Belize is a country on the north-eastern coast of Central America. It is bordered by Mexico to the north, the Caribbean Sea to the east, and Guatemala to the west and south. It also shares a maritime boundary with Honduras to the southeast. Despite being in central America, Belize identifies with the Caribbean region, and is a member of the Caribbean Community (CARICOM) and the Commonwealth Caribbean, the historical British West Indies.
The Maya civilization spread into the area of Belize between 1500 BCE and 300 CE and flourished until about 1200. European contact began in 1502–04 when Christopher Columbus sailed along the Gulf of Honduras. European exploration was begun by English settlers in 1638. Spain and Britain both laid claim to the land until Britain defeated the Spanish in the Battle of St. George’s Caye (1798). It became a British colony in 1840, and a Crown colony in 1862. Belize achieved its independence from the United Kingdom on 21 September 1981.[ It is the only mainland Central American country which is a Commonwealth realm, with King Charles III as its monarch and head of state, represented by a governor-general.
Belize’s abundance of terrestrial and marine plants and animals and its diversity of ecosystems, including extensive coral reefs, give it a key place in the globally significant Mesoamerican Biological Corridor. It is considered a Central American and Caribbean nation with strong ties to both the American and Caribbean regions.
It has an area of 22,970 square kilometres (8,867 sq mi) and a population of 397,483 (2022). Its mainland is about 290 km (180 mi) long and 110 km (68 mi) wide. It is the least populated and least densely populated country in Central America. Its population growth rate of 1.87% per year (2018 estimate) is the second-highest in the region and one of the highest in the Western Hemisphere. Its capital is Belmopan, and its largest city is the namesake city of Belize City. The country has a diverse society composed of various cultures and languages. It is the only Central American country where English is the official language. Belizean Creole and Spanish are widely spoken, followed by the Mayan languages and Garifuna. Over half the population is multilingual due to the diverse linguistic backgrounds of the population. It is known for its September Celebrations and punta music.
Source: https://en.wikipedia.org/wiki/Belize
Healthcare in Belize is provided through both public and private healthcare systems. The Ministry of Health (MoH) is the government agency responsible for overseeing the entire health sector and is also the largest provider of public health services in Belize. The MoH offers affordable care to a majority of Belizeans with a strong focus on providing quality healthcare through a range of public programs and institutions.
In contrast to the public health sector, the private health sector provides care to a smaller portion of the population. However, similar to the public sector, private health services are offered at a relatively low cost with a shared emphasis on quality of care and quality improvement.
The Human Rights Measurement Initiative[3] finds that Belize is fulfilling 83.0% of what it should be fulfilling for the right to health based on its level of income. When looking at the right to health with respect to children, Belize achieves 99.1% of what is expected based on its current income. In regards to the right to health amongst the adult population, the country achieves only 86.6% of what is expected based on the nation’s level of income. Belize falls into the “very bad” category when evaluating the right to reproductive health because the nation is fulfilling only 63.2% of what the nation is expected to achieve based on the resources (income) it has available.
Source:https://en.wikipedia.org/wiki/Healthcare_in_Belize
- GLOBAL PRETERM BIRTH RATES – Belize
- Estimated # of preterm births: 12.6 per 100 live births
- (Global Average: 10.6)
- Source- WHO Preterm Birth Rate (Per 100 Live Births)

COMMUNITY
Longest continuously running study on preterm birth that has followed research participants for more than 35 years published in JAMAURI College of Nursing Professor Amy D’Agata’s study shows that the effects of preterm birth can linger throughout an individual’s lifetime, necessitating the inclusion of birth history in adult health records.
KINGSTON, R.I. — August 4, 2025 — The stress preterm infants experience at birth can carry on throughout a lifetime and cause negative health impacts later in life, necessitating the routine inclusion of birth history in medical records and the development of clinical guidelines for adults born preterm, the longest continuously running study of individuals born preterm in the United States has shown.
University of Rhode Island College of Nursing Professor Amy D’Agata is continuing the work that began in the 1980s with a group of babies born preterm at Women & Infants Hospital. Involving 215 people born 35 years ago—including a control group of full-term babies, and preterm babies born at 22 to 36 weeks—the study tracks the successes and difficulties preterm babies continue to face into adulthood, and compares them to the group of participants born full term. The project has so far garnered more than $10 million in research grant funding.
D’Agata, who took over as principal researcher after the retirement of Professor Emeritus Mary Sullivan, has published the most recent results in the Journal of the American Medical Association. The published paper focuses physiological and psychological health outcomes that D’Agata and her team of researchers have identified as the study participants approach 40 years old. Those born preterm have shown a higher risk of high blood pressure, high cholesterol, increased abdominal fat, and low bone density. Psychologically, the group tends to internalize problems, often resulting in increased levels of depression and anxiety.
“Preterm birth is not just a neonatal issue. It, in fact, is a lifelong condition,” D’Agata said the study shows. “For individuals who have medical complications early in life, we are now seeing an increased risk of different chronic health issues later in life. We are now realizing that there is a very strong link between what happens to you early in life and later health outcomes.”
The study offers important takeaways for health-care clinicians, who are not always aware a patient was born preterm because birth history is not commonly included in adult medical records. D’Agata’s study is showing the need to include the information, and to develop adult screening guidelines for individuals who have a history of preterm birth. The work is also helping people who have been impacted by preterm birth understand that their birth history should be included in their medical records and should be considered in the context of their overall health.
“In this country, millions of people born preterm have grown into adulthood and are now seeing clinicians across primary care and various specialties, yet providers rarely ask about birth history,” D’Agata said. “We are urging that birth history be included as a standard question on every adult intake form. Health cannot be fully optimized if we overlook such a critical assessment piece.
Understanding an individual’s birth history, alongside growing research identifying increased health risks for those born preterm and the development of targeted clinical guidelines, will advance health equity for survivors of early birth. We believe a paradigm shift is needed in health care that recognizes preterm birth as a chronic condition requiring lifelong monitoring and support.”
While the study’s most recent results were just published in JAMA Network Open in July, D’Agata is already looking toward the next set of findings. Continuing to work with fellow URI professor Justin Parent, D’Agata is examining epigenetic age acceleration among individuals born preterm. Understanding any differences in epigenetic aging that may exist between preterm and full-term born adults may be another approach to understanding long-term health.

In the heart of the Cuban capital, the Dr. Cosme Ordoñez Carceller Teaching Polyclinic stands as a testament to the nation’s unique approach to healthcare: universal, free of charge, accessible, regionalized, community-centered, and deeply rooted in preventive medicine. Unlike the profit-driven models that dominate much of the world, Cuba’s system prioritizes equitable access, public health education, and early intervention.
At the core of this approach is a commitment to health promotion through education, disease prevention through habit management, and the integration of medical care and rehabilitation. By emphasizing proactive healthcare rather than reactive treatment, the system ensures that communities receive continuous, comprehensive support to maintain overall well-being.
During a recent visit to the Dr. Cosme Ordoñez Carceller Teaching Polyclinic in Havana, the staff detailed how the system was developed and how it ensures that no Cuban, regardless of income, is left without medical care.
The structure of Cuba’s healthcare system
Cuba’s National Health System operates as a hierarchical, state-run model designed to ensure seamless coordination of care. At the top, the National Assembly oversees the Ministry of Public Health, which sets national policies and directs specialized health institutes that tackle broader public health concerns.
