

Scotland is a country that is part of the United Kingdom. It contains nearly one-third of the United Kingdom’s land area, consisting of the northern part of the island of Great Britain and more than 790 adjacent islands, principally in the archipelagos of the Hebrides and the Northern Isles. To the south-east, Scotland has its only land border, which is 96 miles (154 km) long and shared with England; the country is surrounded by the Atlantic Ocean to the north and west, the North Sea to the north-east and east, and the Irish Sea to the south. The population in 2022 was 5,439,842 and accounts for 8% of the population of the UK. Edinburgh is the capital and Glasgow is the largest of the cities of Scotland.
NHS Scotland sometimes styled NHSScotland, is the publicly–funded healthcare system in Scotland and one of the four systems that make up the National Health Service in the United Kingdom. It operates 14 territorial NHS boards across Scotland, supported by seven special non-geographic health boards, and Public Health Scotland.
At the founding of the National Health Service in the United Kingdom, three separate institutions were created in Scotland, England and Wales and Northern Ireland.
https://en.wikipedia.org/wiki/Scotland#
- GLOBAL PRETERM BIRTH RATES – SCOTLAND
- Estimated # of preterm births: 8.0 per 100 live births
- (Global Average: 10.6)
- Source- WHO Preterm Birth Rate (Per 100 Live Births)

COMMUNITY
Nursing and midwifery
3 May 2024

Key facts
- There are an estimated 29 million nurses worldwide and 2.2 million midwives. WHO estimates a shortage of 4.5 million nurses and 0.31 million midwives by the year 2030.
- That will bring the a global shortage of health workers estimated for 2030 to 4.8 million nurses and midwives, with the greatest gaps found in countries in Africa, South-East Asia and the WHO Eastern Mediterranean Region, as well as some parts of Latin America.
- Nurses and midwives play a pivotal role in improving health and contributing to the wider economy. Investing in them is imperative to achieve efficient, effective, resilient and sustainable health systems. They not only provide essential care but also play a critical role in shaping health policies and driving primary health care. Nurses and midwives deliver care in emergency settings and safeguard the sustainability of health systems globally.
- Globally, 67% of the health and social workforce are women compared to 41% in all employment sectors. Nursing and midwifery occupations represent a significant share of the female workforce.
- More than 80% of the world’s nurses work in countries that are home to half of the world’s population. And one in every eight nurses practices in a country other than the one where they were born or trained.
- Higher levels of female nurses are positively correlated with health service coverage, and life expectancy and negatively correlated with infant mortality.
Overview
Nurses and midwives are central to Primary Health Care and are often the first and sometimes the only health professional that people see and the quality of their initial assessment, care and treatment is vital. They are also part of their local community – sharing its culture, strengths and vulnerabilities – and can shape and deliver effective interventions to meet the needs of patients, families and communities.
WHO response
WHO’s work relating to nursing and midwifery is currently directed by World Health Assembly resolution WHA74.15 (2021) which calls on WHO Member States and WHO to strengthen nursing and midwifery through the Global Strategic Directions for Nursing and Midwifery (SDNM) 2021–2025. The SDNM is an interrelated set of policy priorities that can help countries to ensure that midwives and nurses optimally contribute to achieving universal health coverage (UHC) and other population health goals .
The SDNM comprises four policy focus areas: education, jobs, leadership, and service delivery Each area has a “strategic direction” articulating a goal for the five-year period, and includes between two and four policy priorities If enacted and sustained, these policy priorities can support advancement along the four strategic directions: 1) educating enough midwives and nurses with competencies to meet population health needs; 2) creating jobs, managing migration, and recruiting and retaining midwives and nurses where they are most needed; 3) strengthening nursing and midwifery leadership throughout health and academic systems; and 4) ensuring midwives and nurses are supported, respected, protected, motivated and equipped to safely and optimally contribute in their service delivery settings.
WHO engages ministries of health, the Government Chief Nurses and Midwives (GCNMOs) and other relevant stakeholders to enable effective planning, coordination and management of nursing and midwifery programmes in countries. The Global Forum for the Government Chief Nurses and Midwives, established in 2004, is organized by WHO and meets every two years. It is a Forum for senior nursing and midwifery officials to develop and inform areas of shared interest. WHO also engages with academic institutions specialised in nursing and midwifery. Forty-seven academic centres are designated as Collaborating Centres for Nursing and Midwifery with WHO. The academic centres are affiliated to the Global Network of WHO Collaborating Centres for Nursing and Midwifery.
WHO has established a Nursing and Midwifery Global Community of Practice (NMGCoP). This is a virtual network created to provide a forum for nurses and midwives around the world to collaborate and network with each other, with WHO and with other key stakeholders (e.g WHO collaborating centres for nursing and midwifery, WHO Academy, Nursing and Midwifery Associations and Institutions.) The network will provide discussion forums, a live lecture programme, opportunities to develop and share policies, WHO documents and tools, and facilitated innovation workshops, masterclasses and webinars.
The Nursing and Midwifery Global Community of Practice is free to join and available to nurses and midwives everywhere.
From May 2022 it will be possible to access the virtual community via a smartphone, by downloading the Nursing and Midwifery Global Community of Practice App Nurses Beyond the Bedside_WHO_CSW66 Side Event available for Android and IOS system via the APP store.
A 2017 Report on the history of nursing and midwifery in the World Health Organization 1948 –2017, demonstrates how WHO, since its inception, has given this workforce a voice, and highlights the critical role nurses and midwives play in improving health outcomes across the world.
https://www.who.int/news-room/fact-sheets/detail/nursing-and-midwifery


Feb 8, 2024
Watch this amazing Scottish artist sing Yellow by Coldplay with me! @AndrewDuncan

Open Access to Neonatal Drug Development Education Modules
Mary A. Short MSN, RN – Volumn19/Issue 5 May 24

