

Slovakia, officially the Slovak Republic, is a landlocked country in Central Europe. It is bordered by Poland to the north, Ukraine to the east, Hungary to the south, Austria to the west, and the Czech Republic to the northwest. Slovakia’s mostly mountainous territory spans about 49,000 km (19,000 sq mi), hosting a population exceeding 5.4 million. The capital and largest city is Bratislava, while the second largest city is Košice.
Slovakia is a developed country with an advanced high-income economy. The country maintains a combination of a market economy with a comprehensive social security system, providing citizens with universal health care, free education, one of the lowest retirement age in Europe and one of the longest paid parental leaves in the OECD. Slovakia is a member of the European Union, the Eurozone, the Schengen Area, the United Nations, NATO, CERN, the OECD, the WTO, the Council of Europe, the Visegrád Group, and the OSCE. Slovakia is also home to eight UNESCO World Heritage Sites. The world’s largest per-capita car producer, Slovakia manufactured a total of 1.1 million cars in 2019, representing 43% of its total industrial output.
Healthcare in Slovakia has features of the Bismarck, the Beveridge and the National health insurance systems. It has public health system paid largely from taxation. The cost of national health insurance is shared between the employees and the employers. The part of these taxes are paid by the employees as a deduction from theirs wages and the remaining part of these taxes is paid as compulsory contribution by employers. Sole traders pay the full amount of these taxes.
These taxes are managed by health insurance companies. Current healthcare system has 3 health insurance companies, namely Union (12,4%), Dôvera (32,4%) and Všeobecná zdravotná poisťovňa (55,2%)(market share). Všeobecná zdravotná poisťovňa is a state-run insurance company, the other two are private. These insurance companies have contracts with outpatient clinics, hospitals, rehabilitation centres, pharmacies, etc. Despite this, not everywhere and not always the insurance company covers the costs. The costs are not covered for all medicines, or the full price of them. Also, it is not covered dental treatment.
The government pays health insurance for children, students, pensioners, invalids, people performing activities for a church, religious or charitable community, etc.
Source: https://en.wikipedia.org/wiki/Slovaki
- GLOBAL PRETERM BIRTH RATES – Slovakia
- Estimated # of preterm births: 6.2 per 100 live births/Global Average:
- Source- WHO Preterm Birth Rate (Per 100 Live Births)
- WHO Prematurity
- World Population Review
- WHO Country Consultation of Low and Preterm Birth Weight

COMMUNITY

CR’s experts say it’s much safer for children to wear their winter coat backward and on top of their car seat harness.
“You better bundle that baby up or she’s going to catch a cold!” I knew before I turned around what was happening: The well-meaning lady in the grocery store parking lot wanted to know why my child didn’t have a coat on in her car seat, even though it was the middle of winter.
The reason? Because a bulky coat and a child car seat can be a dangerous combination. As a general rule, winter coats should not be worn underneath a car seat harness because that can leave the harness too loose to be effective in a crash.

Research priorities for preterm lung health research across the lifespan: a community priority setting partnership

Author affiliations – Naomi R Hemy1 Amber Bates1 Belinda Frank2 Anne McKenzie2 Shannon J Simpson1 3
Abstract
Background It is essential to embed patient and public perspectives into every stage of the research journey, including setting the future research agenda. The substantial gaps in our understanding of prematurity-associated lung disease presented a timely opportunity to determine the community’s research priorities.
Objective To conduct a priority setting partnership (PSP) to determine the top 10 research priorities for preterm lung health.
Design We undertook a modified James Lind Alliance methodology comprising three main stages: (1) an idea generating survey with open questions to ascertain the community’s most important ideas for future preterm lung health research, (2) prioritisation survey to distill the main themes into a shortlist of 20 and (3) consensus workshop where participants were tasked with ranking their final top 10. This PSP is reflective of the view of preterm-born individuals, parents of preterm children and healthcare professionals in an Australian healthcare setting.
Results We collated 144 submissions from the idea generating survey from which 27 prioritisation themes were developed. From the 150 prioritisation survey responses, the 20 themes receiving the most votes were taken to the consensus workshop. Participants identified the following top 10: (1) lifelong impacts; (2) interventions, treatments or supports; (3) ongoing lung health follow-up; (4) diagnostic tools, resources and education for primary healthcare providers; (5) resources to inform and empower families; (6) relationship to physical health and developmental issues; (7) preventing and/or treating lung infections; (8) additional supports, resources and research for minority groups; (9) impact on mental well-being; and (10) likelihood of asthma diagnosis.
Conclusion Priorities identified through the PSP will be invaluable in informing future research into prematurity-associated lung disease.
Full Study-https://bmjpaedsopen.bmj.com/content/9/1/e003050


