integration of NICU care with broader public health models to address disparities and promote lifelong well-being. Several studies stand out.
Population-based NICU care models have been developed to redesign follow-up programs for children at risk of falling through safety nets. For example, Litt et al. propose a Life Course Health Development (LCHD) framework that emphasizes the importance of early experiences in shaping long-term outcomes. Their model encourages NICUs to coordinate care that extends beyond survival, integrating follow-up services, community engagement, and policy reform. The theoretical strength of this model lies in its comprehensive approach to public health through individualized care for neonates .
Equity audits, culturally competent care, and social supports are being developed to mitigate the compounded effects of racial and socioeconomic inequities on neurodevelopmental outcomes post NICU. Neonatologists are proposing new models of neonatal follow-up that emphasize family and child function. For example, leveraging existing staff, a NICU raised the level of social risk screening coupled with referral to resources in the NICU, with effective results.
Moreover, the familiar Vermont Oxford Network Potentially Better Practices for Follow Through are a key acknowledgement of the idea that “As neonatal care providers, we play critical roles in the lives of small and sick newborns and their families and therefore are uniquely positioned to address social determinants of health. Our responsibility to infants and families extends beyond the walls of the hospital or clinic. We must follow through. Follow-through is different from the more typical neonatal practice of ‘follow-up.’ It is a comprehensive approach that begins before birth and continues into childhood. Health professionals, families, and communities must partner to meet the social as well as medical needs of infants and families to achieve health equity”.
These efforts are highly relevant for two reasons. First, climate change will exacerbate health equity challenges. The forward thinking NICU will therefore need to be even more diligent about addressing social determinants of health and disparities, even to maintain its current level of outcomes. NICU professionals should be aware of this and the ways that colleagues have effectively done this work. Second, NICUs have uniquely developed systems to address complex problems that involve both upstream and downstream factors, for which it may initially seem that the NICU has little to no control. This type of thinking and action provides important lessons and motivation as NICUs strategize to impact decarbonization.
At the Individual Level: Empowering Climate-Conscious Healthcare Workers
Individual healthcare workers and patients are often the first points of contact in the climate-health interface. Although their personal choices might seem modest in scale, the cumulative effect across a large workforce and patient population can be profound. For instance, clinicians can make deliberate choices to avoid low-value care, such as ordering unnecessary diagnostic tests or procedures, which then not only reduces patient harm but also curbs resource waste and emissions. Similarly, choosing digital over printed materials, avoiding overuse of disposables, and advocating for reusable equipment where safe are all everyday actions that help reduce waste streams.
Clinicians also influence clinical practice. By counseling patients on climate-resilient behaviors, such as adopting plant-based diets, quitting smoking, and using active transportation like walking or biking, they can advance both individual health and climate goals. Hospitals like Kaiser Permanente have adopted this ethos, offering incentives for green commuting, including subsidized transit passes, bike facilities, and carpooling programs.
Education is essential. Frontline providers who are informed about the health effects of climate change are better equipped to communicate with patients and colleagues, thereby reinforcing a culture of climate literacy and sustainable practices—these actions, while individual, are essential building blocks for larger systemic change.
Neonatologists are uniquely positioned to advance climate-responsive care. Their roles span clinical advocacy, research, systems improvement, and public health engagement. NICU professionals should collaborate with hospital leadership to reduce waste, switch to lower-impact equipment, and improve energy efficiency. Other actionable steps include implementing clinical screening for climate-related risk factors: housing instability, exposure to air pollution, maternal heat stress, and advocacy for policies that reduce air pollution, expand maternal protections during heatwaves, and strengthen infrastructure for birth centers and NICUs.
Additionally, NICU professionals can lend their voices to interdisciplinary coalitions that recognize child health as a core pillar of climate justice. Their authority, rooted in science and ethics, can shape public discourse and health policy.