Below the Ministry, provincial governments, answering directly to the Assembly, oversee provincial health departments, which manage larger hospitals and specialized medical facilities. These provincial bodies, in turn, delegate responsibilities to municipal governments, which run the municipal health departments and smaller hospitals that serve local populations. At the community level, municipal health departments manage Cuba’s extensive polyclinic network, the cornerstone of the country’s healthcare system. These polyclinics not only provide specialized care, diagnostics, and emergency services, but they also coordinate closely with family doctor-and-nurse teams, who serve as the first point of contact for Cuban citizens.
These frontline providers play a crucial role beyond immediate treatment, emphasizing preventive care, home visits, and alternative therapies such as nutrition counseling, acupuncture, and plant-based medicine. Despite supply shortages exacerbated by US sanctions, this integrated, top-down approach ensures that resources are distributed efficiently, maintaining consistent healthcare access nationwide.
Founded in 1974, the Dr. Ordoñez Carceller Polyclinic serves approximately 13,000 residents, offering care in medical specialties such as cardiology, orthopedics, fertility consultations, and genetic testing. The clinic is named after Dr. Cosme Ordoñez Carceller (1927–2019), an epidemiologist and pioneer of Community Medicine, who championed the polyclinic model that emerged in the 1960s and 1970s. He played a key role in training young physicians in comprehensive general medicine and launched innovative programs like the Grandparents’ Circles, a senior care initiative so effective that it was replicated nationwide.
Cuba’s system prioritizes equitable access, public health education, and early intervention. The country’s healthcare approach is rooted in promoting health through education, preventing disease by managing habits, and ensuring comprehensive medical care and rehabilitation. Unlike the fragmented, for-profit US healthcare model, Cuba’s integrated, community-based approach ensures better health outcomes and higher patient satisfaction. At polyclinics like Ordoñez Carceller, primary care is not just about treating illness but about education, prevention, and holistic well-being. This commitment to accessible, people-centered medicine reflects Cuba’s broader philosophy: that healthcare is not a privilege, but a fundamental human right.
Cuba’s healthcare achievements: A global leader in public health
Despite enduring over six decades of economic embargo, Cuba has achieved remarkable public health milestones. The following list highlights key accomplishments of both the Ordoñez Carceller Polyclinic and the Cuban healthcare system as a whole:
- AIDS: Cuba identified HIV in 1983 and quickly set up a system to track and treat it. By 2014, it eliminated mother-to-child transmission of HIV and syphilis, a milestone the US has yet to reach.
- COVID: Cuba developed two COVID vaccines, kept infections low, and even sent vaccines abroad.
- Diabetes: The nation has developed an effective medication that treats diabetic ulcers (skin wounds that result from poor blood sugar control)
- Alzheimer’s research: Cuba developed a drug that may help reverse Alzheimer’s effects
- Maternal-fetal medicine: 99% of Cuban children are vaccinated, and the country has a lower infant mortality rate than the US
- Nutrition: While obesity is not an issue in Cuba, malnutrition is an increasing concern due to shortages caused by the US embargo
- Home health Doctors make house calls to care for the elderly and new mothers.
Profit vs. public health: How medical education and healthcare delivery differ in Cuba and the US
The paths to becoming a doctor in Cuba and the United States could not be more different. In the US, medical students take on crippling debt, often exceeding USD 200,000, before ever treating a patient. The pressure to repay loans steers many toward high-paying specialties, leaving primary care and rural communities underserved. The system is structured around financial incentives rather than public need, reinforcing the idea that medicine is a business first, a service second.
Cuba takes the opposite approach. Medical education is fully state-funded, allowing students to focus on patient care instead of profit. Training begins immediately after secondary school, with students placed in community clinics early in their careers. By the time they specialize, they have already served in primary care settings, ensuring that the system produces physicians committed to public health, not private wealth.
A focus on prevention, not just treatment
Cuba’s prevention-first model stands in stark contrast to the reactive nature of US healthcare. While American medicine often prioritizes treatment over lifestyle interventions, Cuban doctors routinely incorporate nutrition, exercise, and disease prevention strategies into care plans. The country’s polyclinic system ensures patients receive consistent, community-based healthcare rather than navigating a fragmented, for-profit system that often leaves them behind.
The US blockade: An unjust barrier to health
The US embargo continues to hinder Cuba’s healthcare system by restricting access to essential medicines, medical equipment, and scientific research. Pharmaceutical and shipping companies, fearing US penalties, avoid business with Cuba—leading to severe shortages of everything from aspirin to cancer treatments.
Even medical journals and online resources are blocked due to US restrictions, forcing Cuban researchers to work under constraints that most Western physicians never encounter.
Yet, rather than succumbing to these barriers, Cuba has turned to self-sufficiency, investing in biotechnology, vaccine development, and herbal medicine research to compensate for limited imports. If freed from economic sanctions, Cuba’s contributions to global healthcare innovation could expand exponentially.
For decades, Cuba has exported medical expertise worldwide, sending doctors to disaster-stricken and underserved regions. These global medical brigades have provided care to millions, particularly in Latin America, Africa, and the Caribbean. Yet, rather than supporting these humanitarian efforts, Washington has sought to dismantle them. In February 2025, the US expanded sanctions on Cuba’s international medical program, further restricting its ability to send doctors abroad. The move reflects a deeper failure to understand Cuba’s model of solidarity-driven healthcare, a stark contrast to the US system, where medicine is often dictated by profit rather than public service.
It is within this profit-driven framework that Cuba’s medical missions are misunderstood, labeled as “forced labor” by those who cannot imagine doctors choosing service over salary. The very idea of healthcare as a human right, rather than a commodity, challenges the US worldview, leading to efforts to discredit and sanction those who practice it differently.
What could be if the embargo were lifted
Cuba’s healthcare system is a model of resilience and innovation, but its full potential remains hindered by decades of US sanctions. If given access to global resources and technology, Cuban researchers could expand medical advancements in infectious diseases, chronic illness treatment, and disaster response. For now, Cuban doctors continue their work—undaunted by external pressures, committed to the principle that healthcare is a right, not a privilege.
People’s Health Dispatch is a fortnightly bulletin published by the People’s Health Movement and Peoples Dispatch. Renée L. Quarterman, MD, FACS, is a surgical breast specialist. She is the director of Delaware Breast Care, a part of US Oncology.

HEALTHCARE PARTNERS


Quality improvement (QI) initiatives have become essential to advancing patient outcomes in the neonatal intensive care unit (NICU), where high acuity and complex care are the norms. NICU nurses are uniquely positioned to find inefficiencies, propose practical solutions, and drive meaningful change. However, despite the growing emphasis on QI in nursing practice, well-intentioned projects fall short due to avoidable missteps in the planning and execution phases.
The following guide can be utilized by NICU nurses to navigate through common pitfalls in QI research and offers evidence-based strategies to overcome them. By focusing on foundational principles and real-world examples, this guide supports nurses in conducting impactful, sustainable QI work that enhances neonatal outcomes and team collaboration.
Common Pitfalls in QI Research
Lack of Clear Problem Definition
A common pitfall in QI efforts is the failure to define the problem thoroughly. Without a precise understanding of the issue, teams may invest critical time and resources into solutions that do not address the root cause.