Neurodevelopmental Impairment, who decides what it is?
Posted on 27 January 2025 by Keith Barrington
Following important research in neonatology / newborn medicine from around the world
I have written frequently about my concerns with “NDI” as an important measure of neonatal outcomes, indeed, it seems to be often thought of as if it were the only important measure. It has very often been included as part of a composite outcome measure “death or NDI”.
So why am I disturbed about the use of NDI as a primary outcome measure? NDI is itself already a composite measurement, including some indicator of delayed development (most commonly one of the various iterations of the Bayley Scales of Infant Development), some severity of motor disorder expected to be permanent, i.e. Cerebral Palsy, some severity of hearing loss, and some severity of visual impairment. It was a composite invented by neonatologists and follow up specialists as a way of trying to quantify the impacts of adverse cerebral impacts of prematurity. There are many problems with this, both in the actual importance of each component of NDI, and also in the permanence of the finding. For example, most infants with low scores on developmental screening tests at 2 years do not have intellectual impairment at follow up. In the follow up of the CAP trial, for example, only 18% of babies who had a low Bayley score at 18 months (version 2 MDI <70) actually had a low IQ at 5 years (WPSII <70). This is unlike CP, for which a diagnosis at 2 years is very accurate (not 100%, but appears to be about 95% PPV) as a predictor of long term motor dysfunction, but the severity of the problem can vary, especially after a diagnosis at 2 to 3 years, where about 1/3 of infants will change their classification on the GMFCS, either to a higher or a lower score. Visual and auditory impairments seem to be more permanent and invariable, but are a much smaller part of the NDI.
And, of course, combining NDI with death as part of a composite outcome implies that they are equally important, and means that an intervention which decreases death may not be found to be significant is there is an increase in low BSID scores in the survivors (for example).
Do parents of babies who are labelled as having NDI think that their infants are impaired? That is the question asked in a new publication from the follow up centres across Canada (Canadian Neonatal Follow-Up Network, CNFUN). Richter LL, et al. Parental and Medical Classification of Neurodevelopment in Children Born Preterm. Pediatrics. 2025. Over 1000 very preterm infants are involved in the study, and their parents were asked if they thought that their child had a developmental impairment when they attended a follow-up clinic appointment, but before they completed the standardised evaluation. They then had their evaluation and were classified as having no NDI or :
“to have a mild-moderate NDI if they had any 1 or more of the following: CP with GMFCS 1 or 2; Bayley-III motor, cognitive, or language composite scores 70 to 84; hearing loss without requirement for hearing devices or unilateral visual impairment. A child was considered to have a severe NDI if they had any 1 or more of the following: CP with GMFCS 3, 4, or 5; Bayley-III motor, cognitive or language composite scores <70; hearing aid or cochlear implant; or bilateral visual impairment.”
As this table shows, there was poor agreement between what the parents thought, and what the standardised evaluation stated. Most of the disagreements were parents considering their infants to not be impaired, or to be less impaired than the standard classification. There were 185 infants with “severe NDI” according to the definition above, only 23 parents thought their child was severely impaired, in contrast, among the 596 with no NDI, there were 11 parents who found their child to have severe impairment, and 104 thought they had mild-moderate impairment.
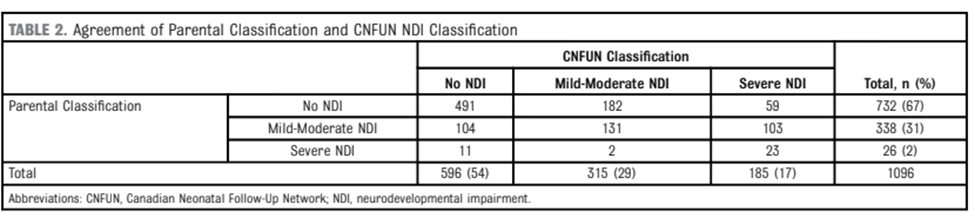
Some of the details of the analyses are quite interesting, for example, the small number of infants with serious CP, GMFCS 4 or 5, were mostly considered to have moderate or severe impairment by parents. The cognitive scores of infants who agreed that their infant, with CNFUN defined severe NDI, had at least moderate impairment were lower (median 70) than those who disagreed (median 80).
Many problems faced by families with ex-preterm infants are not captured by “NDI”. This is reflected, I think, by those parents who thought their child was impaired despite not satisfying CNFUN definitions, such infants were much more likely to be using technology at home, and more likely to have been referred for occupational therapy, or to see a psychologist or other therapist. Needing re-hospitalisation also made parent more likely to agree that their infant had an impairment.
Because we haven’t measured some of the things that impact families, such as behavioural disturbances, feeding problems, and sleep disruption, we really don’t know if they are affected by any of our NICU interventions. It wouldn’t surprise me if some interventions, ranging from postnatal steroids to skin-to-skin care or light cycling, might have major impacts on those outcomes. We just don’t know.
What should we do about findings such as these newly published data, and others from the Parents’ Voices project? Defining a single ‘yes or no’ outcome variable is the old-fashioned way of designing research and determining the benefit of an intervention. There are much better ways of comparing outcomes between groups, ways which can take into account the variety of outcomes, and the preferences of parents. It takes some extra work to define the kind of ordinal outcomes which reflect the values of parents and the relative importance of each component, but that is hugely preferable to using composite outcomes which implicitly value each component as being equivalent. Being dead, having a Bayley Cognitive composite of 69, having severe visual loss all qualify as “dead or severe NDI”, but the implications are enormously different.
In the future outcomes we measure should focus on how infants function, and should recognize that the answer to the question “how is your child doing?” is not a dichotomous choice.
High protein intake on later outcomes in preterm children: a systematic review and meta-analysis
Subhasish Das, Thomas McClintock, Barbara E. Cormack, Frank H. Bloomfield,Jane E. Harding & Luling Lin Pediatric Research volume 97, pages67–80 (2025)
Abstract
Background
Appropriate protein intake is crucial for growth and development in children born preterm. We assessed the effects of high (HP) versus low protein (LP) intake on neurodevelopment, growth, and biochemical anomalies in these children.
Methods
Randomised and quasi-randomised trials providing protein to children born preterm (<37 completed weeks of gestation) were searched following PRISMA guideline in three databases and four registers (PROSPERO registration CRD42022325659). Random-effects model was used for assessing the effects of HP (≥3.5 g/kg/d) vs. LP (<3.5 g/kg/d).
Results
Data from forty-four studies (n = 5338) showed HP might slightly reduce the chance of survival without neurodisability at ≥12 months (four studies, 1109 children, relative risk [RR] 0.95 [95% CI 0.90, 1.01]; P = 0.13; low certainty evidence) and might increase risk of cognitive impairment at toddler age (two studies; 436 children; RR 1.36 [0.89, 2.09]; P = 0.16; low certainty evidence). At discharge or 36 weeks, HP intake might result in higher weight and greater head circumference z-scores. HP intake probably increased the risk of hypophosphatemia, hypercalcemia, refeeding syndrome and high blood urea, but reduced risk of hyperglycaemia.
Conclusions
HP intake for children born preterm may be harmful for neonatal metabolism and later neurodisability and has few short-term benefits for growth.
Impact statement
- Planned high protein intake after birth for infants born preterm might be harmful for survival, neurodisability and metabolism during infancy and did not improve growth after the neonatal period.
- Protein intake ≥3.5 g/kg/d should not be recommended for children born preterm.
Conclusion (Full Study)
Planned high protein intake in the first weeks after preterm birth had few benefits and may be harmful for survival, neurodisability and biochemical abnormalities in neonatal care. However, there are few data beyond the toddler period and considerable unexplained heterogeneity. Longer-term follow-up and an individual participant data meta-analysis of existing trials, including data on total energy intake, would be helpful to clarify the effects of high protein intake for children born preterm.
FULL Article:https://www.nature.com/articles/s41390-024-03296-z