Critical Path Institute (C-Path) announces the launch of Bridging the GAP: Empowering Neonatal Nurses in Drug Development for Neonates, a comprehensive series covering the history of neonatal drug development, approaches to promote drug development for neonates, pharmaceutical industry decision-making processes, and strategies for advocating neonatal needs. Developed in collaboration between its International Neonatal Consortium (INC) and the National Association of Neonatal Nurses (NANN), this series aims to empower neonatal nurses and interested neonatal health care professionals with the knowledge needed to actively participate in research and ensure better outcomes for our tiniest patients.
“As an organization committed to advancing neonatal research and care, we recognize the vital role nurses and clinicians play in the hospital setting,” said INC Executive Director Kanwaljit Singh, MD, MPH. “This collaboration with NANN represents a pivotal step forward in our mission to support and empower neonatal nurses and clinicians. By engaging them in developing these educational modules, we aim to enhance their understanding and involvement in neonatal clinical trials and drug development.”
The modules aim to provide foundational knowledge on innovative, regulated medicines development for neonates, including pipeline decision-making factors and addressing neonatal needs within the current environment. Upon completion of the presentations and activity evaluations, participants can earn up to 4.5 FREE CE credits and 2.56 FREE pharmacology credits. NANN is an accredited provider of nursing continuing professional development recognized by the American Nurses Credentialing Center’s Commission on Accreditation. The content is appropriate for AMA PRA Category 2 Credit. The presenters reflect the diversity of neonatal stakeholders, as illustrated in Figure 1, which outlines the module titles and the presenters involved.
Background:
Neonates are therapeutic orphans, underserved by the drug development community, and lag in the development of new, safe, and effective therapies. Most NICU drugs are off-label, impacting their safety and efficacy evaluation. Nurses play a vital role in administering medications and monitoring their effects but often lack a comprehensive understanding of clinical trials and drug development processes in the NICU. Critical Path Institute (C-Path) is an independent nonprofit established in 2005 as a public-private partnership in response to the FDA’s Critical Path Initiative. C-Path’s mission is to lead collaborations that advance better treatments for people worldwide. Globally recognized as a pioneer in accelerating drug development, C-Path has established numerous international consortia, programs, and initiatives that currently include more than 1,600 scientists and representatives from government and regulatory agencies, academia, patient organizations, including parent/family advocates, nursing organizations, disease foundations, and pharmaceutical and biotech companies. INC, established in 2015 as a public-private partnership within the construct of C-Path, advances the unmet drug development needs in the neonatal population.
INC conducted a multistakeholder (neonatologists, neonatal nurses, parents) survey to explore communication practices and stakeholders’ perceptions and knowledge regarding the conduct of clinical trials in the NICU. Survey results indicated that most neonatologists (82%) responded that medications are insufficient to meet the needs of critically ill neonates and identified a knowledge gap for nurses regarding drug development. Degl et al. conclude that the engagement of nurses at all stages of neonatal research is suboptimal and indicates a need for nurses to be educated about research. Beauman et al. report additional findings specific to nurse respondents from the multistakeholder survey. Nurses expressed a learning need because they historically lacked effective education to prepare them for competent participation in neonatal research, especially in informing study design. The authors recommend leveraging neonatal nurses’ unique and essential role as key stakeholders from the onset of the study design to enhance the conduct of neonatal clinical research and improve care for premature and sick neonates.
To address the survey findings, industry representatives held an education workshop on Pharmaceutical Drug Development for Neonates at the 2019 INC Annual meeting intended for all neonatal stakeholders, including academics, clinicians, and regulators. The INC Communication Workgroup updated the content for the recently launched education modules, emphasizing the significance of the information for nurses, but the content remains relevant to other neonatal healthcare professionals.
Product Description:
“Consistent with our mission to elevate and transform neonatal care, NANN is grateful to bring forth this important collaboration with INC and give all neonatal nurses access to these outcome improving modules,” said NANN Executive Director Molly Anderson. “We know neonatal nurses have the expertise and knowledge to play an essential role in drug development that benefits their patients. NANN seeks out partnerships with organizations like INC that allow us to empower deepened nurse involvement with all aspects of care throughout their careers.”
The series includes access to seven on-demand video modules related to nurse-informed neonatal study design for drug development to provide context for the importance and implications for neonatal nurses. The NANN iLEARN site provides a platform for open access. Share the product flyer with colleagues to provide the QR code for access.

Free Preemie/Premature Baby Knitting Patterns

Jan 31, 2021 Kay Lloyd
Free patterns. Great for a beginner or just someone who wants to make for local maternity/neo natal hospital.


