Liberia, officially the Republic of Liberia, is a country on the West African coast. It is bordered by Sierra Leone to its northwest, Guinea to its north, Ivory Coast to its east, and the Atlantic Ocean to its south and southwest. It has a population of around 5.5 million and covers an area of 43,000 square miles (111,369 km2). The official language is English. Over 20 indigenous languages are spoken, reflecting the country’s ethnic and cultural diversity. The capital and largest city is Monrovia.
Liberia has 5,000 full-time or part-time health workers and 51 Liberian doctors to cater to a population of 3.8 million, according to the 2006 health survey. That’s the equivalent of one doctor serving about 76,000 civilians. Most of the hospitals, clinics and equipment were destroyed as a result of the 14-year civil war from 1989 to 2003. Strengthening the health sector faces financial problems. The government used only 16.8% of the total health expenditure in the country.
Liberia is heavily dependent on the international community for health infrastructure and assistance. International aid organizations assist the government in rebuilding medical facilities and providing basic health care to its citizens. The World Health Organization (WHO) donated equipment and helped provide and assist in vaccinating people to prevent the spread of many infectious diseases.
The Global Alliance for Vaccines and Immunization (GAVI) is investing $160 million to improve Liberia’s health care system and improve the quality of immunization services. The international medical humanitarian organization Médecins Sans Frontières (MSF) helped Liberia after the civil war (2003) by running free hospitals, treating more than 20,000 women and children each year.
Source: https://en.wikipedia.org/wiki/Liberia
- GLOBAL PRETERM BIRTH RATES – Liberia
- Estimated # of preterm births: 14 per 100 live births
- (Global Average: 10.6)
- Source- WHO Preterm Birth Rate (Per 100 Live Births)

COMMUNITY

Monrovia Liberia: Liberia has received a major boost to its healthcare sector as 26 leading medical professionals from the United States, Canada, Europe, and beyond have arrived for the Liberia Medical Mission (LMM) 2025. The mission, a special initiative led by President Joseph Nyuma Boakai’s administration, represents a transformative step toward improving healthcare delivery across the country.
As part of the mission, over $500,000 worth of life-saving medicines will be distributed across five counties, aligning with President Boakai’s vision for a healthier and stronger Liberia.
The mission’s launch was celebrated with a special reception at the Tea House, Executive Mansion in Monrovia, where President Boakai expressed deep gratitude for the medical team’s commitment to making a difference.
“This mission exemplifies the power of compassion and service,” President Boakai said. “You’ve left the comfort of your homes to bring healing and hope to our people. Liberia is truly grateful for your selfless contributions. My administration is committed to supporting and expanding this mission so that more lives can be saved.”
He reiterated the government’s dedication to modernizing Liberia’s healthcare system, ensuring that medical professionals and facilities are equipped to improve service delivery nationwide.
Expanding Medical Care Across Liberia’s Counties
The Liberia Medical Mission 2025 aims to provide essential healthcare services to thousands of Liberians in need. Over $500,000 worth of medicines will be distributed to hospitals and clinics in Gbarpolu, Cape Mount, Bomi, Grand Bassa, and Montserrado counties. The mission will provide the following critical healthcare services:
• Cataract Surgeries at Emirates Hospital: Restoring vision to patients from Gbarpolu, Bomi, Cape Mount, and Montserrado counties.
• Mental Health Awareness & Training: Focused on trauma-informed care, with training for healthcare workers, educators, and security agencies.
• CPR & Emergency Training: Aimed at enhancing life-saving emergency response skills for 7 security personnel.
• Biomedical Equipment Repairs: At John F. Kennedy Memorial Hospital and other key medical centers to improve service efficiency.
• Specialized Urology Surgeries: Performed by leading urologists at JFK Memorial Hospital.
This initiative is being led by Minister Mamaka Bility, the Minister of State Without Portfolio for Presidential Affairs, and is directly overseen by the President’s Delivery Unit (PDU). Minister Bility spoke on February 21, 2025, at the event, highlighting the government’s unwavering commitment to reshaping Liberia’s healthcare sector.