HEALTHCARE PARTNERS

Personalized communication with parents of children born at less than 25 weeks: Moving from doctor-driven to parent-personalized discussions
Marlyse F. Haward a, Antoine Payot b c, Chris Feudtner d e, Annie Janvier b c

Abstract
Communication with parents is an essential component of neonatal care. For extremely preterm infants born at less than 25 weeks, this process is complicated by the substantial risk of mortality or major morbidity. For some babies with specific prognostic factors, the majority die. Although many of these deaths occur after admission to the intensive care unit, position statements have focused on communication during the prenatal consultation. This review takes a more comprehensive approach and covers personalized and parent-centered communication in the clinical setting during three distinct yet inter-related phases: the antenatal consultation, the neonatal intensive care hospitalization, and the dying process (when this happens). We advocate that a ‘one-size-fits-all’ communication model focused on standardizing information does not lead to partnerships. It is possible to standardize personalized approaches that recognize and adapt to parental heterogeneity. This can help clinicians and parents build effective partnerships of trust and affective support to engage in personalized decision-making. These practices begin with self-reflection on the part of the clinician and continue with practical frameworks and stepwise approaches supporting personalization and parent-centered communication.
Section snippets
Part 1: Antenatal consultation
Current recommendations for the antenatal consultation focus on equalizing knowledge imbalances by providing parents with physician-derived sets of information to facilitate rational, data-driven choices.14 These information sets span short and long-term morbidities, survival and mortality statistics determined by physicians, with little input from parents. Although recommendationssuggest exploring values, they fall short in acknowledging the ‘process’ of relationship building.
Part 2. Communication during the neonatal hospitalization
Parent-centered communications during neonatal hospitalizations follows similar concepts. This section will add how continuity of care and ‘good parenting beliefs’ can help manage uncertainty, hope, and realism. We will consider the case of Ms. Gladwell.
Part 3. Dealing with death: the importance of a stepwise approach
Generally, for babies born at less than 25 weeks, neonatal death occurs relatively early when the infant does not respond to interventions, often within the first 3 days of life for the most immature babies.84 Other babies die when respiratory support is removed after death is judged inevatable, or for quality of life concerns.15 For parents like Ms. Gladwell, when death is not immediate, time permits knowledge to be acquired and values to be clarified influencing how choices are interpreted.
Conclusion
Parents and families will live with these experiences for the rest of their lives. How they remember the communication process and care their infants received depends on their perceptions of the relationships built with clinicians and their ability to ‘justify’ what happened within the context of their values. Behaviors that make them feel disrespected or their infant not valued can leave lasting impressions, whereas trusting partnerships solidifies their roles as parents.
Source:https://www.sciencedirect.com/science/article/abs/pii/S0146000521001658?via%3Dihub
Having Kids During Residency (Part 1) – Journey Through Medicine
Efficiently Natural Jan 24, 2021 #medicalschool #residency #doctorcouple
Here’s another video in our Journey Through Medicine series where we talk about what it was like for us to have a child while both completing our medical residencies. There’s never a perfect time to have a child during medical training, but here’s how we made it work. #medicalschool #residency #doctorcouple

Neuroprotective therapies in the NICU in preterm infants: present and future
Nature–Neonatal Neurocritical Care Series – 19 December 2023
Abstract
The survival of preterm infants has steadily improved thanks to advances in perinatal and neonatal intensive clinical care. The focus is now on finding ways to improve morbidities, especially neurological outcomes. Although antenatal steroids and magnesium for preterm infants have become routine therapies, studies have mainly demonstrated short-term benefits for antenatal steroid therapy but limited evidence for impact on long-term neurodevelopmental outcomes. Further advances in neuroprotective and neurorestorative therapies, improved neuromonitoring modalities to optimize recruitment in trials, and improved biomarkers to assess the response to treatment are essential. Among the most promising agents, multipotential stem cells, immunomodulation, and anti-inflammatory therapies can improve neural outcomes in preclinical studies and are the subject of considerable ongoing research. In the meantime, bundles of care protecting and nurturing the brain in the neonatal intensive care unit and beyond should be widely implemented in an effort to limit injury and promote neuroplasticity.
Impact
- With improved survival of preterm infants due to improved antenatal and neonatal care, our focus must now be to improve long-term neurological and neurodevelopmental outcomes.
- This review details the multifactorial pathogenesis of preterm brain injury and neuroprotective strategies in use at present, including antenatal care, seizure management and non-pharmacological NICU care.
- We discuss treatment strategies that are being evaluated as potential interventions to improve the neurodevelopmental outcomes of infants born prematurely.

https://www.nature.com/articles/s41390-023-02895-6
Compassionate Inquiry with Gabor Maté

Leading Edge Seminars May 23, 2017
Compassionate Inquiry is a psychotherapeutic method developed by Dr. Gabor Maté that reveals what lies beneath the appearance we present to the world. Using Compassionate Inquiry, the therapist unveils the level of consciousness, mental climate, hidden assumptions, implicit memories and body states that form the real message that words both express and conceal.