HEALTHCARE PARTNERS

Neonatal Nurse and Nurse Practitioner Engagement in Antibiotic Stewardship
A Call to Action
Zukowsky, Ksenia PhD, CRNP, NNP-BC; Editorial Board Member; Savin, Michele Kacmarcik DNP, APRN, NNP-BC, CNE, FAWHONN; Assistant Professor Director; Manning, Mary Lou PhD, CRNP, CIC, FAPIC, FSHEA, FAAN; Professor Director
Advances in Neonatal Care 24(3):p 209-211, June 2024. | DOI: 10.1097/ANC.0000000000001168
Metrics
Antibiotics are life-saving drugs and essential for the treatment of many serious infections, but widespread inappropriate use is now common and has become a major contributor to the development of antibiotic resistance (ABR). ABR is an urgent global public health and socio-economic threat, generating calls for actions from the World Health Organization and the US Centers for Disease Control and Prevention (CDC). Left unchecked, ABR is poised to reverse a century of medical progress, rendering antibiotics ineffective in treating even the most common infectious diseases. Infants admitted to neonatal intensive care units (NICUs) are at high risk for the development and transmission of multidrug-resistant pathogens, particularly where hospital stays are prolonged because of prematurity or congenital anomalies.3 Worldwide, sepsis is the third leading cause of neonatal mortality, with antibiotic resistant pathogens responsible for approximately 30% of deaths.
Antibiotics are the most common medication prescribed in NICUs, with wide variability in use, regardless of the level of care or complexity of patients.5 On any given day, 40% of infants admitted to a NICU are prescribed antibiotics, with an estimated 90% exposed to antibiotics over the duration of their NICU stay. A recent study published in The Lancet Regional Health-Southeast Asia found that the most commonly prescribed antibiotics in Southeast Asia are now only 50% effective at treating sepsis and meningitis in newborns. Furthermore, there is increasing evidence that preterm infant antibiotic exposure is associated adverse outcomes including alteration in the intestinal microbiome, necrotizing enterocolitis, invasive fungal infections, retinopathy, and late-onset sepsis.5 Early life antibiotic exposure is also associated with future health problems including childhood obesity, asthma, allergic disorders, and inflammatory bowel disease. Therefore, it is important to find strategies to reduce antibiotic use in the NICU patient population.
ANTIBIOTIC STEWARDSHIP
According to the Society for Healthcare Epidemiology of America, the Infectious Diseases Society of America, and the Pediatric Infectious Diseases Society, the major objective of antibiotic stewardship (AS) is to achieve the best clinical outcomes related to antibiotic use while minimizing toxicity and other adverse events, thereby limiting the emergence of ABR bacterial strains. AS – a core strategy to combat ABR – is intended to ensure patient safety through the implementation of combined, coordinated interprofessional interventions to optimize how antibiotics are used. Studies indicate that the implementation of AS initiatives in NICUs is associated with a significant decrease in the overall days of therapy and reduction in use of broad-spectrum antibiotics, such as cephalosporins, without adverse issues. However, significant gaps exist between CDC recommendations to improve antibiotic use and antibiotic practices during the neonatal and newborn period. Until recently, AS interventions focused primarily on improving clinician antibiotic prescribing practices through formulary restriction and prospective audit with feedback. However, with more nurses in the frontline of healthcare than any other healthcare profession, the CDC, the American Nurses Association (ANA), the International Council of Nurses and The Joint Commission, have endorsed nurses’ active participation in AS activities to expand the reach and impact of stewardship programs. A recent survey of NICU nurses found that most were familiar with the term AS, yet over half reported administering an antibiotic to a patient who they thought was an inappropriate choice and most reported not questioning the treating provider about antibiotic choice, dose or route of administration.
THE ROLE OF NEONATAL NURSES AND NEONATAL NURSE PRACTITIONER IN ANTIBIOTIC STEWARDSHIP
As trusted professionals, expert clinicians, and advocates for their patient’s health, neonatal nurses and neonatal NPs are well qualified to make significant contributions to the reduction of ABR through active engagement in AS. There are multiple AS activities to consider now.
- Advance your knowledge. Read the articles cited in this editorial. Participate in educational opportunities (eg, grand rounds, seminars, webinars) to advance your antibiotic, ABR and AS knowledge. Learn with and from others by starting an interprofessional AS journal club or lunch-and-learn at your practice setting. Contact the National Association of Neonatal Nurses and encourage them to provide state-of-the-science ABR and AS educational sessions specific to neonatal care and evidence-based antibiotic prescribing.
- Advocate for the adoption and evaluation of at least one nurse driven AS recommended action in your practice setting. Many preterm infants who do not have infections receive antibiotic treatment in the setting of negative cultures. Consider implementing daily antibiotic timeouts.
- Antibiotic time-outs involve a daily formal antibiotic review, often conducted during clinical rounds, to determine if a modification or discontinuation of a patient’s antibiotic therapy is warranted. The time-out approach is in keeping with nurse engagement in prevention of central line-associated bloodstream infections, which includes a daily formal review of central line necessity. Bedside neonatal nurses are well positioned to lead reassessment of antibiotic treatment for they know how long a patient has been receiving antibiotic(s) and when diagnostic test results become available. For additional examples of nursing interventions that may have an important impact on promoting nurse engagement, read the recommendations from the ANA/CDC Workgroup and an article providing a framework to guide AS nursing practice.
- Become an antibiotic stewardship champion. Neonates are entitled to receive antibiotic therapy that is based on evidence and best practice, but might be overlooked in hospital AS programs. Build and strengthen partnerships and facilitate communication between the NICU clinical staff and your organization’s AS team (physicians, clinical pharmacists, clinical laboratory personnel). Reach out to the AS team to learn about the overall AS program and specific AS NICU strategies. Engage and educate NICU staff about AS to increase their buy-in and awareness of nursing-related AS practices. Consider AS within the tenets of patient safety, and promote local-level “stewarding” behaviors that tap into the interprofessional NICU team’s collective knowledge, expertise, relationships and wisdom.15 NICU AS nursing practices should be intentionally selected, and strategically align with the organization’s AS program, giving ample consideration to the local context and tailored to the needs and resources of the NICU patients and clinical setting.
- Monitor your antibiotic prescribing practices. A core AS strategy is tracking and reporting of provider antibiotic prescribing. Audit and feedback, includes analyzing antibiotic prescribing data and providing feedback to clinicians aimed at helping them understand their antibiotic prescribing habits. These data are most effective when individual results are compared to other clinicians in the clinician’s area and/or specialty (e.g., NNP peer comparisons). If you are a prescriber and are not receiving peer comparison audit and feedback data, work closely with your practice colleagues to develop a process to audit patterns of antibiotic prescribing to gauge appropriateness.
- Use evidence-based clinical decision support systems. Clinical decision support systems are electronic tools or software that provide guidance to providers in making both diagnostic and therapeutic choices for patients.16 Applications range from pop-up reminders during a patient encounter, to automated order entry, to electronic guides, including dynamic interactive programs that tailor guidelines to specific patients. Such systems can be particularly useful when applied to antibiotic prescribing. Engage and partner with the NICU clinical team to identify the most useful systems to enhance clinical guideline adherence, decrease antibiotic consumption, or narrow the spectrum of antibiotic usage.
ABR has been aptly described as a subtle, slow moving catastrophe. AS programs aim to optimize antibiotic use to prevent the emergence of resistant pathogens and protect patients from the adverse effects of unnecessary antibiotics. We posit that all NICU nurses have a central role to play in the safe and responsible use of antibiotics and suggest several strategies for NICU nurses to engage in preventing unnecessary antibiotic exposure in this highly vulnerable population. We encourage you to seize the moment and become active, engaged stewards!