“This mission reflects President Boakai’s vision for a reformed healthcare system,” Minister Bility stated. “We are honored to host the Liberia Medical Mission again this year, as their critical services will touch and improve countless lives.”
Liberians Abroad Give Back to Their Country
Many of the medical experts participating in this mission are Liberians who have spent years abroad, gaining experience in their fields, and are now returning home to contribute to the development of their country’s healthcare system.
As the mission progresses, President Boakai has called on all Liberians to work together with the medical team to maximize its life-saving impact.
“This is a national effort, and every Liberian has a role to play in ensuring the mission’s success,” President Boakai said. “My administration remains dedicated to advancing healthcare policies and mobilizing resources to build a more resilient healthcare system for Liberia.”
The Liberia Medical Mission 2025 offers free medical checkups, surgeries, and other essential services at no cost to the government or private institutions, making it a crucial component in the country’s healthcare transformation.
A Step Toward a Healthier Liberia
The Liberia Medical Mission 2025 stands as a testament to the collective efforts of both international and Liberian medical professionals who are dedicated to improving healthcare in the country. With the government’s ongoing support, this initiative is set to deliver lasting benefits for thousands of Liberians in need of medical care.

The World Health Organization (WHO) has officially designated Health Canada, the Ministry of Health, Labour and Welfare/Pharmaceuticals and Medical Devices Agency (MHLW/PMDA) of Japan, and the Medicines and Healthcare products Regulatory Agency (MHRA) of the United Kingdom as WHO-Listed Authorities (WLAs), a status granted to national authorities that meet the highest international regulatory standards for medical products.
With these latest designations, WHO expands the growing list of WLAs, now involving 39 agencies across the world, supporting faster and broader access to quality-assured medical products, particularly in low- and middle-income countries (LMICs).
In addition, the Republic of Korea’s Ministry of Food and Drug Safety (MFDS) – one of the first regulatory authorities to complete the WLA assessment for both medicines and vaccines in October 2023 – has had its listing scope successfully expanded, now covering all regulatory functions.
“This recognition reflects the deep commitment of these authorities to regulatory excellence,” said Dr Tedros Adhanom Ghebreyesus, WHO Director-General. “Their designation as WHO-Listed Authorities is not only a testament to their robust regulatory systems but also a critical contribution to global public health. Strong and trusted regulators help ensure that people everywhere have access to safe, effective, and high-quality medical products.”
Around 70% of countries worldwide still face significant challenges due to weak or inadequate regulatory systems for evaluating and authorizing medical products. The WLA framework promotes regulatory convergence, harmonization and international collaboration, allowing WHO Prequalification Programme and regulatory authorities, especially those in LMICs, to rely on the trusted work and decisions of designated agencies. This collaboration supports efficient use of limited resources, enabling better and faster access to quality-assured life-saving medical products to millions more people.
“The principle of reliance is central to WHO’s approach to regulatory systems strengthening and a cornerstone for effective, efficient and smart regulatory oversight of medical products,” said Dr Yukiko Nakatani, WHO Assistant Director-General for Health Systems, Access and Data. “WHO-Listed Authorities are key enablers in promoting trust, transparency, and faster access to quality-assured medical products, especially in low- and middle-income countries.”
In a world where health threats, including substandard and falsified medical products, know no borders, WLAs also serve as critical pillars of preparedness and equity, making life-saving products available more broadly, rapidly and efficiently.
The designations follow a rigorous performance evaluation process carried out by WHO using its globally recognized benchmarking and assessment tools. These evaluations were reviewed by the Technical Advisory Group on WLAs (TAG-WLA), which convened in June 2025.
Canada, Japan and the UK’s regulatory authorities were previously recognized as Stringent Regulatory Authorities (SRAs). Their designation under the WLA framework marks an important step in moving beyond the old SRA system, while ensuring continuity and stability in global procurement processes of quality-assured medical products.