PREEMIE FAMILY PARTNERS


Your friend or family has finally brought their preemie baby home from the NICU, and you’re excited to meet their little miracle, but unsure of how to approach the family altogether.
Don’t worry, as long as you stick to these simple do’s and don’ts written by a preemie mom, visiting a premature baby will be a happy and smooth time for everyone!
Do Listen to the Preemie Parents’ Conditions (and Comply)
Before visiting a premature baby, ask the parents if they are ready to receive visits in their home. And under which terms.
Don’t miss out!
You know the drill, if you want to be part of Preemie Mom Tip’s email list, subscribe below! You’ll receive weekly emails that will help you on your journey. We are preparing a new and improved FREE resource library, sign up and be the first to know once it’s ready!
Top of Form
It’s not uncommon that when we take our babies home, the doctors impose a no visit rule until we can complete the first vaccination schemes (which more often than not include at least three shots of the Synagis shot.) The complete process can take up to three months.
We didn’t allow almost any visit from friends or family until my son was around four months old (2 months old adjusted), some of our friends were understanding, and some weren’t.
We knew that we were doing what was best for our son, so we stuck to it!
If your friend says it’s OK to visit their baby, find out if they have any special request for your visit.
Some of the petitions may seem weird but know that they come from a very real place (the NICU), and visiting a premature baby during her first months is much like visiting babies in the NICU: short and strict.
Some parents may ask you to keep your cell phones at the entrance of the house (phones are full of germs), wash your hands for five minutes, visit straight from home, or tie your hair, take a shower just before visiting, or wear a surgical face mask. Whatever it is, by doing as they say you’ll help protect their baby and their peace of mind.
Do Bring Extra Clean Clothes for Interacting with the Preemie Baby
This is especially true if you are visiting a premature baby after being all day outside of your home.
The street is full of germs and contamination, and we preemie parents tend to develop a germ-vision.
By bringing freshly laundered clothes and changing into them as soon as you arrive at the house you are visiting you will show them that you are on their side, and support their every measure to keep their baby safe.
It is even more likely that they will let you hold the baby if you do this since she won’t be directly exposed to dirty clothes.
Do: Wash your Hands as Soon as you Enter, Wash your hands thoroughly.
Make sure you wash the space between your fingers, your palm, and the back of your hand.
You’ll be amazed to know the number of diseases we can avoid by just washing hands. Simple, right?
Even so, many of us neglect this standard practice.
When a baby is in the NICU, the nurses teach us parents about the importance of hand-washing, the correct techniques to do so, the right moment to do it. We wash our hands so frequently that we get rashes most of the time (since the NICU soap is strong.)
It is second nature to us to wash our hands when visiting babies!
Having said all this, once our babies are bigger and stronger, we’ll be a bit laxer about this. After all, germs do help develop the immune system, we just don’t want to expose our miracles before they are ready for this!
Do Keep the Visit Short and Simple
There will be time for the lengthy visits that you may be dreaming about. In the months and years to come, you’ll be able to kiss and smooch the baby to your heart’s content, and stay during weekends, afternoons, and evenings!
But right now, the preemie family may be in need of some alone time. And though seeing you will surely help them, keep your visit under 30 minutes if possible.
Most breastfeeding moms need time adjusting to… well…breastfeeding, but this is especially the case of us preemie moms. We came from pumping our way in the NICU to actually breastfeeding a baby. That transition takes time to get used to.
Additionally, like all new parents, we are most likely to be sleep-deprived. Partly because our babies wake us up all night and partly because of the monitors beeping or ourselves waking up to check that the babies are doing fine.
Keeping a short visit is a long time investment in your relationship with NICU families.
Don’t Go if You’re Not Feeling Well
If your head hurts, your throat is sore or your nose itches, reprogram your visit.
Even if you are feeling well but visited someone who has had the flu within seven days before your visit you may be carrying the virus, so it’s also best to reprogram.
RSV and pulmonary infections are dangerous for preemies.
Ollie had simple flu when he was 12 months old and turned into pneumonia and bronchiolitis in less than 24 hours. We had to rush him to the ER because he wasn’t breathing. He was in the hospital on oxygen for ten days until he recovered. The younger the baby, the higher the risk of infection.
We limited our visits to non-flu visitors until Ollie was well over 8 months. And, we still ask everyone who may be sick to wear a facemask. We don’t overprotect our son, he goes to crowded places and has had the flu several times by now at 24 months. But we still don’t want to risk it by letting someone with the flu hold him without wearing a facemask.
Don’t Hold the Preemie Baby
Unless the parents ask you to hold their baby, don’t press them into it.
You’ll have plenty of opportunities. Just make them feel comfortable by knowing that you are OK just looking at the baby. If they are comfortable with you holding her, they will let you know.
Also, to keep on the safe side, avoid kissing the baby and holding her hands.
Don’t Compare their Preemie to any Other Baby
As preemie parents, the greatest joy in the world comes with sorrow.
We love our baby and wouldn’t change him for anyone else, nor would we want him to be any different. So we try not to compare our baby to anyone else’s. But, sometimes it is inevitable, and we internally cave in.
My son looked like a newborn during his first four months. He didn’t smile until he was eight months old and had to go through weekly Physical Therapy to move his hands and arms. He is healthy, bright, and has no significant delay. But when the children of my friends were smiling, walking, and talking, he wasn’t, and it’s human nature to worry and to compare them.
It gets even worse when people pity my boy or openly compare him to others. It feels as if they are undermining us as if they don’t know or don’t care about our background.
A few months ago a fellow mom who has a son two months younger than Ollie (but bigger and heavier), raved on and on about how small and fragile my Ollie was. She held him without my permission and said that she remembered the times when her son was smaller. She went as far as to congratulate me for being so chill and not overprotecting him. He was evidently so weak (to her eyes.) She seemed to be following an anti-manual for visiting a premature baby.
Needless to say, I despised every second we spent together, and I’ve never seen her again.
Don’t Talk about other Full-Time Pregnancies
Us moms also grieve about the weeks that we should have been heavily pregnant and weren’t.
Sometimes I see other moms complaining about their heavy wombs. Begging for their babies to come early so that they can stop being feeling uncomfortable. I understand that they don’t know what they are saying, but it hurts.
My son was born at 31 weeks, which means that I missed out on nine weeks of pregnancy. Some women dream about their pregnancies their whole lives. They imagine them picture perfect, so we miss what we didn’t have. And in some cases, what we’ll never have.
So it’s better to play it safe and stay clear of that topic.
That’s a Wrap
I’m sure you’ll love visiting a premature baby. Take it one step at a time and be patient with us preemie parents. We do want what’s best for our children, even if sometimes it is hard to express ourselves.
Most of all, you’ll see how powerful and miraculous a person can be, no matter how small!
Have you visited a preemie recently? Are you planning a preemie visit? Or, are you a preemie parent and would like people to know how to plan their visits? Tell us all about it in the comment section!
Source: https://preemiemomtips.com/visiting-preemie-dos-donts/