First Day of Neonatology


NICU Volunteer Coordinators Are Indispensable
Jennifer Degl, MS, Deb Discenza, MA, Mitchell Goldstein, MD, MBA, CML
In contemporary healthcare settings, the role of a Neonatal Intensive Care Unit (NICU) Volunteer Coordinator is indispensable, as it embodies the essence of compassionate care and community support for families navigating the challenges of premature births and neonatal health complications. While volunteer coordinators are often relied upon to fulfill this critical role, it is imperative to recognize the value they bring to the table and advocate for establishing a paid position dedicated to this noble cause.
Parents experience trauma regardless of what level NICU their baby is in and no matter the length of their NICU stay, and so it is vital that we push for a national campaign to address the inequity in order to help families bond and start the healing process before discharge. Not doing so can lead to trauma-related family issues at home. Currently, we largely focus on preparing parents for discharge across all things involving care of the infant. Why would we leave out the important topic of mental health Not addressing this important issue is tantamount to failure for that infant’s long term outcome, not to mention the outcome of the family unit as well. A NICU Volunteer Services Coordinator can alter that trajectory.
The NICU Volunteer Services Coordinator serves as a beacon of hope and support for families enduring the emotional rollercoaster of having their newborn hospitalized. This position encompasses a myriad of responsibilities aimed at fostering a nurturing environment within the NICU, where families feel empowered and supported throughout their journey. From recruiting additional NICU graduate parents to serve as volunteers to organizing crucial training sessions on mental health first aid and active listening, the coordinator plays a pivotal role in equipping volunteers with the necessary skills to provide invaluable support to NICU families.
Furthermore, the coordinator is a liaison between volunteers, nursing staff, and physicians, ensuring seamless communication and collaboration for improving patient care. Facilitating regular meetings and educational events creates opportunities for peer to-peer support among parents and disseminates vital information on neonatal care practices, empowering families to make informed decisions regarding their child’s healthcare journey.
The significance of celebrating milestones and raising awareness cannot be overstated in the NICU setting. The coordinator spearheads initiatives such as NICU Awareness Month/Day and World Prematurity Month/Day, fostering community and solidarity among NICU families and staff. Moreover, their involvement n fundraising activities and grant writing endeavors ensures continued access to resources and services that benefit NICU babies and their families, underscoring their dedication to enhancing the quality of care provided.
Regarding qualifications and working conditions, the NICU Volunteer Services Coordinator must possess a unique blend of empathy, organizational acumen, and leadership skills. While a post-secondary education degree serves as a foundation, firsthand experience as a parent of a NICU graduate and previous involvement in peer mentoring or emotional support roles are invaluable assets. The flexible nature of the position, with a combination of on-site and remote work, accommodates the dynamic needs of NICU families while ensuring that the coordinator remains accessible and responsive to their concerns.
Crucially, advocating for a paid position for the NICU Volunteer Services Coordinator acknowledges the intrinsic value of their role and underscores the commitment of healthcare institutions to prioritize patient-centered care and community engagement. By investing in this position, hospitals enhance the support provided to NICU families and cultivate a culture of compassion and collaboration that is essential for fostering positive health outcomes.
In conclusion, establishing a paid position for the NICU Volunteer Services Coordinator is not merely a bureaucratic formality but a testament to the unwavering commitment of healthcare institutions to uphold the highest standards of patient care and support. By recognizing the invaluable contributions of these dedicated individuals, we affirm our collective responsibility to ensure that every NICU family receives the compassion, guidance, and support they deserve during their journey toward healing and hope. And in the end, the hospital, as a whole, wins substantially through quality improvement scores and community appreciation. It is worth the investment because the benefits are tenfold.