For instance, a unit may notice an uptick in central line-associated bloodstream infections (CLABSIs) and immediately implement new sterile techniques without investigating the underlying variables. Was the increase related to staffing changes, procedural drift, or equipment issues? Without a clear problem definition, interventions risk being misaligned or ineffective.
Strategy: Use structured problem-identification tools—such as root cause analysis (like the Five Whys) or fishbone diagrams—to uncover deeper system issues. Frame the problem in a way that is specific, data-informed, and agreed upon by stakeholders. A clearly defined problem becomes the foundation for targeted and measurable interventions.
Neglecting Stakeholder Involvement
Successful QI initiatives require input and collaboration across disciplines. A common misstep occurs when projects are developed in isolation, often without input from those who will implement or be affected by the change. This can lead to resistance, logistical challenges, or unintended consequences.
For example, consider a QI team aiming to improve feeding initiation times by adjusting nursing workflows. If respiratory therapists or neonatal physicians are not consulted, the new protocol might inadvertently clash with intubation or stabilization practices, resulting in delays rather than improvements.
Strategy: Identify all stakeholders early in the project, including nurses, physicians, respiratory therapists, pharmacists, and families, when appropriate. Conduct stakeholder analyses and engage representatives in project design and testing phases. Inclusive collaboration fosters ownership, smoother implementation, and more sustainable outcomes (Institute for Healthcare Improvement, n.d.).
Poorly Defined Metrics
Without clearly defined, relevant, and measurable outcomes, a QI initiative’s impact is difficult to assess. Broad or vague goals such as “improve thermoregulation” fail to provide direction or an evaluation method.
Strategy: Use SMART goals—Specific, Measurable, Achievable, Relevant, and Time-bound—to guide metric development. For instance, instead of aiming to “reduce hypothermia,” a SMART goal might be: “Increase the percentage of newborns with normothermic admission temperatures (36.5°C–37.5°C) from 65% to 90% over six months.” Tools and resources are available to learn how to develop clear metrics, help track progress, guide adjustments, and communicate results to the team and leadership (Agency for Healthcare Research and Quality, 2020).
Inadequate Data Collection Planning
Even well-designed projects can falter without a strong plan for data collection. Inconsistent, incomplete, or biased data limit the ability to draw valid conclusions and make informed decisions.
Strategy: Design a standardized data collection process before the intervention begins. Identify what data are needed, who will collect data, how often, and how data will be stored and analyzed. Use validated tools where possible and use the electronic health record (EHR) system to reduce manual workload and increase reliability. Pilot test the data collection process to identify issues before scaling up.
Failure to Pilot Interventions
Another frequent misstep is implementing large-scale changes without first evaluating them in a controlled way. Skipping the pilot phase can lead to disruptions in care, staff confusion, or overlooked safety concerns.
Strategy: Use Plan-Do-Study-Act (PDSA) cycles to test changes on a small scale. For instance, a new bedside handoff tool can be trialed with one team for over a week before expanding unit wide. Piloting helps refine interventions, identify barriers early, and build staff confidence.
Lack of Sustainability Planning
Often, improvement is easier to achieve than sustain. QI initiatives can experience initial success but not maintain gains over time due to a lack of follow-up, ownership, or integration into routine practice.
Strategy: Plan for sustainability from the outset. Embed new practices into policies, electronic systems, and training programs. Assign champions to monitor compliance, provide feedback, and adapt as needed. Ongoing measurement and leadership support are critical to prevent regression.
Not Sharing or Publishing Results
When results are not shared beyond the unit, valuable insights and lessons are lost. This limits the potential for broader impact and professional growth.
Strategy: Disseminate findings through presentations, newsletters, or professional journals. Even small projects can inspire similar efforts elsewhere and contribute to the collective advancement of neonatal care. Sharing also strengthens the culture of learning and improvement.
Better QI Creates Lasting Change
Quality improvement is a powerful tool NICU nurses use to enhance care and outcomes. By avoiding common pitfalls—such as unclear problem definitions, poor metric planning, and lack of sustainability—nurses can lead effective and lasting change. Through structured planning, collaborative engagement, and thoughtful execution, every QI effort becomes an opportunity for growth and better care for our most vulnerable patients. (Institute for Healthcare Improvement, n.d.).
Source: https://nann.org/publication/feature-34/
Ghosting is one of those terms that seem out of place in medicine, borrowed from social media and dating culture. However, the phenomenon itself is alive and well in our clinical ecosystems. In fact, medicine may be one of the most fertile environments for it. How else can someone remain deeply involved, wholly committed, ever-present in the work, yet increasingly pushed to the side, rendered peripheral to decisions they once shaped?
In the professional world, ghosting is less dramatic and more insidious. It is not someone vanishing; it is colleagues stepping around them. It is conversations that slip behind closed doors. It is the rise of intermediaries and buffers. It is the subtle but unmistakable shift from direct speech to third-person references. It is the choice to go around rather than through.
It is ostracizing, but with a veneer of civility. It is quiet exclusion disguised as efficiency.
And yes, it does not feel very good. For many, the experience intensifies with seniority. The more seasoned someone becomes, the more they know, the more institutional memory they carry, the more perspective they bring; the easier it becomes for others to rationalize keeping them out of the loop. People frame it as respect, as courtesy, as a desire not to “burden” them. Nevertheless, the line between courtesy and dismissal is thin and often crossed.
Technology, ironically, amplifies the problem. Zoom, Teams, and the creeping normalization of AI presence create new pathways for invisibility. What once required the discomfort of face-to-face avoidance now happens silently. Disengagement becomes frictionless. They can be physically present on a screen and still be utterly alone in the room. When they realize they are the only one who showed up in person, while everyone else has delegated their attendance to an AI proxy, they feel the ghostliness in full.
Ghosting rarely begins with an attack. It begins with a narrative.
“They’re too busy for this.”
“They have so much on their plate already.”
“They’re so senior; we shouldn’t bother them with this.”
“They don’t need feedback—they’re above the evaluators.”
What begins as deference quietly morphs into distance. And distance, unchecked, hardens into exclusion. Soon, the storyline shifts:
“They’re not involved.”
“They didn’t attend the last meeting.”
“They never weigh in anymore.”
What remains unsaid and often unnoticed is that no one invited them, no one asked for their opinion, and no one created space for them to be part of the process.
Decisions move forward. Processes evolve. Incentives and priorities shift. Meanwhile, the ghosted clinician continues to do their work, unaware that the landscape is changing around them in ways that diminish their role, complicate their tasks, or diminish their influence. When they finally recognize that something fundamental has shifted, it is often too late to re-enter the conversation.
What does this feel like? It feels exactly like being a ghost.
The film The Sixth Sense offers a powerful metaphor. (Spoiler Alert) Bruce Willis’s character, after suffering a fatal gunshot wound, continues living as though nothing has changed. He goes to work, he engages in therapy, and he attempts to connect with his wife. However, something is off. People drift away. His wife is distant. Rooms feel colder. It is only through his sessions with a child who can “see dead people” that he finally confronts the truth: he is no longer part of the living world, no longer part of the relationships he believes himself to be nurturing.
Professionally, the comparison is not perfect, but it is evocative. In medicine, the “ghosts” have not died. They walk our halls. They mentor trainees. They contribute to scholarship. They carry decades of clinical experience. They built the foundations upon which our teams now stand.
Nevertheless, they are treated as if they no longer inhabit the same professional world as everyone else.