A 25-year study reveals how empathy is passed from parents to teens to their future children
By Jessica A. Stern, University of Virginia and Joseph P. Allen, University of Virginia
Posted on January 14, 2025
Empathy — the capacity to identify others’ needs and emotions, and to provide supportive care that meets those needs.
Our recent research shows that parents who express empathy toward their teenagers may give teens a head start in developing the skill themselves. In addition, adolescents who show empathy and support toward their friends are more likely to become supportive parents, which may foster empathy in their own offspring.
How we did our work
The KLIFF/VIDA study at the University of Virginia has tracked 184 adolescents for more than 25 years: from age 13 well into their 30s.
Starting in 1998, teens came to the university every year with their parents and closest friend, and a team of researchers recorded videos of their conversations. Researchers observed how much empathy the mother showed to her 13-year-old when her teen needed help with a problem. We measured empathy by rating how present and engaged mothers were in the conversation, whether they had an accurate understanding of their teen’s problem, and how much help and emotional support they offered.
Then, each year until teens were 19 years old, we observed whether teens showed those same types of empathic behaviors toward their close friends.
A decade later, when some of those same teens were starting to have children of their own, we surveyed them about their own parenting. We also asked them about their young children’s empathy. For example, parents rated how often their child “tries to understand how others feel” and “tries to comfort others.”
We found that the more empathic a mother was toward her teenager at age 13, the more empathic the teen was toward their close friends across the adolescent years. Among teens who later had kids themselves, the ones who had shown more empathy for close friends as adolescents became more supportive parents as adults. In turn, these parents’ supportive responses to their children’s distress were associated with reports of their young children’s empathy.
Why it matters
The ability to empathize with other people in adolescence is a critical skill for maintaining good relationships, resolving conflict, preventing violent crime and having good communication skills and more satisfying relationships as an adult.
Adults want teens to develop good social skills and moral character, but simply telling them to be kind doesn’t always work.
Our findings suggest that if parents hope to raise empathic teens, it may be helpful to give them firsthand experiences of being understood and supported.
But teens also need opportunities to practice and refine these skills with their peers. Adolescent friendships may be an essential “training ground” for teens to learn social skills such as empathy, how to respond effectively to other people’s suffering, and supportive caregiving abilities that they can put to use as parents. Our lab’s most recent paper presents some of the first evidence that having supportive teenage friendships matters for future parenting.
What’s next
We’re continuing to follow these participants to understand how their experiences with parents and peers during adolescence might play a role in how the next generation develops.
We’re also curious to understand what factors might interrupt intergenerational cycles of low empathy, aggression and harsh parenting. For example, it’s possible that having supportive friends could compensate for a lack of empathy experienced from one’s family.
While it’s true that you can’t choose your family, you can choose your friends. Empowering teens to choose friendships characterized by mutual understanding and support could have long-term ripple effects for the next generation.