Midwifery Review: Adding Care by Midwives Improves Birth Outcomes

August 15, 2023 – by Robert Forman
Midwife care can improve pregnancy outcomes for mothers and babies, says new “Expert Review” from Yale faculty
The practice of midwifery is less common in the United States than in other countries and other cultures, which is a shame because adding care by midwives generally improves childbirth outcomes, according to two Yale faculty members who have published an “Expert Review” in the American Journal of Obstetrics & Gynecology. Holly Powell Kennedy PhD, MSN,CNM, the Helen Varney Professor of Midwifery, and Joan Combellick, PhD, MPH,CNM, assistant professor of nursing, along with their colleagues, examined the scientific literature related to midwifery and childbirth, and conclude that many measures of successful pregnancy are elevated when midwives play a central role.
They cite the approach to midwifery that is standard in other countries, especially in wealthy European nations, where women have as much as seven times the access to midwives that they do in the United States. They report that midwifery care has improved outcomes by 56 different measures—including lower morbidity and mortality among mothers and newborns, fewer preterm births and low birthweight infants, and reduced interventions in labor.
The authors acknowledge that differences in those countries’ overall health systems make a substantial contribution to good outcomes, but say it’s the integral role of midwives that matters most. “In other countries, midwives make up the basic maternity care provider workforce, and then, obstetricians are used as the specialists that they are, surgeons who are there to handle complications,” says Combellick. “[Midwives] are the experts in normal childbirth, which happens the majority of the time.” Combellick adds that midwives also extend their care beyond pregnancy. “We also do well-person preventive care, across the lifespan from teenagers through postmenopausal people, so it isn’t only pregnancy-related.”
The Value of Midwives at the Baby’s Arrival
But the continuum of pregnancy, birth, and postnatal care is what midwives are best known for, and where the contribution of midwives can differ sharply from what is often considered standard care. Kennedy says a very basic way that outcomes can improve is because prenatal care by midwives is not squeezed into appointments of a set duration, where the provider may not have the time to fully answer the patient’s questions. Kennedy notes that in some settings, midwives caring for a woman throughout the pregnancy bring continuity and can structure longer appointments. Having more time permits building better rapport with a mother-to-be and helps her feel more respected, which often translates into a smoother pregnancy.
“In our paper, we discuss some of the research done about respect. It’s true for any kind of health care, but particularly in prenatal care,” says Kennedy. “It can amount to being highly disrespected and simply having to wait two hours for a very short prenatal visit. If people aren’t feeling respected or safe, they’re less likely to keep coming in for prenatal care.” Combellick adds that this can be especially true for women of color, for whom the cumulative race-based disrespect they endure in their daily lives can make the pressures of pregnancy more intense.
When the time for delivery arrives, a few statistics are especially striking. First-time mothers giving birth at medical centers where midwives were on their care team were 74% less likely to have their labor induced, 75% less likely to receive oxytocin augmentation, and 12% less likely to deliver by cesarean than their counterparts at medical centers without midwives in attendance.
Midwives and Ob/gyns Collaborate During Childbirth
Combellick says that on a collaborative team, the pregnant person is at the center of care, with everyone contributing their particular expertise. Whether to wait and allow labor to continue at its own pace, to induce, or to perform a cesarean can generally be a shared decision that involves patient understanding and consent. “We are collaborators,” says Combellick. “We work in conjunction with physicians. To have two viewpoints thinking about one person is a really strong style of care.”
At Yale, Kennedy and Combellick contribute to the midwifery faculty practice supporting student midwives as they learn. Faculty practice midwives are also active with obstetricians-in-training. “We contribute to the resident training program,” Combellick says. “So the residents, when they first come, are assigned to follow a midwife. Around the country, midwives often play a role in demonstrating ‘here’s what normal physiologic birth looks like,’ and that occurs at Yale.”
Hugh S. Taylor, MD, chair and Anita O’Keeffe Young Professor of Obstetrics, Gynecology & Reproductive Sciences at Yale School of Medicine, says this collaboration has been good for all involved. “It’s important that all of our practitioners get exposure and training on the collaborative practice model. The trainees participate in these teams and get a living example of how collaboration results in outstanding care. It was very important to establish that program—not only for patient care but for our residents and students.”
Taylor says that both for prenatal care and during deliveries, the presence of midwives on the care team can be invaluable. “Most of the prenatal care in our collaborative practice is delivered by midwives, with appropriate escalation and/or referral when things get complicated. If somebody develops diabetes or high blood pressure in pregnancy, we get the physician involved. However, for routine prenatal care or uncomplicated deliveries, we try to keep the physician in the background.”
Kennedy and Combellick both hope that the profile of midwifery in this country will rise, both through growing what Combellick now calls a “relatively small midwifery workforce” that attends only 10 to 12% of births in the United States, and by reforming practices related to health care delivery at large. “It’s not a simple, magical thing about the midwife,” Kennedy concludes, “but really about the model of care: that it’s accessible, it’s available, it’s respectful.” Those changes for the better, they say, would be nothing short of radical, and they are doing their part to gather the available evidence and advocate for change to happen.
https://medicine.yale.edu/news-article/the-value-of-midwives-during-prenatal-care-and-birth/
*** For you interested or involved in neonatal or pediatric surgery we found this interesting APP information


Course Support: Surgery Clerkship
Find clinical answers at the point of care or anywhere you need them! Now you can access UpToDate’s current, synthesized clinical information — including evidence-based recommendations — quickly and easily on your iPad, iPhone, or iPod touch.
Notes: To use the mobile app you must first create an UpToDate account. Use this link on the WCMC-Q network to create an account.
Do you need evidence-based answers to clinical questions at the point of care? The First Consult iPhone/iPad app is your solution. The app allows First Consult’s trusted answers to be stored on your iPhone, iPad, or iPod touch. A data connection is required for the initial content download and content updates, but is not required to use the app itself.
Notes: Log in with your ClinicalKey account created from a WCMC-networked computer.
DynaMed Plus™ is the clinical reference tool that physicians go to for answers to clinical questions. Content is written by a world-class team of physicians and researchers who synthesize the evidence and provide objective analysis. DynaMed Plus topics are always based on clinical evidence and the content is updated multiple times each day to ensure physicians have the information they need to make decisions at the point of care.
Note: To use this app begin by clicking on the “Get the DynaMed Plus Mobile App” link on the DynaMed Plus homepage. See this link for more information.
Surgery Speciality Clinical Apps
Touch Surgery, Surgical Simulator – Free
Touch Surgery is an interactive mobile surgical simulator that guides you step-by-step through every part of an operation, and every decision that’s made along the way. It’s the OR in your pocket.
Preop Eval organizes and presents much of the guidance that one needs in order to evaluate and prepare adult patients for non-cardiac surgery. It is based upon the guidelines on this topic from the American College of Cardiology of 2014, the European Society of Anaesthesiology of 2011, , and more. The app contains 1 algorithm and 3 resources: the cardiac evaluation algorithm, guidance on starting and stopping key medications in the perioperative period, guidance on timing of surgery after cardiac events, and guidance on preoperative testing. It also contains a review of preoperative evaluation mainly for students and residents.
AO Surgery Reference is an online repository for surgical knowledge. It describes the complete surgical management process from diagnosis to aftercare for all fractures of a given anatomical region, and also assembles relevant material that the AO has published before.
Surgery Apps for Patient Counseling
drawMD General Surgery’s content was developed by physicians and clinical practitioners to facilitate discussion of the most common conditions and procedures. The drawMD platform allows you to easily annotate any condition on our pertinent medical illustration or you can easily upload your own images.
*** This site also has All-Purpose Clinical APPs:
https://hslib-guides.qatar-weill.cornell.edu/c.php?g=364087&p=4181702

PREEMIE FAMILY PARTNERS
BABY BOX
In Scotland, we believe that parenting is one of the most important jobs in the world. The work we do preparing our children for the future will ultimately shape our world in the years to come. With that in mind, we want to make sure that Scotland was the best place in the world to grow up in. That’s why, in 2017, we launched the Baby Box initiative, which is designed to give every single baby in Scotland an equal start in life.