Ghosting in medicine is not just a social slight; it is a cultural wound. It erodes respect. It weakens teams. It destroys continuity. It discards institutional memory. It creates unnecessary rifts between generations of clinicians. It deprives trainees of mentorship. It can turn accomplished physicians into isolated figures who continue to serve, but without the acknowledgment or inclusion that sustains service.
Most dangerously, ghosting perpetuates the illusion that this is normal. That it is natural. That it is simply the denouement of a career.
But it does not have to be.
In an era where burnout is widespread, where talent is scarce, and where the wisdom of experience is more valuable than ever, ghosting is a luxury medicine cannot afford. Inclusion is not just good manners: it is good practice. It strengthens teams, enhances decision-making, and honors the very people who paved the way.
So the next time you see a colleague who seems peripheral, someone once central, now slowly fading from the edges of the conversation—pause before stepping around them. Invite them in. Ask their opinion. Keep them part of the fabric of the work. The difference between belonging and ghosthood may hinge on the smallest acts of acknowledgment, the simplest acts of inclusion. Because the ghost you see before you today is not a relic to be ignored; they are a reflection, a warning, of what any one of us might become.
Source: https://neonatologytoday.net/newsletters/nt-nov25.pdf

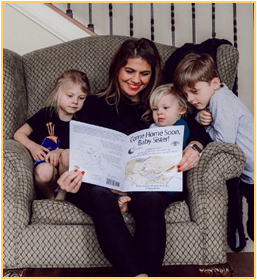
PREEMIE FAMILY PARTNERS
Key Points
At well-baby visits, your baby’s provider checks your baby’s health and development and gives your baby vaccinations to protect them from diseases.
If your baby has a medical condition, they may need ongoing care from different healthcare providers.
If you think your baby is sick, call their provider. If you think it’s an emergency, call 911.
If your baby needs medicine or medical equipment at home, learn how to give or use it correctly before your baby leaves the NICU.
When does your baby need to see their healthcare provider?
Your baby will get several checkups (well-baby visits) with their provider during their first year. At each visit, talk to their provider to make sure your baby’s developing in a healthy way. Are they rolling over, sitting up, crawling, and walking when they should? These skills are called developmental milestones. You may need to remind the provider that your baby spent time in the neonatal intensive care unit (NICU), because this may affect when they reach the milestones.
Take your baby’s medical file to your first visit with your baby’s provider. This file includes their discharge summary and other information from the hospital. The provider needs to know what happened during and after your baby’s birth. Hospital staff may send the summary directly to the provider.
If your baby has a medical condition, such as a birth defect, they may need ongoing care from different healthcare providers. Find a way to keep track of your baby’s medical appointments. This may be on a calendar in your kitchen or on your phone with an alert to remind you. Decide if it’s easier to schedule a few appointments on the same day or spread them out over different days.
Ask your providers to keep your baby’s main provider up to date about all visits and treatments. This helps make sure that all members of your baby’s healthcare team have the same information.
Keep your own record of any checkups, tests, and treatments your baby has had. When your doctor makes a change to your baby’s care or medication, make sure this is also shared with your baby’s in-home nursing care agency and equipment company if you use these services.
What should you do if your baby gets sick?
All babies get sick from time to time. But babies who were in the NICU are more likely than other babies to get infections. Watch for signs that your baby may be sick so you can get medical help right away. You should call your baby’s healthcare provider if your baby:
- Looks blue around the nose, lips, or on the skin, or is paler than usual
- Refuses to eat or doesn’t eat enough
- Throws up (which is more serious than spitting up or reflux)
- Has less than five wet diapers in a 24-hour period, or has diarrhea for more than a day
- Has a large or hard belly that they have not had before
- Has a temperature higher than 100.4 F or lower than 97 F (using a rectal thermometer)
- Has apnea or trouble breathing. Apnea is when the baby stops breathing for 15 seconds or more.
You know your baby best. If you think something is wrong, call their provider, call 911, or take your baby to the emergency room.
How do vaccinations help protect your baby?
All babies, including those who spend time in the NICU, need vaccinations to help protect them from serious diseases. Some babies start getting these shots while they’re in the NICU. Check with your baby’s provider about when they need their vaccinations. Keep a record of your baby’s vaccinations in your medical file for them.
If you have other children, they need their vaccinations, too. This helps keep them from passing infections to the baby. During flu season, everyone in the family, including parents, should get a flu shot. Any adult who may have contact with your baby also needs a Tdap vaccination. This vaccination helps protect against tetanus, diphtheria, and pertussis (whooping cough). If you didn’t receive your Tdap vaccine during pregnancy, you can get it after you’ve given birth. To create a safe space for your baby, it is important for everyone who will be in contact with your baby to receive their vaccinations.
How can you protect your baby from respiratory syncytial virus (RSV)?
RSV is a common virus. It affects almost all children before they reach age 2. Most of the time, it causes a slight cold. But for preterm babies (born before 37 weeks of pregnancy), this virus can be more serious. Babies born preterm or who have heart or lung problems may benefit from a medicine to keep them from getting RSV. Ask your baby’s healthcare provider if your baby got this medicine in the NICU or if they should get it now that they’re at home.
What do you need to know about giving your baby medicine?
Some babies go home from the NICU still taking medicines. Learn how to give your baby their medicine before they leave the hospital. Write down all the directions. If you have questions or are worried about giving your baby medicine, tell the nurse or other NICU staff. They can show you exactly what to do so you feel comfortable and confident about giving your baby medicine.
When giving your baby medicine, make sure you know:
- Where you can get the prescription filled (at a grocery store, drug store, or pharmacy). A prescription is an order for medicine given by a healthcare provider.
- How much medicine to give, how often to give it, and when to stop giving it
- If you can give it before, during, or after feedings
- If the medicine needs to be refrigerated, prepared, or mixed
- What to do if you miss a dose
- If your baby needs more than one medicine, if you can give them together at the same time
You also need to know:
- What position your baby should be in to take the medicine
- What to do if your baby spits up or vomits the medicine
- If there are side effects from the medicine and what to do if your baby has them
To track your baby’s different medicines and when to give them, use a chart. Ask the nurse to help you make the chart.
How can you manage your baby’s medical equipment at home?
If your baby has medical equipment at home, this can feel like a lot to manage. Staying organized and planning ahead can help. Keep a list of your baby’s equipment and medical supplies, including order numbers, size, and quantity. The equipment company can give you a checklist. Be sure to re-order supplies with enough time, as shipments can sometimes be delayed. Always be prepared when you leave the house, make sure you have your baby’s supplies even when you’re just going to the park.
If the equipment uses electricity:
- Share information about your baby’s medical condition with your local fire department and emergency or first responders so they know what to expect in case they’re called to your home for an emergency. Invite them to come to your home to meet you and your baby.
- Contact your utility companies to let them know your baby’s healthcare needs. They may have a priority list for repairing power outages or plowing snow.
- Make a plan for if the power goes out. Have back-up batteries and know how long they will last.
Last reviewed April 2025: https://www.marchofdimes.org/find-support/topics/neonatal-intensive-care-unit-nicu/continuing-medical-care-after-nicu
Anxiety is another word for feeling worried or scared. It’s normal for children and teens to feel anxious sometimes, like before a big test at school or talking in front of a group of people. But if your child’s anxiety gets in the way of normal activities, such as sleeping alone at night, playing outside or going to school, they may need extra support.