Launched in 2022 to replace the previous SRA model, the WLA initiative provides a transparent and evidence-based pathway for global recognition of regulatory authorities to facilitate regulatory convergence and reliance. It builds on decades of WHO leadership to help countries work together more closely on regulating medical products, speeding up access to safe, effective and quality-assured medical products for people around the world.


Here is our list of the best team building ideas for healthcare professionals.
Team building ideas for healthcare professionals are exercises, activities, and games that build morale and keep healthcare employees positive and engaged. Examples include daily positive affirmations, Secret Number, and Mystery Diagnosis. The purpose of these activities is to build healthcare teams that are motivated to best serve patients.
These exercises are examples of team building activities for technical teams, small group team building activities, team building exercises, and team building events.
This list includes:
- team building activities for caregivers
- communication activities for healthcare workers
- team building exercises for nurses
- team building ideas for doctors
- healthcare team building games
Let’s get started!
List of team building ideas for healthcare professionals
It is not uncommon for healthcare professionals to feel stress and fatigue when under constant pressure. As a result, healthcare leaders must engage in fun and meaningful team building exercises and activities with their teams. Here is our list of the top ideas to improve bonds between teams of healthcare workers.
1. Thanks and Gratitude Circle
If you want to boost communication activities for healthcare workers in your facility, then start by fostering a culture of recognition and gratitude on your team. Building and maintaining a positive work culture can lay the foundation for a strong and successful team of healthcare professionals.
There are different ways you can show gratitude toward your team and make a fun game out of it. Communication is key in any workplace, so we recommend conducting your gratitude activity by getting your entire team together at the end of each day.
You should begin by having all team members sit together in a circle. Then, you can go around the circle and have each employee express gratitude for one teammate. A great way to think about this exercise is to have each participant start with the words, “Today, I want to thank blank.” For example, you could say: “Today, I want to thank Amanda for going above and beyond in treating her patients and helping other members of the team who were struggling with their patients.”
This communication exercise is a meaningful way for all teammates to build camaraderie by sharing words of thanks and gratitude toward other team members. Communication exercises for recognition and appreciation are also a great way to end each day.
2. Daily Positive Affirmations
One of the most beneficial team building activities for caregivers is to practice positive affirmations at work.
Positive affirmations are phrases that can help you build yourself up and overcome negative thoughts.
Here are a few examples:
- I am making a difference.
- I will show kindness and empathy to every patient.
- I will care for myself as I care for my patients.
- I help others in their most vulnerable moments.
- I am energized and ready for the day.
- I will make today a great day.
- I am strong.
- I am proud of myself and the work I do.
Affirmations like these are ideal for all employees to stay motivated and positive. Caregivers must remain positive as they work with patients dealing with difficult and sometimes life-threatening diseases and disorders.
Positive affirmations can be a great help in allowing employees to free their minds and stay positive, even during a tough day at work. Plus, the whole team can collectively build their positivity and confidence by having employees recite positive affirmations together.
3. Coffee Chats and Tea Time
As a doctor, it can be challenging to make time to socialize with your team regularly. As a result, one of the best team building ideas for doctors is to set aside time each week to socialize with their team over a cup of coffee or tea.
Gathering in the break room with your team can provide the perfect opportunity to get to know each other and take a much-needed break in the middle of a busy day. To make your coffee chat and tea time a success, you should remember to stock up your break room with various coffees and teas.
In addition, you should make a goal for yourself to chat with a new coworker new each week. It can be tempting to talk to your well-known coworkers and friends, but by chatting with a new colleague each week, you will meet different teammates while building new relationships in your workplace.
4. Line Leader
When it comes to communication activities for healthcare workers, the exercise that may help your team most is a nonverbal communication game.
Nonverbal games are an effective way to build communication skills. Instead of relying solely on spoken words, healthcare professionals can learn to look at nonverbal cues and body language to decipher patients’ and colleagues’ needs and wants.
Line leader is a nonverbal communication game in which the group must form a line in a specific order without talking to each other. Instead, teammates must rely on silent cues and body language to get in the correct order while working together. The moderator is the only player allowed to speak in this game.