Parent Club: What’s in the Baby Box?

Scottish Government Jun 29, 2022
New babies need a surprising amount of stuff! Scotland’s Baby Box is packed full of clothes, bedding and lots of other useful things to help give your baby the best possible start in life
https://www.scotland.org/live-in-scotland/progressive-scotland/baby-box

Pathway 2: What are Maternity and Neonatal Psychological Interventions Teams? How can they help me?

INNOVATIONS

Prevention of Neurological Sequelae in Preterm Infants
by Eduardo Gonzalez-Moreira, Thalía Harmony, Manuel Hinojosa-Rodríguez, Cristina Carrillo-Prado,María Elena Juárez-Colín,Claudia Calipso Gutiérrez-Hernández, María Elizabeth Mónica Carlier, Lourdes Cubero-Rego, Susana A. Castro-Chavira, and Thalía Fernández / Published: 2 May 2023
Abstract
Background: Preterm birth is one of the world’s critical health problems, with an incidence of 5% to 18% of living newborns according to various countries. White matter injuries due to preoligodendrocytes deficits cause hypomyelination in children born preterm. Preterm infants also have multiple neurodevelopmental sequelae due to prenatal and perinatal risk factors for brain damage. The purpose of this work was to explore the effects of the brain risk factors and MRI volumes and abnormalities on the posterior motor and cognitive development at 3 years of age. Methods: A total of 166 preterm infants were examined before 4 months and clinical and MRI evaluations were performed. MRI showed abnormal findings in 89% of the infants. Parents of all infants were invited to receive the Katona neurohabilitation treatment. The parents of 128 infants accepted and received Katona’s neurohabilitation treatment. The remaining 38 infants did not receive treatment for a variety of reasons. At the three-year follow-up, Bayley’s II Mental Developmental Index (MDI) and the Psychomotor Developmental Index (PDI) were compared between treated and untreated subjects. Results: The treated children had higher values of both indices than the untreated. Linear regression showed that the antecedents of placenta disorders and sepsis as well as volumes of the corpus callosum and of the left lateral ventricle significantly predicted both MDI and PDI, while Apgar < 7 and volume of the right lateral ventricle predicted the PDI. Conclusions: The results indicate that preterm infants who received Katona’s neurohabilitation procedure exhibited significantly better outcomes at 3 years of age compared to those who did not receive the treatment. The presence of sepsis and the volumes of the corpus callosum and lateral ventricles at 3–4 months were significant predictors of the outcome at 3 years of age.
OPEN ACCESS ARTICLE HERE: Brain Sci. 2023, 13(5), 753; https://doi.org/10.3390/brainsci13050753 ; https://www.mdpi.com/2076-3425/13/5/753
New Gene Therapy Trial Shows Restored Hearing and Speech in Children Born Deaf, Treated in Both Ears
Administering gene therapy in both ears of five children with DFNB9 led to additional benefits compared to previous trial, including sound source localization and hearing in noisy environments.
Ryan Jaslow – Program Director, External Communications – Research, Mass General Brigham- rjaslow@mgb.org
06/05/24
Key Takeaways
- A new clinical trial in Shanghai, China, in partnership with Mass Eye and Ear researchers, demonstrated the restoration of hearing in both ears in five children born with autosomal deafness caused by mutations in the OTOF gene.
- All children gained ability to determine locations that sounds came from and improved speech perception in noisy environments.
- The trial is the first to provide gene therapy for this form of inherited deafness to children in both ears, and the researchers hope to expand this work internationally.
Boston, Mass. — A novel gene therapy designed to target a form of inherited deafness restored hearing function in five children who were treated in both ears. The children also experienced better speech perception and gained the ability to localize and determine the position of sound. The study, the world’s first clinical trial to administer a gene therapy to both ears (bilaterally), demonstrates additional benefits than what were observed in the first phase of this trial, published earlier this year, when children were treated in one ear. The research was led by investigators from Mass Eye and Ear (a member of the Mass General Brigham healthcare system) and Eye & ENT Hospital of Fudan University in Shanghai, and findings were published June 5th in Nature Medicine.
“The results from these studies are astounding,” said study co-senior author Zheng-Yi Chen, DPhil, an associate scientist in the Eaton-Peabody Laboratories at Mass Eye and Ear. “We continue to see the hearing ability of treated children dramatically progress and the new study shows added benefits of the gene therapy when administrated to both ears, including the ability for sound source localization and improvements in speech recognition in noisy environments.”
The researchers noted their team’s goal was always to treat children in both ears to achieve the ability to hear sound in three dimensions, a capability important for communication and common daily tasks such as driving.
“Restoring hearing in both ears of children who are born deaf can maximize the benefits of hearing recovery,” said lead study author Yilai Shu MD, PhD, professor, director of Diagnosis and Treatment Center of Genetic Hearing Loss affiliated with the Eye & ENT Hospital of Fudan University in Shanghai, “These new results show this approach holds great promise and warrant larger international trials.
Over 430 million people around the world are affected by disabling hearing loss, of which congenital deafness constitutes about 26 million of them. Up to 60 percent of childhood deafness is caused by genetic factors. Children with DFNB9 are born with mutations in the OTOF gene that prevent the production of functioning otoferlin protein, which is necessary for the auditory and neural mechanisms underlying hearing.
This new study is the first clinical trial to use bilateral ear gene therapy for treating DFNB9. The new research presents an interim analysis of a single-arm trial of five children with DFNB9 who were observed over either a 13-week or 26-week period at the Eye & ENT Hospital of Fudan University in Shanghai, China. Shu injected functioning copies of the human OTOF transgene carried by adeno-associated virus (AAV) into the inner ears of patients through a specialized, minimally invasive surgery. The first case of bilateral treatment was conducted in July 2023. During follow-up, 36 adverse events were observed, but no dose-limiting toxicity or serious events occurred. All five children showed hearing recovery in both ears, with dramatic improvements in speech perception and sound localization. Two of the children gained an ability to appreciate music, a more complex auditory signal, and were observed dancing to music in videos captured for the study. The trial remains ongoing with participants continuing to be monitored.
In 2022, this research team delivered the first gene therapy in the world for DFNB9 as part of a trial of six patients in China treated in one ear. That trial, which had results published in The Lancet in January 2024, showed five of six children gained improvements in hearing and speech. Shu initially presented the data at the 30th annual congress of European Society of Gene and Cell Therapy (ESGCT) in Brussels, Belgium in October 2023, becoming the first in the world to report clinical data on using gene therapy to restore hearing.
“These results confirm the efficacy of the treatment that we previously reported on and represent a major step in gene therapy for genetic hearing loss,” said Shu. Shu trained under Chen for four years as a postdoctoral fellow at Mass Eye and Ear, with their collaboration continuing for more than a decade since he returned to Shanghai.
“Our study strongly supports treating children with DFNB9 in both ears, and our hope is this trial can expand and this approach can also be looked at for deafness caused by other genes or non-genetic causes,” added Chen, who is also an associate professor of Otolaryngology–Head and Neck Surgery at Harvard Medical School. “Our ultimate goal is to help people regain hearing no matter how their hearing loss was caused.”
Currently, there are no drugs available to treat hereditary deafness, which has made room for novel interventions like gene therapies.
Mass General Brigham’s Gene and Cell Therapy Institute is helping to translate scientific discoveries made by researchers into first-in-human clinical trials. Chen and his colleagues are working with the Institute to develop platforms and vectors with good manufacturing practice standards that would enable his team to more easily test this therapeutic approach with other genes in the future.
The authors note that more work is needed to further study and refine the therapy. The bilateral study requires more consideration compared to the unilateral (one-ear) study as operations in both ears, in the course of one surgery, doubles the surgical time. Furthermore, by injecting double doses of AAVs into the body, the immune response is likely to be stronger and the potential for adverse effects could be greater. Looking ahead, more patients as well as a longer follow-up duration are necessary, and continued analysis of gene therapies and cochlear implants in larger randomized trials will be valuable.
Paper cited: Wang, H et al. “Bilateral gene therapy in children with autosomal recessive