At the NICU Level: Greening High-Intensity Care Without Compromising Safety
The NICU represents one of the most resource-intensive settings within a hospital. Infants in NICUs often require continuous monitoring, temperature control, oxygen therapy, and sterile environments, all of which demand energy and generate waste. Nevertheless, even here, there are viable strategies for reducing environmental impact without compromising safety.
NICUs can rethink single-use items. Many NICUs have historically relied heavily on disposable gowns, linens, and medical tools to ensure sterility. However, studies suggest that switching to reusable surgical gowns offers both environmental and financial benefits.
NICU professionals should insist that major renovation or new construction projects are designed to use zero operational carbon. The NICU should enthusiastically support any hospital decarbonization efforts. This includes supporting energy reduction projects. NICUs rely on constant power to support incubators, ventilators, and monitors. Retrofitting these spaces with LED lighting, motion sensor controls, and energy-efficient HVAC systems can lead to substantial energy savings.
Additionally, better waste segregation can reduce the overclassification of waste as “regulated medical waste,” which is often incinerated and carries a carbon footprint several times greater than general waste.
Finally, NICUs may consider approaches to manage the use of oxygen and anesthetic gases, especially during surgeries involving neonates. Choosing lower-impact anesthetic agents and using them judiciously not only reduces GHG emissions but also protects staff from exposure.
At the Hospital Level: Embedding Sustainability in Operations and Culture
At the hospital level, climate mitigation must become a central tenet of operational planning. Hospitals are significant consumers of energy, water, and materials, and they generate substantial waste, including high GHG emissions from anesthetic gases and sterilization processes.
A critical area for action is the operating room, which can account for 30% or more of hospital waste. Hospitals like Hackensack University Medical Center have implemented successful initiatives to eliminate the use of desflurane, a potent anesthetic with a global warming potential more than 2,500 times that of carbon dioxide. By switching to sevoflurane or total intravenous anesthesia, they significantly reduced emissions without compromising patient care.
Food services represent another high-impact area. Hospitals serve millions of meals each year, and most of these meals traditionally rely on carbon-intensive meat and dairy products. Transitioning toward plant-forward menus, sourcing food locally, and implementing food waste diversion programs, such as composting and donating excess food, can significantly reduce a hospital’s environmental impact. Several institutions working with Health Care Without Harm have reported cost savings and improved patient satisfaction with healthier, sustainable meals).
Additionally, investing in green building standards, such as LEED certification, for new construction or retrofitting existing infrastructure with high-performance HVAC systems, water recycling systems, and smart building automation can generate long-term savings and enhance resilience. Hospitals like the Cleveland Clinic have reduced their emissions by 20–30% between 2010 and 2020 with a plan to continue improving energy and waste performance.
These changes often require a cultural shift. Hospitals must empower a “green team” of clinicians, facilities managers, and executives to drive change, track metrics, and communicate progress regularly to staff and the community.
At the Health System Level: Leading Climate Action Through Policy and Partnerships
At the top of the pyramid, health systems have the unique capacity to shape supply chains, influence public policy, and lead national or global climate action. They can develop system-wide sustainability roadmaps that set science-based targets for emissions reductions and embed climate goals into governance structures. Large health systems, such as Kaiser Permanente in the US, have achieved carbon neutrality through investments in renewable energy, the elimination of coal-based power contracts, sustainable procurement practices, and aggressive energy efficiency efforts. Their model proves that decarbonization is achievable at scale with proper leadership and investment.
On a broader level, health systems can influence their entire supply chain by prioritizing vendors that meet environmental, social, and governance (ESG) criteria. Given that the majority of healthcare’s emissions are Scope 3 (indirect) emissions from supply chains, procurement reform is one of the most powerful levers available (36).
Finally, resilient infrastructure planning is essential. Hospitals now require climate-resilient infrastructure, microgrids, and emergency plans to ensure they remain operational during floods, wildfires, and extreme heat events.