For example, the game’s moderator can ask the team to get in a line starting from January birthdays through December birthdays. In this case, the first player in the line should be the team member with the first January birthday, while the last player in line should be the member with the last December birthday.
Since players may not speak to each other, they must determine the correct order by using body language and signs. The game Line Leader is an ideal activity that can help healthcare professionals better understand the nonverbal communication cues they may receive from patients or colleagues.
5. Secret Number
A nonverbal communication game your team can play together is Secret Number. To play this game, you should break your group into two teams of three to ten players. These teams will ultimately compete against each other, and it is best if your teams are large.
You should begin the game by designating one player as the moderator. The game’s moderator should communicate instructions or guidelines to other players. The moderator should then give each team a piece of paper and a pencil.
Before the game officially begins, each team should devise a secret code to use throughout the activity. This secret code will come in handy when players get stumped, as they will not be allowed to speak with each other or write anything down.
You can use the following steps to ensure a smooth game:
- The moderator gives each team leader a “secret number.”
- Each leader should communicate this number to each member of their team one by one. However, the leader should not speak or spell out the number with their hands.
- As each team member reads the leader’s nonverbal clues, the player should write down their guess of the secret number.
- Once the team leader has communicated with each participant, they should signal to the moderator that their team is finished.
- The winner of the game is the team that finishes the fastest and can guess the correct number.
To keep the game exciting, you should switch team leaders for each turn so different players can have the opportunity to lead. Secret Number is a great way to get teams accustomed to nonverbal cues as they engage in friendly competition.
6. Care Packages
Among the different types of healthcare professionals in the workforce, nurses typically feel higher levels of stress and burnout. As a result, one of the most ideal team building exercises for nurses to combat burnout is to have the team leader send out care packages.
By sending care packages to your team, you are sending the message that you care about employee wellbeing.
Here are a few items you can include in your care packages for self-care:
- Herbal teas
- Bath bomb
- Face masks
- Candles
- Meditation subscription
- Positive affirmation cards
- Snacks
Assembling care packages is a great exercise to decrease burnout, boost morale, and increase employee satisfaction. A well-rested team of nurses is most likely to provide the utmost level of care to patients.
7. Question of the Day
One of the most classic healthcare team building games is icebreakers. This team building activity works well for new teams that are just meeting each other or teams that want to get to know each other better.
A great icebreaker to begin each shift with is Question of the Day. As part of this icebreaker exercise, designate one person on your team to come up with the day’s question. From there, the employee tasked with creating the question should kick off the icebreaker exercise by stating the question and their own answer. Question of the Day is a great icebreaker to help coworkers learn more about each other.
A few suggestions for Question of the Day prompts include:
- What is one important skill that all nurses should have?
- If you had an extra hour in your day, what would you do during that time?
- If you were not a nurse, what kind of job do you think you would have?
Icebreakers can help teams build unity by learning more about each other. Plus, when a team feels more united, they are more likely to excel in their roles and keep hospital operations running smoothly.
8. Workshops
Workshops provide an excellent opportunity to learn new things while spending time with coworkers. We recommend organizing monthly workshops that employees can attend throughout the work day or on their breaks.
Although the workshop may take place during the workday, it is important to know that these sessions do not have to be directly related to job training or building on-the-job skills. Instead, these workshops should focus on building camaraderie while promoting employees’ well-being.
Here are a few suggestions for the types of workshops that you can get your team excited about:
- Yoga and meditation
- Healthy habits
- Journaling
- Resume writing
- Networking
Each workshop will provide employees with the opportunity to decompress while learning new skills that can help them in their daily job.
9. Board Games
If you are looking for healthcare team building games to engage your group, start with board games. Board games are a fun and competitive way to get your team to interact.
Some suggestions:
- Monopoly
- Sorry!
- Trouble
- The Game of Life
- Taboo
- Operation
It can be a good idea to keep a handful of board games in your facility’s break room. Having easy access to a few board games allows your team to choose different options to play with teammates during their lunch break or at other team building events.