The good news is that there are things you can do to help prevent your child from feeling anxious and help them handle worries when they happen. Talk with your pediatrician to discuss strategies and tips that can help.
What are some common signs of anxiety in children?
If your child is feeling anxious, they may not be able to tell you. Your child may feel bad or sick without knowing why, or you may notice they seem restless or tired.
- Feeling as if their heart is racing
- Sweating or blushing
- Shaking or feeling sick to their stomach
- Feeling very cold or hot
- Trouble paying attention or sitting still
- Touching the crotch area (for young boys)
How can I help my child manage anxiety at home?
These tips are helpful for all children, but they can be especially helpful for children with anxiety. Parenting is a busy job, so use your judgment about which tips make the most sense for your family.
Connect with your child
- Set aside one-on-one time every day without TV or other media. Even just 10 minutes each day can make a big difference. Try gardening or taking care of houseplants, drawing or going for a bike ride.
- Praise your child and make them feel good about themselves. For example, “You did a great job on that homework assignment!” or “Thank you for helping me with the laundry. I’m so lucky to have your help.”
- Find out what’s worrying your child, because stress can make them feel anxious. Things such as being bullied at school, divorce, or a death in the family can make a child feel anxious. Your child may need extra help to handle issues such as these.
Help your child learn to manage fears
When your child is calm, start a conversation about things they can do to manage fears and worries when they happen. For example, let them know that they can
- Practice deep breathing and muscle relaxation.
- Use positive self-talk (for example, “I can try this” instead of “I can’t do this”).
- Think of a safe place, such as their bedroom or favorite place outdoors.
- Gradually facing fears. Consider gradually exposing your child to feared objects or activities.
- Praise and reward brave behavior: the goal is to cope, not avoid.
Build healthy habits to support mood
Healthy lifestyle habits can help reduce stress and support a positive mood.
- Get active! Encourage your child to be active for at least an hour every day. This activity can include playing outside, joining a sports team or an activity at the YMCA, biking or walking to school, or dancing at home to favorite music.
- Eat healthy. Eat healthy meals every day, including fruits and vegetables, whole grains, and protein foods. Remember to eat breakfast!
- Get plenty of sleep. School-aged children need 9 to 12 hours of sleep every night, and teens need 8 to 10 hours.
- Build a family media plan to set healthy guidelines around entertainment screen time. Avoid scary or violent TV shows, video games, and movies.
- Set up family routines. Follow a regular schedule for playtime, mealtime, and bedtime. Knowing what to expect can help your child feel safe and secure.
How can I help my child manage school anxiety?
Children may find it hard to focus on or even go to school when they’re feeling worried. If your child is having trouble in school, try these ways to help.
- Gently but firmly tell your child why it’s important to go to school.
- Talk with your child’s teachers and the guidance counselor about what to do if your child asks to go home from school early.
- If you think your child may be upset by family stress or pressure to do well in school, let them know they are doing a good job and you’re proud of them.
- Help your child set realistic goals for school. If they set goals that are too hard to meet, they may feel worse about themselves.
- Remind your child that they can take steps to control their worries. For example, they can think about what to do ahead of time to handle a stressful situation.
- Reward your child’s brave behaviors at school. Spending time doing fun activities with a parent is a very powerful reward.
Remember, you know your child best.
Whether it’s at school or the doctor’s office, you are your child’s biggest advocate. Don’t hesitate to speak up on behalf of your child.
When do I need to go back to the doctor?
If your child’s anxiety doesn’t go away or gets worse, get back in touch with the doctor. You and the doctor can make a plan to try new approaches or strategies with your child.
It’s especially important to talk with your child’s doctor if:
- Your child starts to experience other behavior problems, such as shyness.
- Something scary happens in your child’s life that may make their anxiety worse, such as an injury or death in the family.
- You suspect your child’s anxiety is affecting another medical condition (for example, if your child’s asthma gets worse with anxiety).
The doctor can also help you decide whether visiting a specialist may help. For example, a type of therapy called cognitive behavioral therapy can be helpful for children with anxiety.
Make time to care for yourself, too.
Parenting can be stressful. If you’re feeling overwhelmed, don’t be afraid to ask for support from family, close friends, social services, or your faith community. Children pick up on the stress and worries of adults, so getting support for yourself can help your child too.
Last Updated – 09/24/2024 –https://www.healthychildren.org/English/family-life/family-dynamics/Pages/help-your-child-manage-fears-and-anxieties.aspx
The neonatal intensive care unit (NICU) is a special unit in the hospital for babies born preterm, very early, or who have some other serious medical condition. Most babies born very early will need special care after birth. This is done by or under the supervision of a neonatologist, a doctor with special training in the care and problems of newborns.
This article discusses the consultants and support staff who may be involved in the care of your infant depending on your infant’s specific medical needs.
Information
AUDIOLOGIST
An audiologist is trained to test a baby’s hearing and provide follow-up care to those with hearing problems. Most newborns have their hearing screened before leaving the hospital. Your health care providers will determine which hearing test is best. Hearing tests may also be done after leaving the hospital.
CARDIOLOGIST
A cardiologist is a doctor that has special training in the diagnosis and treatment of heart and blood vessel disease. Pediatric cardiologists are trained to deal with newborn heart problems. The cardiologist may examine the baby, order tests, and read test results. Tests to diagnose heart conditions may include:
If the structure of the heart is not normal due to a birth defect, a cardiologist might work with a cardiovascular surgeon to perform surgery on the heart.
CARDIOVASCULAR SURGEON
A cardiovascular (heart) surgeon is a doctor who has special training in doing surgery to correct or treat defects of the heart. Pediatric cardiovascular surgeons are trained to deal with newborn heart problems.
Sometimes, surgery can correct a heart problem. Other times, complete correction is not possible and surgery is done just to make the heart work as well as possible. The surgeon will work closely with the cardiologist to care for the baby before and after surgery.
DERMATOLOGIST
A dermatologist is a doctor who has special training in diseases and conditions of the skin, hair, and nails. Such a doctor might be asked to look at a rash or skin lesion on a baby in the hospital. In some cases, the dermatologist might take a sample of the skin, called a biopsy. The dermatologist might also work with the pathologist to read the biopsy results.
DEVELOPMENTAL PEDIATRICIAN
A developmental pediatrician is a doctor who has been specially trained to diagnose and care for infants who have trouble doing what other children of their age can do. This type of doctor often evaluates babies who have already gone home from the NICU and will order or perform developmental tests. The doctor can also help you find resources near your home that provide therapies to help infants and children in meeting development milestones. Developmental pediatricians work closely with nurse practitioners, occupational therapists, physical therapists, and sometimes neurologists.
DIETITIAN
A dietitian has special training in nutritional support (feeding). This type of provider may also specialize in pediatric (children’s) nutritional care. Dietitians help determine if your baby is getting enough nutrients, and may recommend some choices of nutrition that can be given through the blood or a feeding tube.
ENDOCRINOLOGIST
A pediatric endocrinologist is a doctor with special training in the diagnosis and treatment of infants with hormone problems. Endocrinologists might be asked to see babies who have problems with the level of salt or sugar in the body, or who have problems with the development of certain glands and sexual organs.