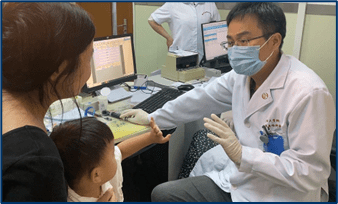
Research shows comforting babies eases parental stress in painful procedures
HEALTHMEDICAL SCIENCES 11 MAR 2024
The Neuroimaging Group, at the Department of Paediatrics, in collaboration with Bliss, the charity for babies born premature or sick, has launched a new suite of information resources for parents of neonates, designed to make them feel more confident about being involved in the care of their babies.
While evidence demonstrates that parents can play a positive role in comforting their baby during painful procedures, practice in the UK lags far behind. However new research by the Neuroimaging Group, published in the Lancet Child & Adolescent Health and Pain has brought further proof of the positive impact that being involved in their baby’s care has on parents.
The Parental touch trial (Petal) aimed to assess whether parental touch at a speed of approximately 3 cm/s to optimally activate C-tactile nerve fibres, provides effective pain relief during a heel-prick procedure. While there was no difference in the babies’ brain, behavioural or heart rate response to pain regardless of whether the parent touched their baby before or after the painful procedure, the findings did demonstrate that the majority of parents had positive emotions when involved in their child’s care – such as feeling useful and reassured – and an overall decrease in parental anxiety after their participation.
These new resources, a combination of beautifully curated and informative videos, FAQs and online information content, have been developed in light of the collaboration with parents and healthcare professionals. They are free to access online and set out in detail the many ways that parents can touch and comfort babies of all gestations during painful procedures on the neonatal unit, including skin-to-skin care.
Commenting on the research in an accompanying Lancet Child and Adolescent Health editorial, Ruth Guinsburg, said: ‘This study is an example of excellence in research. The trial was carefully designed with a clear question, strict inclusion and exclusion criteria, a well-designed and reproducible intervention based on biological plausibility, and defined outcomes, with the strength of using an objective rather than a subjective measure of pain. Only with trials like this might we transform faith in scienceand test the efficacy of traditional aspects of parental care in order to incorporate them, or not, in bundles to alleviate the pain in neonates.’
Dr. Rebeccah Slater, Professor of Paediatric Neuroscience and Senior Wellcome Fellow at the Neuroimaging Group, said: ‘Working with parents, babies and healthcare professionals to better understand how we can support premature and sick babies during painful procedures has been a highlight of my career. Developing these resources with Bliss has placed families at the heart of all the research we do, and has directly improved our engagement with families and the quality of our research. We will continue to find new ways to support parents and their babies when painful procedures form an essential component of neonatal care.’
Dr. Roshni Mansfield, a Paediatrics trainee and NIHR Academic Clinical Fellow in the Paediatric Neuroimaging Group said: ‘The Petal trial has highlighted the importance of involving parents in the provision of care and comfort for relieving their child’s pain. Future studies can build upon the insights gained from this trial including the positive parental experiences observed in this study. Prospective research might, for example, exercise a more spontaneous approach to delivering the gentle touch, such as allowing parents to stroke their child at their own pace, for as long as they need to calm and comfort their child, rather than a more mechanical and precise application.’
Dr. Maria Cobo, a postdoctoral researcher who managed the trial, added: ‘Another positive aspect of the study was the high degree of involvement by both fathers (35%) and mothers (65%) in delivering the parental touch to their babies. This contrasts with many studies, where only mothers’ opinions and involvement have been sought.’
Caroline Lee-Davey, Chief Executive of Bliss, said: ‘We are thrilled to have worked alongside the amazing team of researchers at the University of Oxford to further our understanding on the importance of parental involvement in their babies’ neonatal care. We know that babies have the best chance of survival and quality of life when their parents are empowered to be partners in their care but, sadly, we hear all too often that parents are not informed about their babies’ procedures or the role that they can have in comforting their baby. The outcomes of this research have directly shaped a new suite of Bliss information for parents and healthcare professionals which will help to validate what families often instinctively know to be true – that no matter how unexpected or strange the neonatal environment can feel, they are still their baby’s parent and they have a vital role to play in their comfort and care.’
Additional funding from the Wellcome Trust enabled Bliss to develop these valuable resources for families, including new information, video content filmed at John Radcliffe Hospital’s neonatal unit giving precious insight into neonatal care, as well as translated flyers for neonatal units and a webinar for healthcare professionals on how to support parents to be involved in their babies’ procedures. These resources were created in collaboration with parents and healthcare professionals, and included a listening event with the Raham Project, a CIC supporting ethnic minority families, where four mothers shared their neonatal stories.