Organizations that act decisively can not only reduce their environmental footprint but also improve population health, lower costs, and build long-term resilience. Every part of the healthcare system is essential in the move toward climate-smart care.
Conclusion:
Climate change is a threat to public health, impacting children and neonates all around the world, making them more likely to end up in the NICU and more likely to have adverse long-term outcomes. Likewise, climate change will augment health inequities. Like all areas of hospitals, NICUs contribute significantly to greenhouse gas emissions. There is an imperative for NICUs to have a positive impact on the climate. Fortunately, this is possible. By leveraging their unique voice and in-depth understanding of complex problems, NICU professionals can advocate for policies and projects that significantly reduce the carbon footprint of operating the NICU, thereby continuing to save babies and families.



HEALTHCARE PARTNERS
To learn more, check out our article here: https://trueconf.com/blog/reviews-com.
Check out the video to see the best option for your medical practice.




PREEMIE FAMILY PARTNERS
Having a baby in the NICU changes you. Even after your preemie is home, the emotional rollercoaster doesn’t always stop. The stress, anxiety, fear, and trauma of premature birth and intensive care can linger—and that’s completely normal.
In fact, parents of premature babies are more likely to experience postpartum depression, anxiety, and even post-traumatic stress. That’s why supporting your mental health isn’t optional—it’s essential. This article will help you recognize what you’re feeling, know when to seek support, and give yourself permission to heal and thrive alongside your baby.
Common Emotional Experiences for Preemie Parents
You may feel a complex mix of emotions—many of them contradictory:
- Joy at progress and milestones
- Fear of setbacks or illness
- Guilt for not being able to prevent early birth
- Grief over the loss of a “normal” birth or newborn experience
- Helplessness during the NICU stay
- Overwhelmed during the transition home
These are real, valid, and common. There’s no “right” way to feel.
Attending routine well-child exams at Kids Central Pediatrics helps ensure your baby is growing and developing properly, and allows their doctor to detect diseases or illnesses before serious complications arise.
Common Causes of Premature Birth
Understanding why prematurity happens is helpful, though sometimes a specific cause is never found. Common reasons include:
- Multiple pregnancies (twins, triplets, etc.)
- Maternal infections or chronic conditions (like high blood pressure or diabetes)
- Problems with the placenta or uterus
- Premature rupture of membranes (water breaking early)
- Smoking, substance abuse, or poor prenatal care
- History of previous premature births
Often, a combination of factors is involved. Regardless of the cause, your focus now shifts to supporting your baby’s health and development from day one.
Signs You May Be Struggling
It’s okay to feel stressed—but if it starts interfering with your ability to function or connect, it’s time to talk to someone. Look out for:
- Trouble sleeping even when baby is sleeping
- Constant worry or racing thoughts
- Feeling numb or detached from your baby
- Crying frequently or feeling hopeless
- Panic attacks or shortness of breath
- Avoiding social interactions or appointments
- Feeling like you’re failing, even when others say you’re doing great
Partners can experience these feelings too, even if they show up differently (withdrawal, irritability, overworking).
Postpartum Depression, Anxiety, and PTSD
Postpartum depression (PPD) and postpartum anxiety (PPA) are not limited to moms of full-term babies. Preemie parents are often at even higher risk due to:
- Medical emergencies during labor and birth
- Separation from baby in the NICU
- Prolonged uncertainty and fear
Some parents also develop post-traumatic stress disorder (PTSD) after a difficult NICU journey.
You are not weak or broken if you’re experiencing any of this. These are medical conditions that deserve treatment, just like any other.
When and How to Get Help
If your emotions are interfering with your daily life or sense of well-being, reach out early:
- Talk to your pediatrician—they often screen parents for mental health, not just babies
- Call your OB-GYN or primary care provider
- Connect with a therapist—ideally one who understands perinatal or NICU-related trauma
- Ask your hospital social worker or NICU follow-up clinic for resources
Getting help isn’t selfish—it’s one of the best things you can do for your baby and your family.