GASTROENTEROLOGIST
A pediatric gastroenterologist is a doctor with special training in the diagnosis and treatment of infants with problems of the digestive system (stomach and intestines) and liver. This type of doctor might be asked to see a baby who has digestive or liver problems. Tests, such as x-rays, liver function tests, or abdominal ultrasounds, might be done.
GENETICIST
A geneticist is a doctor with special training in the diagnosis and treatment of infants with congenital (inherited) conditions, including chromosomal issues or syndromes. Tests, such as chromosome analysis, metabolic studies, and ultrasounds, may be done.
HEMATOLOGIST-ONCOLOGIST
A pediatric hematologist-oncologist is a doctor with special training in the diagnosis and treatment of children with blood disorders and types of cancer. This type of doctor might be asked to see a baby for bleeding problems due to low platelets or other clotting factors. Tests, such as a complete blood count (CBC) or clotting studies, might be ordered.
INFECTIOUS DISEASE SPECIALIST
An infectious disease specialist is a doctor with special training in the diagnosis and treatment of infections. They might be asked to see a baby that develops unusual or serious infections. Infections in babies can include blood infections or infections of the brain and spinal cord.
MATERNAL-FETAL MEDICINE SPECIALIST
A maternal-fetal medicine doctor (perinatologist) is an obstetrician with special training in the care of high-risk pregnant women. High-risk means there is an increased chance for problems. This type of doctor can care for women who have premature labor, multiple gestations (twins or more), high blood pressure, or diabetes.
NEONATAL NURSE PRACTITIONER (NNP)
Neonatal nurse practitioners (NNP) are advanced practice nurses with extra experience in the care of newborn infants in addition to completing master’s or doctoral level educational programs. The NNP works along with a neonatologist to diagnose and treat health problems in babies in the NICU. The NNP also performs procedures to help diagnose and manage certain conditions.
NEPHROLOGIST
A pediatric nephrologist is a doctor with special training in diagnosing and treating children who have problems with the kidneys and urinary system. This type of doctor might be asked to see a baby who has problems in the development of the kidneys or to help care for a baby whose kidneys do not work properly. If a baby needs kidney surgery, the nephrologist will work with a surgeon or urologist
.NEUROLOGIST
A pediatric neurologist is a doctor with special training in the diagnosis and treatment of children with disorders of the brain, nerves, and muscles. This type of doctor might be asked to see a baby who has seizures or bleeding in the brain. If the infant needs surgery for a problem in the brain or spinal cord, the neurologist might work with a neurosurgeon.
NEUROSURGEON
A pediatric neurosurgeon is a doctor trained as a surgeon who operates on children’s brains and spinal cords. This type of doctor might be asked to see a baby who has problems, such as spina bifida, skull fracture, or hydrocephalus.
OBSTETRICIAN
An obstetrician is a doctor with special training in taking care of pregnant women. This type of doctor might also assist women who are trying to get pregnant and follow women with medical conditions, such as diabetes or decreased fetal growth.
OPHTHALMOLOGIST
A pediatric ophthalmologist is a doctor with special training in diagnosing and treating eye problems in children. This type of doctor might be asked to see a baby who has birth defects of the eye.
An ophthalmologist will look at the inside of the baby’s eye to diagnose retinopathy of prematurity. In some cases, this type of doctor might perform laser or other corrective surgery on the eyes.
ORTHOPEDIC SURGEON
A pediatric orthopedic surgeon is a doctor with special training in the diagnosis and treatment of children who have conditions involving their bones. This type of doctor might be asked to see a baby who has birth defects of the arms or legs, hip dislocation (dysplasia), or fractures of the bones. To see the bones, orthopedic surgeons might order ultrasounds or x-rays. If needed, they can perform surgery or place casts.
OSTOMY NURSE
An ostomy nurse is a nurse with special training in the care of skin wounds and openings in the belly area through which the end of the intestine or the collecting system of the kidney stick out. Such an opening is called an ostomy. Ostomies are the result of surgery needed to treat many intestinal problems, such as necrotizing enterocolitis. In some cases, ostomy nurses are consulted to help care for complicated wounds.
OTOLARYNGOLOGIST/EAR NOSE THROAT (ENT) SPECIALIST
A pediatric otolaryngologist is also called a pediatric ear, nose, and throat (ENT) specialist. This is a doctor with special training in the diagnosis and treatment of children with problems with the ear, nose, throat, and airways. This type of doctor might be asked to see a baby who has problems with breathing or a blockage of the nose.
OCCUPATIONAL/PHYSICAL/SPEECH THERAPISTS (OT/PT/ST)
Occupational and physical therapists (OT/PT) are professionals with advanced training in working with infants with developmental needs. This work includes neurobehavioral assessments (postural tone, reflexes, movement patterns, and responses to handling). In addition, the OT/PT professionals will help determine a baby’s nipple-feeding readiness and oral-motor skills. Speech therapists will also help with feeding skills in some centers. These types of providers might also be asked to provide family education and support.
PATHOLOGIST
A pathologist is a doctor with special training in lab testing and examination of body tissues. They supervise the lab where many medical tests are performed. They also examine tissues under the microscope that are obtained during a surgery or an autopsy.
PEDIATRICIAN
A pediatrician is a doctor with special training in the care of infants and children. This type of doctor might be asked to see a baby in the NICU, but is usually the primary care provider for a healthy newborn. A pediatrician also provides primary care for most babies after they leave the NICU.
PHLEBOTOMIST
A phlebotomist is a specially trained professional who takes your blood. This type of provider may take the blood from a vein or a baby’s heel.
PULMONOLOGIST
A pediatric pulmonologist is a doctor with special training in diagnosing and treating children with respiratory (breathing) conditions. Even though the neonatologist cares for many infants with respiratory problems, the pulmonologist might be asked to see or to help care for babies who have unusual conditions of the lung.
RADIOLOGIST
A radiologist is a doctor with special training in obtaining and reading x-rays and other imaging tests, such as barium enemas and ultrasounds. Pediatric radiologists have extra training in imaging for children.
RESPIRATORY THERAPIST (RT)
Respiratory therapists (RTs) are trained to deliver multiple treatments to the heart and lungs. RTs are actively involved with babies having breathing problems, such as respiratory distress syndrome or bronchopulmonary dysplasia. An RT might become an extracorporeal membrane oxygenation (ECMO) specialist with further training.
SOCIAL WORKERS
Social workers are professionals with special education and training to determine the psychosocial, emotional, and financial needs of families. They help families find and coordinate resources in the hospital and community that will help to meet their needs. Social workers also help with discharge planning.
UROLOGIST
A pediatric urologist is a doctor with special training in diagnosing and treating conditions involving the urinary system in children. This type of doctor might be asked to see a baby with conditions such as hydronephrosis or hypospadias. With some conditions, they will work closely with a nephrologist.
X-RAY TECHNICIAN
An x-ray technician is trained in taking x-rays. X-rays can be of the chest, stomach, or pelvis. Sometimes, solutions are used to make body parts easier to see, as with barium enemas. X-rays of bones are also commonly performed on babies for a variety of reasons.
Source: https://medlineplus.gov/ency/article/007249.htm
INNOVATIONS
OBJECTIVE
Pediatric surgical conditions are a significant source of morbidity and mortality in low- and middle-income countries (LMICs), where children with surgically treatable conditions lack access to care owing to an insufficient number of pediatric surgeons, poor and limited training, and financial barriers. There is a growing shift from charitable missions to capacity-strengthening projects, which strengthen the skills and resources of communities. The objective of this study was to synthesize the literature to identify capacity-strengthening projects, their methods and outcomes, and their limitations and barriers.