Global Collaboration


Empowering the Unsung Heroes: Siblings of NICU Warriors
When a baby is born prematurely or with critical health needs, the entire family is thrust into a world of uncertainty and emotional upheaval. While much attention is rightfully focused on the newborn and parents, siblings often navigate this journey with a unique blend of resilience and vulnerability. These brave siblings of preemie babies deserve recognition and support for the vital role they play in the family’s NICU journey.
Siblings of NICU babies often experience a whirlwind of emotions, from fear and confusion to jealousy and isolation. It’s essential to create an environment where their feelings are acknowledged, and their contributions celebrated. Simple actions, like involving them in care routines or creating special sibling-only times, can foster a sense of inclusion and importance. Encouraging open conversations about their fears and questions can also help them feel more connected and less isolated.
Educational resources tailored to siblings can also be beneficial. Books, videos, and activities that explain the NICU environment in age-appropriate terms can demystify the experience and reduce anxiety. These resources help siblings understand the medical aspects of their baby brother or sister’s care, making the hospital environment less intimidating. Providing clear and accessible information empowers siblings by giving them a sense of control and understanding in an otherwise overwhelming situation. Resources such as Hand to Hold, Bliss, Miracle Babies Foundation, and Canadian Premature Babies Foundation, offer valuable insights and practical tips for supporting siblings during this challenging time.
Recognizing the importance of supporting siblings of NICU babies is essential for fostering a positive family dynamic and ensuring the emotional health of all children involved. By acknowledging their unique experiences and providing targeted support, parents and caregivers can help these strong siblings navigate the complex emotions and challenges they face, contributing to the overall resilience and well-being of the entire family navigating the NICU journey.
These resources provide valuable insights and practical tips to help siblings navigate the complex emotions and experiences associated with having a brother or sister in the NICU:
Hand to Hold provides comprehensive resources to support siblings of NICU babies, including tips for preparing siblings for NICU visits and strategies for making them feel included in their baby brother or sister’s care.
https://handtohold.org/resources/siblings
Bliss (UK): Support for Siblings
Bliss is a UK-based charity that provides comprehensive support for families of premature and sick babies. They offer resources and guidance specifically designed for siblings, including advice on how to involve them in the care process and ways to help them understand and cope with the NICU environment.
https://www.bliss.org.uk/parents/support/siblings
Miracle Babies Foundation (Australia): Sibling Support
Miracle Babies Foundation is an Australian organization dedicated to supporting premature and sick newborns, their families, and the hospitals that care for them. They provide resources tailored for siblings, helping them navigate the emotional and practical challenges of having a brother or sister in the NICU.
https://www.miraclebabies.org.au/parents-and-families/sibling-support/
Canadian Premature Babies Foundation Sibling Support
The Canadian Premature Babies Foundation (CPBF) offers a range of resources to support families of premature babies across Canada. They provide specific guidance and materials for siblings, including educational resources and support groups to help them cope with their sibling’s NICU stay.
https://www.cpbf-fbpc.org/sibling-support

Boy’s Heart Melts As He Meets Baby Sister After NICU Stay
Sep 11, 2023
A three-year-old boy who could not meet “his” baby sister while she spent her first days in the NICU lit up when he was finally able to hold her for the first time. Dominic “Dommy” Voso, from Rome, Georgia, told his parents the newborn would be “his” baby, having asked mom and dad for a sibling for a long time, proudly telling others when his mom was pregnant. But unfortunately for Dommy, mom Chrissy, 30, had preeclampsia during her pregnancy, which meant that Mia had be delivered at 35 weeks and four days. Mia then had trouble breathing, which caused her to spend her first 12 days in the NICU. This period was extremely tough for Dommy, as he had been desperate to meet his newborn sister, but only adults and siblings over 13 years of age could enter the NICU. Added to this difficulty, Chrissy had to spend an extra eight days in hospital, too, so Dommy couldn’t understand why he could see his mom but not his little sister. But that all changed on July 4 when Dommy sat in his family’s home and Chrissy came in holding Mia. When Dommy was then presented with his little sister, he immediately beamed with joy, holding her before bringing toys and books to share with her.


This inspiring video highlights the experiences and resilience of siblings of Preemie Warriors:

Scotland’s BEST Surfing Spots for Everyone

Let’s Travel! #scotland #travelchannel #scotlandtravel
Surfing Scotland, Thurso, surf trip UK, Surfing scotland West Coast, Surfing Scotland East Coast, Surfing Dunbar, Moray firth, December surf!