*We checked to confirm these organizations are still active in February, 2025.There was only one resource we were unable to locate. We have also attached the website links!
12 Preemie Support Groups For New Parents, Because You Can’t Go It Alone
It really does take a village for preemie parents by Kinsey Gidick Nov.24, 2020
Only the parents of a premature baby can understand the emotional toll it takes to care for such a fragile child. That’s why finding a community of parents and caretakers who have been through similar circumstances is so important. Fortunately, there are many online resources for parents experiencing the challenge of navigating the NICU and raising a premature baby, from preemie support groups to virtual counseling sessions to even social media accounts.
While each is different, the focus is the same: to provide a space where preemie parents can bring their worries, wins, and concerns to each other and get help and feedback from those going through the same situations. 380,000 babies are born before 37 weeks gestation each year in the U.S. per March of Dimes — that’s 1 out of every 10 American babies. That’s a lot of babies receiving extensive medical intervention including respiratory support, invasive treatments, and extended Neonatal Intensive Care Unit stays. In many cases, these spaces are like lifelines for parents who are afraid of not only the unknown, but the known as well.
Rather than shoulder that burden alone, preemie support groups offer all kinds of resources from chat rooms to virtual mentors, podcasts to classes. It’s the kind of care one won’t often find in a clinic or hospital — ongoing assistance a preemie parent can turn to whether a child is 3 weeks or 3 years old.
1. A space for NICU transition support
Graham’s Foundation, a not-for-profit support group based in Ohio, was founded with a mission that no one should experience prematurity alone. To that end, the organization has a number of programs designed to help pre-term birth families including NICU transition to home care packages, preemie parent mentors who can be contacted 24/7, an app called MyPreemie, and many online forums for parents to engage with other preemie families. –https://www.grahamsfoundation.org/
2.A community of peers
Hand to Hold is an organization created to guide preemie families through the long journey from a NICU stay to home, as well as provide comfort and support in times of loss. To do so, the website maintains forums for its 63,000 online community members. But it’s not just for preemie families. There are also resources for NICU professionals including podcasts and an ambassador program of bedside support volunteers who visit NICUs and provide additional help. –https://handtohold.org/
3.A place for bereavement support
Bereavement support is something all too many families of premature babies need. And High Risk Hope is one place they can find it. The 501(c)3 believes that “there is no foot too small that it cannot leave an imprint on this world.” To do so, the Florida-based organization connects families with other organizations to provide ongoing grief support and counseling. –https://highriskhope.org/
4.One-on-one care
Support 4 NICU Parents Support 4 NICU Parents aims to improve psychosocial support for NICU parents and enhance training and support for NICU healthcare providers, ensuring families and babies thrive together. –https://www.pqcnc.org/node/13721
5.Parental Zoom chats
Tiny Miracles is a nonprofit charity based in Fairfield County, Connecticut, that is dedicated to helping families with premature babies. Like many premature baby groups, it offers all kinds of resources for families, but its most popular offerings are free weekly Zoom support chats that anyone can join. Held every Thursday at 8 p.m. EST, they’re a way for people to get to know other parents beyond a virtual chat room or forum.-https://www.projectsweetpeas.com/
6. Material support
Care packages, hospital events, peer-to-peer support, financial aid, educational materials, these are all the work of Project Sweet Peas. Families can reach out directly for all of the above and receive the care they need from this nonprofit. And for those who have simply been touched by a premature birth and want to give back, they can donate to Project Sweet Peas’ effort which has sent 23,126 NICU care packages to families and 4,909 bereavement boxes as well.-https://www.projectsweetpeas.com/
7.Facebook Preemie Page
Social media sites, like Facebook, are a natural home for support groups and the Parents of Preemies/Premature Babies is one of the biggest for this specific demographic. With 15.3K members, it’s a private group you must ask to join. It was started in 2007 when founder Heather Armstrong writes that she couldn’t find a similar support space. It invites members to discuss topics related to the raising of premature children but doesn’t allow fundraising, self-promotion, or requests for medical advice. It includes parents of preemies from around the world.-https://www.facebook.com/groups/2304668997
8. Helping hand from March of Dimes
Not every hospital has a March of Dimes NICU Family Support program, but it’s worth inquiring should a family find itself with a baby in the newborn intensive care unit. The nonprofit that’s committed to improving the health of mothers and babies organized its NICU Family Support program to provide families with essential materials during their child’s NICU stay. Those include things like “keepsake booklets for their NICU baby, a guide for parenting in the NICU, and a NICU guide” according to the organization’s website. For families with an infant having a shorter NICU stay, March of Dimes provides materials as well. There’s also a helpful app where families can explore their questions and concerns.-https://www.marchofdimes.org/find-support/compassbymarchofdimes
9.Support for babies less than 2 pounds
Premature babies are not a monolith. There are varying levels of prematurity and some of the most at-risk children are those born less than 2 pounds and before 27 weeks. That’s why the Micro Preemie Parents Facebook support page exists, to be there for parents of these special children. Only parents of so called “micro preemies” will be accepted to the private page. Once in, they can expect to be able to join conversations specific to this very unique experience with other parents and guardians who understand where they’re coming from. –https://www.facebook.com/groups/micropreemiemoms
10. A Space for Black Preemie Parents
Black Preemie Parents Community is a Facebook group just for Black parents to find “support, advice, share stories, or just vent as you go through your journey.” It’s a small group with less than 400 members providing those who join with an intimate circle of friends to reach out to during challenging times. –https://www.facebook.com/groups/blackpreemieparentscommunity
11. Where to go when they grow
The premature parenting journey doesn’t end when a child leaves the NICU. It’s a lifelong path and one that might find parents looking for support well into their child’s teens and twenties. For that there’s Parents of Older Preemies. Another Facebook group, this 1.5K member page is for “parents to share their stories of their preemie(s) and how far they have come in their lives in a caring and supportive environment. This group shares triumphs, setbacks, frustrations and positive advice to others that are on their continued “preemie journey.”-https://www.facebook.com/groups/276697059074997
12. Visual Support
Preemie baby support isn’t limited to Facebook and nonprofit organizations. Instagram has also become a network where people kind find kinship in navigating life with a preemie. For instance, preemiesupermoms is an Instagram page dedicated to prematurity awareness. The page posts images of premature babies along with inspiring quotes and stories
For families looking for someone to listen or a place to gather strength, these organizations are here to help. All families need to do is ask. –https://www.instagram.com/preemiesupermoms/
INNOVATIONS
EDITORIAL: What is new on the Horizon in Neonatology? Recent Advances in Monitoring, Diagnostics, and Therapeutics in Neonatal Care