METHODS
MEDLINE, EMBASE, Cochrane, and Web of Science were searched until May 5, 2023. Eligibility criteria were as follows: (1) inclusion of pediatric surgery patients; (2) designation as capacity-strengthening interventions; (3) outcomes of improved access defined through Lancet Commission on Global Surgery Indicators; and (4) designation as an LMIC defined by the World Bank. Two independent reviewers conducted screening and extraction.
RESULTS
A total of 80 studies met inclusion criteria. Interventions were implemented in 69 LMICs and used 19 different methods of capacity strengthening. Common capacity-strengthening methods included the following: international surgical visits, training programs, partnerships, mobile clinics and camps, infrastructure enhancements, and telemedicine. Common methods used included the following: training of local providers, continuous contact between both countries after the visit was completed, improved access for rural families, and economic support for low-income families. A total of 1 357 077 pediatric surgeries were performed through these interventions. Limitations included the fact that only peer-reviewed studies were included. Included studies were mainly case series or small observational studies with qualitative data.
CONCLUSIONS
This review identifies methods to implement capacity-strengthening interventions in LMICs, including their successes and barriers. Future research should report ethical concerns and quantitative outcomes to determine effectiveness.

Introduction
Neonates and infants are commonly referred to as “therapeutic orphans” due to the overall scarcity of therapeutic interventions that have been developed and tailored to their needs and specific characteristics. This is well known by care providers and researchers active in this field, but is perhaps less on the radar of authorities, funding bodies or the broader public. There is significant health inequity when comparing newborns to other age populations in terms of specific drug and device development and therapeutics. In addition there are health inequities in the provision of neonatal care globally which require special attention in terms of improvement.
Bronchopulmonary dysplasia, neonatal seizures, poor growth, necrotizing enterocolitis (NEC) and short bowel, hypoxic-ischemic encephalopathy, retinopathy of prematurity (ROP), neonatal infections and sepsis hereby serve as a non-exhaustive list of “orphan conditions” in need of more equity, through adequately and urgently funded research and improvement.
The good news is that there have been increased efforts, in recent years, by researchers and regulatory bodies to focus on the provision of drugs, devices, and treatment modalities tailored for neonatal use, while further advocacy remains an obvious need . This brings perspective and explains the initiative taken to organize a focused research topic on what is on the horizon as well as recent advances.
Overview of the topics covered
We targeted emerging or new aspects related to monitoring, diagnostics and therapeutics in neonatal care for the current research topic. Fortunately, this research topic was perceived as very relevant by the research community, as 135 authors expressed their interest as contributors, resulting in 20 accepted papers. This serves as a signal of the importance to continue to work on this topic.
Post-hoc, and in a somewhat arbitrary way (because of overlap in these subcategories) these papers were subdivided by the editors into different subcategories, with focus on (1, 5 papers) perinatal biomarkers in blood and urine and how these relate to or predict outcomes, (2, 6 papers) adaptations of existing and newly emerging equipment in neonatal units, (3, 3 papers) needed advances in pharmacotherapy, (4, 3 papers) machine learning or deep learning applications in neonatal care, and finally, (5, 3 papers) underreported aspects of contemporary NICU care, with a focus on the holistic nature of care for the infant and the family.
Perinatal biomarkers in blood and urine and how these relate to or predict outcomes
Two papers focused on biomarkers related to gestational diabetes, with reflections and data on maternal and neonatal outcomes. Postnatal maternal levels of glycated albumin and hemoglobin A1c in mothers of large-for-gestational-age (LGA) informed us of the relevance of accurate diagnosis during pregnancy. This is because postpartum women without diagnosis during pregnancy had higher glycated albumin values, associated with LGA and associated complications (Železnik et al.). Interestingly and related to this paper, Yin et al. reported on a untargeted metabolomics study in women with gestational diabetes, with the recommendation of a maternal serum metabolite panel to forecast neonatal adverse outcomes (hypoglycemia and macrosomia) (Yin et al.).
Other papers focused on the use of vitamin D, acid-base and biomarkers associated with fetal growth restriction with impaired neurodevelopmental outcome. In a cohort of 217 preterm neonates, a multivariate regression analysis identified antenatal steroids as protective, and lower birth weight, duration of ventilation, sepsis and the serum 25-(OH)D vitamin as risk factors to develop ROP (Yin et al.). Musco et al. reported on a systematic review on blood biomarkers indicating risks of adverse neurodevelopmental outcome in fetal growth restricted infants (Musco et al.). While the authors retrieved some data on neuron specific enolase and S100B, the overall conclusions reflect a call for further research. Finally, an association between lactate levels in umbilical cord blood and cerebral oxygenation in preterm neonates was studied as a secondary outcome analysis (Dusleag et al.). In non-asphyxiated preterm neonates with respiratory support, lactate levels were negatively associated with cerebral and arterial oxygenation. In term neonates without respiratory support, no associations were observed.
Adaptations of existing and newly emerging equipment in our units
In a review on emerging innovations in neonatal monitoring, Krbec et al. concluded that there is an urgent, still unmet need to develop wireless, non- or minimal-contact, non-adhesive technology, capable to integrate multiple signals in a single platform, tailored to neonates (Krbec et al.). Related to this call of action, Svoboda et al. reported on their pilot experience with contactless assessment of heart rate, applying imaging photoplethysmography (Svoboda et al.). Rectal and axillary temperature monitoring on admission were compared in a cohort of preterm (n = 80, <32 weeks gestational age) by Halabi et al., reporting that rectal measurement was likely more reliable in the event of hypothermia (Halabi et al.). Ultrasound-guided measurement of anterior cerebral artery resistive index in the first week of life in 739 preterm neonates (<35 weeks) was not associated with subsequent co-morbidities on admission or during neonatal stay (asphyxia, sepsis, NEC) (Singh Gill et al.). A case series of neurally adjusted ventilatory assist to rescue pulmonary interstitial emphysema in 5 extremely low birth weight infants illustrated the potential value of this ventilatory equipment and strategy and need for further study (Chen et al.). Finally, van Rens et al. compared a conventional to a modified Seldinger technique (a dedicated micro-insertion kit) for peripherally inserted central catheter (PICC) placement, illustrating the relevance of developing “low risk, high benefit” type of medical devices, adapted to the specific needs of neonates (van Rens et al.).
Advances needed in pharmacotherapy
The currently available medicines and dosing regimens in neonatal care are limited and there is an urgent need for improvement in this domain. This was illustrated by articles on sepsis, septic shock and steroids. Inequity in provision of neonatal care across the globe ought to be a major focus of improvement. Gezahegn et al. described the outcome in neonates admitted with sepsis in Harar (Ethiopia). Low white blood cell count, desaturation, preterm birth, absence of prenatal maternal care, and chorioamnionitis were important risk factors for sepsis-related mortality (Gezahegn et al.). Addressing these prognostic factors hold the promise to act as levelers to improve outcomes. A pilot study compared noradrenaline and adrenaline as first line vasopressor for fluid-refractory sepsis shock (Garegrat et al.). Both interventions were comparable to resolve the septic shock, while the overall mortality (13/42, 30%) remained significant, highlighting the need for better diagnostic and therapeutic options. Finally, in a systematic review, outcome of postnatal systemic corticosteroids (hydrocortisone to dexamethasone) were compared as reported in randomized controlled trials (Boscarino et al.). The authors concluded that dexamethasone appeared to be somewhat more effective than hydrocortisone in improving respiratory outcomes, but with inconclusive but relevant concerns on the uncertainties on long-term neurodevelopmental outcome, again highlighting the need for better therapies for prevention and management of chronic lung disease of prematurity.