Coping Strategies That Help
While professional support is key, there are daily habits that can make a big difference too:
Talk about it
- Share your story with people you trust
- Join an online or local NICU parent support group
Practice self-care (even in small doses)
- Take a hot shower, short walk, or 10-minute break
- Eat nourishing meals and drink water
- Ask for help with meals, errands, or childcare
Sleep whenever you can
- Trade night shifts with a partner or loved one
- Let chores go when possible
Lower your expectations
- This is not the time for perfection
- Focus on bonding and surviving one day at a time
Celebrate progress
- Write down your baby’s wins—and your own
- Acknowledge how far you’ve come
Supporting Each Other as Partners
Preemie journeys can be hard on relationships. Open communication, shared responsibilities, and giving each other space to grieve or cope differently are essential.
- Ask each other, “How are you really doing?”
- Divide tasks fairly, including night feedings, appointments, and household needs
- Make time for connection—even if it’s just a short walk or a meal together
What If You’re Feeling Better Now?
That’s wonderful—and also normal. Not every parent develops a mental health condition, and many experience healing as their baby grows stronger. Still, check in with yourself often, especially during big transitions (like going back to work, starting daycare, or hitting developmental milestones).
Your journey as a preemie parent is ongoing, and emotions can resurface at any time.
You are not alone, and you are not failing. The strength it takes to care for a premature baby is immense—but you don’t have to carry it alone. Prioritizing your mental health is not a luxury—it’s a foundation for healing, resilience, and parenting from a place of wholeness.
You deserve support, just like your baby does. Reach out. Speak up. You are worth it.
https://kidscentralpediatrics.com/supporting-your-mental-health-as-a-preemie-parent/

Families of preterm and sick newborns face unique challenges that require strong support, advocacy, and collaboration. Around the world, dedicated parent and patient organizations provide vital guidance, raise awareness, and drive improvements in neonatal and maternal care. Their voices ensure that the needs of babies and families are heard at every level – from local communities to international policy.
Collaboration Opportunities for Parent and Patient Organizations
If you have already established a charitable parent or patient organization, advocacy group, or self-help initiative, we welcome your interest in collaborating with us. Ideally, your group has a clear vision for supporting families of preterm babies in your region and a defined path toward achieving these goals.
Accepted parent and patient organizations benefit from:
- Regular exchange and digital meetings with our global network, including updates on GFCNI’s activities
- Workshops and training opportunities designed to strengthen your impact
- Access to a worldwide community of organizations eager to share knowledge and experience
- Free information and campaign materials, potentially available in your local language
- Opportunities to participate as supporters in global awareness campaigns
- Occasional involvement in research projects as parent or patient representatives
Our Global Network of Parent and Patient Organizations
Across the world, parent and patient organizations are leading change for preterm and sick newborns and their families. By joining our global network, we create a stronger voice for advocacy, share valuable knowledge and resources, and work together to ensure that every baby and family has access to the care and support they need.
Below, you can explore the wide range of parent and patient organizations that are already part of our international community. If your organization is interested in joining our network, we warmly invite you to contact us at network(at)gfcni.org.

When Nash Keen was born, he weighed just 10 ounces, less than a can of soda. His journey is one of medical innovation, relentless teamwork, and the unique capabilities of University of Iowa Health Care’s Stead Family Children’s Hospital, one of the few places in the world equipped to treat babies born so early.
Nash’s birth came just after crossing the hospital’s 21-week threshold for active intervention — timing that high-risk obstetrician Malinda Schaefer, MD, PhD, called “a new frontier in maternal-fetal medicine.” A multidisciplinary team of 21 neonatologists, nine NICU fellows, and dedicated nurse practitioners, nurses, respiratory therapists, dietitians, pharmacists, physical and occupational therapists, and more sprang into action. They inserted a breathing tube — an extraordinary feat for a baby so small — and began targeted organ support using hemodynamic monitoring, a technique pioneered at University of Iowa that allows clinicians to modify treatment based on real-time assessments of heart function and blood flow.