Introduction
Neonates and infants are commonly referred to as “therapeutic orphans” due to the overall scarcity of therapeutic interventions that have been developed and tailored to their needs and specific characteristics . This is well known by care providers and researchers active in this field, but is perhaps less on the radar of authorities, funding bodies or the broader public. There is significant health inequity when comparing newborns to other age populations in terms of specific drug and device development and therapeutics . In addition there are health inequities in the provision of neonatal care globally which require special attention in terms of improvement .
Bronchopulmonary dysplasia, neonatal seizures, poor growth, necrotizing enterocolitis (NEC) and short bowel, hypoxic-ischemic encephalopathy, retinopathy of prematurity (ROP), neonatal infections and sepsis hereby serve as a non-exhaustive list of “orphan conditions” in need of more equity, through adequately and urgently funded research and improvement.
The good news is that there have been increased efforts, in recent years, by researchers and regulatory bodies to focus on the provision of drugs, devices, and treatment modalities tailored for neonatal use, while further advocacy remains an obvious need (2, 4, 5). This brings perspective and explains the initiative taken to organize a focused research topic on what is on the horizon as well as recent advances.
Overview of the topics covered
We targeted emerging or new aspects related to monitoring, diagnostics and therapeutics in neonatal care for the current research topic. Fortunately, this research topic was perceived as very relevant by the research community, as 135 authors expressed their interest as contributors, resulting in 20 accepted papers. This serves as a signal of the importance to continue to work on this topic.
Post-hoc, and in a somewhat arbitrary way (because of overlap in these subcategories) these papers were subdivided by the editors into different subcategories, with focus on (1, 5 papers) perinatal biomarkers in blood and urine and how these relate to or predict outcomes, (2, 6 papers) adaptations of existing and newly emerging equipment in neonatal units, (3, 3 papers) needed advances in pharmacotherapy, (4, 3 papers) machine learning or deep learning applications in neonatal care, and finally, (5, 3 papers) underreported aspects of contemporary NICU care, with a focus on the holistic nature of care for the infant and the family.
Perinatal biomarkers in blood and urine and how these relate to or predict outcomes
Two papers focused on biomarkers related to gestational diabetes, with reflections and data on maternal and neonatal outcomes. Postnatal maternal levels of glycated albumin and hemoglobin A1c in mothers of large-for-gestational-age (LGA) informed us of the relevance of accurate diagnosis during pregnancy. This is because postpartum women without diagnosis during pregnancy had higher glycated albumin values, associated with LGA and associated complications (Železnik et al.). Interestingly and related to this paper, Yin et al. reported on a untargeted metabolomics study in women with gestational diabetes, with the recommendation of a maternal serum metabolite panel to forecast neonatal adverse outcomes (hypoglycemia and macrosomia) (Yin et al.).
Other papers focused on the use of vitamin D, acid-base and biomarkers associated with fetal growth restriction with impaired neurodevelopmental outcome. In a cohort of 217 preterm neonates, a multivariate regression analysis identified antenatal steroids as protective, and lower birth weight, duration of ventilation, sepsis and the serum 25-(OH)D vitamin as risk factors to develop ROP (Yin et al.). Musco et al. reported on a systematic review on blood biomarkers indicating risks of adverse neurodevelopmental outcome in fetal growth restricted infants (Musco et al.). While the authors retrieved some data on neuron specific enolase and S100B, the overall conclusions reflect a call for further research. Finally, an association between lactate levels in umbilical cord blood and cerebral oxygenation in preterm neonates was studied as a secondary outcome analysis (Dusleag et al.). In non-asphyxiated preterm neonates with respiratory support, lactate levels were negatively associated with cerebral and arterial oxygenation. In term neonates without respiratory support, no associations were observed.
Adaptations of existing and newly emerging equipment in our units
In a review on emerging innovations in neonatal monitoring, Krbec et al. concluded that there is an urgent, still unmet need to develop wireless, non- or minimal-contact, non-adhesive technology, capable to integrate multiple signals in a single platform, tailored to neonates (Krbec et al.). Related to this call of action, Svoboda et al. reported on their pilot experience with contactless assessment of heart rate, applying imaging photoplethysmography (Svoboda et al.). Rectal and axillary temperature monitoring on admission were compared in a cohort of preterm (n = 80, <32 weeks gestational age) by Halabi et al., reporting that rectal measurement was likely more reliable in the event of hypothermia (Halabi et al.). Ultrasound-guided measurement of anterior cerebral artery resistive index in the first week of life in 739 preterm neonates (<35 weeks) was not associated with subsequent co-morbidities on admission or during neonatal stay (asphyxia, sepsis, NEC) (Singh Gill et al.). A case series of neurally adjusted ventilatory assist to rescue pulmonary interstitial emphysema in 5 extremely low birth weight infants illustrated the potential value of this ventilatory equipment and strategy and need for further study (Chen et al.). Finally, van Rens et al. compared a conventional to a modified Seldinger technique (a dedicated micro-insertion kit) for peripherally inserted central catheter (PICC) placement, illustrating the relevance of developing “low risk, high benefit” type of medical devices, adapted to the specific needs of neonates (van Rens et al.).
Advances needed in pharmacotherapy
The currently available medicines and dosing regimens in neonatal care are limited and there is an urgent need for improvement in this domain. This was illustrated by articles on sepsis, septic shock and steroids. Inequity in provision of neonatal care across the globe ought to be a major focus of improvement. Gezahegn et al. described the outcome in neonates admitted with sepsis in Harar (Ethiopia). Low white blood cell count, desaturation, preterm birth, absence of prenatal maternal care, and chorioamnionitis were important risk factors for sepsis-related mortality (Gezahegn et al.). Addressing these prognostic factors hold the promise to act as levelers to improve outcomes. A pilot study compared noradrenaline and adrenaline as first line vasopressor for fluid-refractory sepsis shock (Garegrat et al.). Both interventions were comparable to resolve the septic shock, while the overall mortality (13/42, 30%) remained significant, highlighting the need for better diagnostic and therapeutic options. Finally, in a systematic review, outcome of postnatal systemic corticosteroids (hydrocortisone to dexamethasone) were compared as reported in randomized controlled trials (Boscarino et al.). The authors concluded that dexamethasone appeared to be somewhat more effective than hydrocortisone in improving respiratory outcomes, but with inconclusive but relevant concerns on the uncertainties on long-term neurodevelopmental outcome, again highlighting the need for better therapies for prevention and management of chronic lung disease of prematurity.
Machine learning or deep learning applications in neonatal care
Artificial intelligence is a rapidly advancing area with fast evolving clinical applications in healthcare, including in the NICU (6). It is no surprise that the current research topic also contains papers illustrating its relevance to improve our practices and outcomes. Two papers hereby focused on NEC, and a 3rd paper on prediction of significant patent ductus arteriosus (PDA). In a mini-review, Cuna et al. reports on the various pathophysiological processes underlying NEC endotypes, and how artificial intelligence holds the promise to influence further understanding and management (Cuna et al.). An approach to enhance surgical decision making in NEC is illustrated by Wu et al. Based on x-rays from 263 neonates diagnosed with NEC (94 surgical cases), a binary diagnostic tool was trained and validated, with Resnet18 as approach applied (Wu et al.). For PDA, an ultrasound-based assessment of ductus arteriosus intimal thickness in the first 24 h after birth was applied in 105 preterm neonates. A prediction model for closure on day 7 included birth weight, mechanical ventilation, left ventricular end-diastolic diameter, and PDA intimal thickness (Hu et al.). Such models can be considered to better target future study, integrated in a precision medicine approach. Use of AI and big data have the potential to significantly improve our understanding of neonatal conditions and also support neonatal researchers in asking better research questions.
Underreported aspects of contemporary NICU care, holistic care
As part of this research topic, we also accepted papers reporting on the use of music on pain management, on multisensory stimulation to improve maternal milk volume production, and parents’ experiences related to congenital cardiac surgery. All these 3 papers reflect the need for holistic care and to further integrate the perspectives of (former) patients and parents into neonatal practice.
In a systematic review, Ou et al. demonstrated that music is an effective intervention to relief procedural pain (e.g., Premature Infant Pain Profile score) in preterm neonates, as it reduced some markers of stress, and improved blood oxygen saturation (Ou et al.). Multisensory stimulation (audiovisual, or audiovisual + olfactory) compared to a control setting improved maternal milk volume production, with evidence of positive effects of both interventions, even more pronounced if both interventions are combined (Cuya et al.). Finally, a quantitative analysis of parent’s experiences with neonates admitted to NICU with a congenital heart disease reinformed us on the importance of actively focusing on parental experiences of care (Catapano et al.).
From advances in neonatal care to implementation
In our opinion, this research topic nicely illustrates the diversity in ongoing clinical research activities, that all hold the promise to improve our clinical management practices, with the overarching aim to improve neonatal outcomes. There is an urgent need to focus on the current health inequities in the provision of care to neonates (3). The trend towards a “neuro” dedicated NICU care is an illustration on how relevant progress may occur. This progress is based on improved neuromonitoring techniques (7), improved management and precision medicine in the field of anti-epileptic drugs (8), and integrating families as partners in neonatal neuro-critical care and similar improvement programs (9). The good news is that we are already experiencing a shift in the right direction. The neonatal community and all other relevant stakeholders need to work better together to improve the pace and scale of this improvement.
Source:https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2025.1552262/full