Machine learning or deep learning applications in neonatal care
Artificial intelligence is a rapidly advancing area with fast evolving clinical applications in healthcare, including in the NICU (6). It is no surprise that the current research topic also contains papers illustrating its relevance to improve our practices and outcomes. Two papers hereby focused on NEC, and a 3rd paper on prediction of significant patent ductus arteriosus (PDA). In a mini-review, Cuna et al. reports on the various pathophysiological processes underlying NEC endotypes, and how artificial intelligence holds the promise to influence further understanding and management (Cuna et al.). An approach to enhance surgical decision making in NEC is illustrated by Wu et al. Based on x-rays from 263 neonates diagnosed with NEC (94 surgical cases), a binary diagnostic tool was trained and validated, with Resnet18 as approach applied (Wu et al.). For PDA, an ultrasound-based assessment of ductus arteriosus intimal thickness in the first 24 h after birth was applied in 105 preterm neonates. A prediction model for closure on day 7 included birth weight, mechanical ventilation, left ventricular end-diastolic diameter, and PDA intimal thickness (Hu et al.). Such models can be considered to better target future study, integrated in a precision medicine approach. Use of AI and big data have the potential to significantly improve our understanding of neonatal conditions and also support neonatal researchers in asking better research questions.
Underreported aspects of contemporary NICU care, holistic care
As part of this research topic, we also accepted papers reporting on the use of music on pain management, on multisensory stimulation to improve maternal milk volume production, and parents’ experiences related to congenital cardiac surgery. All these 3 papers reflect the need for holistic care and to further integrate the perspectives of (former) patients and parents into neonatal practice.
In a systematic review, Ou et al. demonstrated that music is an effective intervention to relief procedural pain (e.g., Premature Infant Pain Profile score) in preterm neonates, as it reduced some markers of stress, and improved blood oxygen saturation (Ou et al.). Multisensory stimulation (audiovisual, or audiovisual + olfactory) compared to a control setting improved maternal milk volume production, with evidence of positive effects of both interventions, even more pronounced if both interventions are combined (Cuya et al.). Finally, a quantitative analysis of parent’s experiences with neonates admitted to NICU with a congenital heart disease reinformed us on the importance of actively focusing on parental experiences of care (Catapano et al.).
From advances in neonatal care to implementation In our opinion, this research topic nicely illustrates the diversity in ongoing clinical research activities, that all hold the promise to improve our clinical management practices, with the overarching aim to improve neonatal outcomes. There is an urgent need to focus on the current health inequities in the provision of care to neonates (3). The trend towards a “neuro” dedicated NICU care is an illustration on how relevant progress may occur. This progress is based on improved neuromonitoring techniques (7), improved management and precision medicine in the field of anti-epileptic drugs (8), and integrating families as partners in neonatal neuro-critical care and similar improvement programs (9). The good news is that we are already experiencing a shift in the right direction. The neonatal community and all other relevant stakeholders need to work better together to improve the pace and scale of this improvement.
Source:https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2025.1552262/full
Despite the widespread use of pain rating scales in neonatal care worldwide, a new Cochrane review shows that current tools for assessing pain in newborns are based on very low quality evidence. According to the review, none of the pain rating scales in use today are methodologically reliable enough to measure pain.
The Cochrane analysis, which included 79 studies involving over 7,000 infants across 26 countries, evaluated 27 different clinical rating scales. The findings reveal significant limitations in the reliability and clinical usefulness of all currently available tools, raising concerns about whether healthcare professionals can accurately measure pain in this extremely vulnerable population.
“We were truly hoping that one pain scale would be stronger than another, but instead we found that all of them are poorly developed. This is an issue that also affects Swedish clinical practice and research. For example, a recent publication out of KI found that 25 percent of Swedish infants were assessed without using a rating scale at all, which was already shocking, and now we can confirm that the remaining 75 percent of the infants were assessed with rating scales that are now known to not be methodologically sound enough to measure pain. So, this unfortunately means that medical professionals cannot be sure whether they are measuring pain at all.” says Emma Persad, Phd student at the Department of Women’s and Children’s Health, Karolinska Institutet.
Yet, from this uncertainty comes a call to action. The researchers hope these findings will spark a global collaborative effort, led by Swedish experts, to develop a new, robust, and evidence-based pain assessment scale for newborns. Such a tool could greatly improve neonatal care worldwide and further establish Sweden as a leader in the field of neonatology.
According to the article “this involves developing better rating scales or physiological techniques to measure pain”.
““This is precisely what we are hoping to do. Through convening the global community we hope these findings and the outcome become a global collaborative effort, driven by Swedish researchers, to finally develop a pain rating scale that is robust and evidence-informed (and will hopefully be properly adapted and translated for use worldwide). We hope that Sweden’s role in neonatology can further be solidified through this work,” says Emma Persad.
Source: https://news.ki.se/swedish-led-initiative-aims-to-revolutionise-pain-assessment-in-newborns

Dr. Michael Copass, M.D.—a Harborview Emergency Medicine physician instrumental in the early development and later leadership of the Medic One paramedic training program, helping expand it beyond cardiac care—worked alongside Dr. Leonard Cobb and Seattle Fire Chief Gordon Vickery to shape what would become one of the world’s most respected emergency medical systems. When the original grant funding for the Medic One program ended unexpectedly, the community rallied in extraordinary ways: bake sales, marathons, neighborhood drives, even children donating their birthday money. Their efforts raised nearly $200,000, inspiring the creation of the Medic One Foundation in 1974 to ensure this lifesaving work would never fade. Since that time, more than $35 million has been invested in Medica One’s training, equipment, and research, contributing to lifesaving outcomes on a daily basis.
Years later, that legacy still lives and breathes inside the halls of Harborview Medical Center. As a student assistant with the University of Washington School of Medicine and the UW surgical residency program, I had the privilege of witnessing something quite extraordinary. Each week, an Emeritus physician would return to the hospital—not for recognition or ceremony, but simply to sit down for lunch and vibrant conversation.
Those gatherings were never formal lectures. They were living, breathing exchanges of wisdom — stories from the early days of emergency medicine, thoughtful clinical reflections, and gentle reminders that compassion matters just as much as technical skill. Students, interns, residents, fellows, and senior attendings all pulled up chairs. Hierarchies faded. Curiosity filled the room. Medicine, in its truest form, felt like a shared calling.
It was in those moments that I truly understood the impact Emeritus physicians have on the medical community. They often carry history, perspective, humility — and they give it away freely. Their mentorship strengthens not just clinical practice, but the heart of healthcare itself. The legacy of Medic One isn’t only found in ambulances and survival rates — it is also found in conversations around cafeteria tables, where knowledge is passed from one generation to the next.
And as we continue to advocate for fragile newborns and medically complex children, that lesson stays with me: when compassion, community, courage, and teaching come together, the ripple effect is immeasurable — and hope continues forward.
–Kathryn Campos & Kathy Papac