“When he was first born, his blood pressure was really low,” said neonatologist Amy Stanford, MD. “With hemodynamics, we could see that his heart was functioning well, so we adjusted our approach.” This precision medicine approach cuts the chance of death or major brain bleeding in very premature babies in half.
Over the next six months in the NICU, Nash underwent surgery, received dozens of medications, and was monitored around the clock. “They were on top of it every step of the way,” said his father, Randall Keen.
“They made sure we were well-informed and kept us involved in all the decision-making.”
Today, Nash is learning, playing, and growing like any other two-year-old. His Guinness World Record-breaking outcome reflects the strength of academic medicine: a blend of cutting-edge science, collaborative care, and compassion that gives even the smallest, most vulnerable patients a chance at life.
“Every patient teaches us something,” said Stanford. “And we use those lessons to improve care for the next.”
https://www.aamc.org/news/5-stories-survival-made-possible-academic-medicine

INNOVATIONS

https://www.sciencedirect.com/science/article/pii/S0033350624004402
Scientists linked a maternal gut microbe that degrades key pregnancy hormones to early labor, potentially serving as a predictive risk biomarker.
During pregnancy, expectant mothers often take steps to prepare for the arrival of their baby, such as taking vitamins and supplements and avoiding smoking or alcohol. While a typical pregnancy lasts about 40 weeks, preterm birth—defined as birth before 37 weeks of gestation—can occur and is the leading cause of neonatal and under-five mortality worldwide.
Although much research has focused on the vaginal microbiome and its potential connection to preterm birth, the role of the gut microbiome remains less understood. This gap in knowledge motivated a group of researchers in China to explore the maternal gut microbiome more closely and assess its potential link to preterm birth.
In a recent study, published in Cell Host & Microbe, the team identified maternal gut microbes associated with a higher risk of preterm birth during early pregnancy, especially those that can degrade estradiol, an important pregnancy hormone.2 The researchers hope to further explore this association of estradiol-degrading bacteria as potential predictive biomarkers for preterm birth.
First, the researchers gathered stool and blood samples from two groups of pregnant women—one in early pregnancy and the other in mid-pregnancy. Using metagenome and 16S rRNA sequencing, the team identified similar gut microbiota profiles across the women. From this, they found five prevalent genera: Blautia, Faecalibacterium, Bacteroides, Anaerostipes, and Streptococcus. At the same time, they tracked each woman’s preterm delivery status.
The researchers then turned to statistical models to dive deeper into the relationship between the gut microbiota and factors like gestational duration and preterm birth. Their analysis uncovered 11 specific genera linked to these outcomes, but one species stood out: Clostridium innocuum. This bacterium had the strongest connection to preterm birth.
Intrigued by C. innocuum, the team investigated its role in sex hormone metabolism and found that it makes an enzyme that degrades estradiol, a hormone important in pregnancy. To explore this further, they tested the bacterium’s estradiol degrading ability in female mice across different gestational periods (from early pregnancy to having a near-term fetus) and found that doses of C. innocuum significantly reduced estradiol levels by converting it into estrone. Additional analysis revealed key enzymes in the bacterium that played a critical role in this process.
Because of these findings, the researchers hypothesize that a high prevalence of C. innocuum may dysregulate estradiol levels and increase the risk of preterm birth. However, the team also acknowledged that scientists would need to evaluate more cohorts to validate these findings in broader populations.
“This study suggests that for pregnant women or women preparing to become pregnant, it may be important to monitor their gut microbiome to prevent potential adverse pregnancy outcomes,” said study coauthor An Pan, an epidemiologist at Huazhong University of Science and Technology in a press release.
https://www.the-scientist.com/improving-serological-pipetting-for-cell-culture-72953