Abstract
Background
The prenatal shunt, ductus arteriosus (DA), typically closes during the cardio-pulmonary transition at birth. We evaluated maternal and neonatal factors associated with delayed closure of DA in term-born neonates.
Method
We conducted a retrospective cohort study that included full-term neonates from the prospective observational Copenhagen Baby Heart cohort study. We assessed the association between maternal and neonatal factors and delayed ductal closure.
Results
We included 19,566 neonates, of whom 48% were female. Echocardiography was performed at a median age of 12 (IQR:9-15) and eight (IQR:2-13) days for neonates with no DA and an open DA, respectively. Associations with delayed ductal closure included maternal obesity adjusted risk ratio=2 (95%CI:1-3.8), maternal hypothyroidism during pregnancy aRR=2.02 (95%CI:1.2-3.4), low Apgar 2.6 (95%CI:1.2-6), high weight aRR=1.81(95%CI:1.2-2.6), and length at birth aRR=1.7(95%CI:1.1-2.6).
Conclusion:
The identified risk factors for delayed ductal closure in term-born neonates may help increase clinical attention and improve neonatal care.

UNICEF 2025 Global Outlook: Prospects for Children in 2025 – Building Resilient Systems for Children’s Futures
17 February 2025
Prospects for Children in 2025: Building Resilient Systems for Children’s Futures is the latest edition of Global Outlook, a series of reports produced each year by United Nations Children’s Fund (UNICEF) Innocenti – Global Office of Research and Foresight, which look at the key trends affecting children and young people over the following 12 months and beyond.
In this new report, new and intensifying crises for children – including climate change, conflict and economic instability – are shown to be closely interconnected.
For instance, climate change is disrupting the water cycle, leading to widespread water scarcity, threatening food production and livelihoods across the economy. This disruption poses direct and indirect risks to children, as it impacts the availability of safe water, food, and family income.
The report also notes that debt burdens are forcing governments to cut essential public services, including those related to water, sanitation, and hygiene. These challenges are compounded by a lack of investment in long-term development.
According to UNICEF, rising geopolitical tensions and competition among nations are hindering the implementation of solutions that will protect young people’s lives and build more resilient futures for them.
The report calls for resilient national systems that prioritize children’s health, education and wellbeing, and emphasizes the importance of including children’s rights in climate action.
Download the report here.-https://www.unwater.org/news/unicef-2025-global-outlook-prospects-children-2025-building-resilient-systems-children%E2%80%99s

WHO Youth Counsil

Hey, Neonatal Warriors!
Empathy and compassion is the foundation of the powerful bond we share as a community. It’s more than just understanding the struggles of others—it’s about truly connecting with their experiences and emotions. As we continue on our journey from the neonatal unit to where we are today, empathy strengthens our resilience and fosters a sense of unity. This connection gives us the strength to support one another, celebrate our victories, and face challenges together.
In the video you’re about to watch, we’ll dive deeper into how our shared experiences and collective empathy can empower us to not only overcome adversity but also to thrive. It highlights the importance of understanding and supporting each other, offering both comfort and encouragement in meaningful ways. Through storytelling and the exchange of our journeys, we create a community that is stronger, more resilient, and ready to face whatever challenges come our way.
I wanted to share this video because it perfectly encapsulates the power of empathy and how, together, we can elevate each other. It’s a reminder that even in difficult times, we are never alone—our shared experiences and collective strength can light the way forward.
Let’s continue to harness the power of empathy as we watch and reflect on the message in this video. Together, we are unstoppable.
What Is The Difference Between Empathy, Sympathy, and Compassion

The Power of Emotional Competency
Expert Reveals the Truth About Empathy, Sympathy and Compassion | Doug Noll
This video shows you the difference between empathy, sympathy, and compassion
• Sympathy is pity-based and is selfish
• Empathy is a learned skill
• Compassion is empathy with an impulse to relieve distress

This video is for our younger friends to help them understand empathy, which means caring about how others feel and being kind to them. Mark Ruffalo and Murray Monster from Sesame Street will show us what empathy is and give fun examples of how we can be kind and helpful to others. I wanted to share this video because it’s a great way for younger kids to learn how to show empathy and support for their friends and family. Let’s watch and see how we can all use empathy to make the world a kinder place! Enjoy watching!

Sesame Street – Empathy With Mark Ruffalo
This video is perfect for helping young students understand what empathy is. Murray Monster and Mark Ruffalo talk about what empathy means and go through several examples. Use this helpful video for introducing important social skills to your K-2 students!




Quiksilver & Roxy Czech and Slovak Surfing Championship 2022

SnowboardZezula Jul 11, 2022
Mrkni na report z Quiksilver & Roxy Czech and Slovak Surfing Championship 2022
👉 https://snbz.cz/report-surfchamp-2022