10. Escape Room
If you are looking for a team building activity that promotes problem-solving and resolution skills, then consider completing an escape room challenge. Escape rooms are activities in which teams are locked in a room full of puzzles and tasks that they must complete to escape.
To successfully complete an escape room, team members must communicate effectively to solve the many puzzles and challenges. You can find a variety of themes to meet the needs and interests of your whole team.
Fun escape room themes include:
- Mystery
- Science or high-tech
- Fantasy
- Horror or suspense
- Holiday
Although teammates may have differing perspectives and ideas, all players need to work together to escape the room within the given time frame. Escape rooms contain different puzzles and clues that teams must work together to solve, making this activity an optimal choice for a team of healthcare professionals looking to boost teamwork and trust.
11. Team Outing
Engaging with your team outside the workplace can provide a much-needed change of scenery while providing an opportunity to get to know each other and socialize more. Fun activities and team outings can help boost employee happiness and morale.
A few examples:
- Happy Hour
- Boat ride
- Fancy dinner
- Karaoke night
- Paint and sip class
- Science museum
- Art museum
When it comes to team building ideas for doctors, you cannot go wrong with visiting a science museum. In fact, a group of doctors may be especially excited to enjoy a trip to the local science museum and spend an afternoon learning and exploring.
12. Mystery Diagnosis
Role-playing is one of the best team building exercises for nurses that can help improve their patient care skills. To conduct a role-playing exercise with your team, you will need to choose one team member who will act as the doctor.
Here are a few steps to keep in mind when participating in this role-playing game with your team:
- You can start by having the team “doctor” leave the room. Once this player leaves, the rest of the team should come up with an illness or injury. The players should discuss symptoms and scenarios they can later share with the team’s doctor.
- When the doctor comes back into the room, they will diagnose the patient based on the information the remaining players share.
- To make the game challenging, you should give the doctor a timeframe of about 90 seconds to fully diagnose the patient.
- If the team doctor can provide the correct diagnosis in the given timeframe, then the doctor can be declared the winner. The other players win the game if the doctor fails to provide the correct diagnosis.
You can encourage your staff to act out rare and obscure diseases or illnesses to make the game even more fun. For example, some players may pretend to fall asleep while doing everyday activities. The doctor of the game would then need to understand why patients are exhibiting such strange behavior, and ultimately provide a diagnosis.
Role-playing can be helpful for nurses to build upon their analysis, critical thinking, and problem-solving skills. This role-playing exercise is also a great way for a team of nurses to improve their relationships with each other as a team.
13. Bake-Off
Having a team bake-off is a fun way for your team to show off their baking skills while building collaboration skills.
To host a team bake-off, you should split your group into teams of three. Next, have each team choose a pastry or dessert to bake together. You can provide a two-hour time limit for each team to bake their dessert.
Once the teams have finished baking, you should have a team of judges taste each creation to determine a winner. A team bake-off is a great team building exercise as you can get teammates in the kitchen with each other working together on a tasty dessert.
Conclusion
Team building exercises are a great way to get your team of healthcare professionals more comfortable with each other. These activities also have the power to motivate teams to work more efficiently and in sync with one another, especially when serving patients.
Overall, team building is essential for healthcare professionals and it is a great skill for all teams to master. By engaging in team building exercises, you are taking the right steps toward improving relationships between team members with each other, which can lead to happier employees and satisfied patients.
FAQ: Team building ideas for healthcare professionals
Here are answers to questions about team building ideas for healthcare professionals.
What are team building ideas for healthcare professionals?
Team building ideas for professionals are activities that build camaraderie among healthcare teams while keeping employees motivated and happy. Healthcare professionals need to build their team’s morale and collaboration skills with each other both in and out of the workplace. As a result, team building exercises and activities come in handy when you are looking to form a stronger and more united team.
What are some good team building ideas for healthcare professionals?
There are many team building ideas to engage healthcare teams. Here are a few examples of team building exercises and activities for healthcare professionals:
- Icebreaker
- Coffee break
- Team outing
- Escape rooms
Team building activities can motivate employees to work effectively as a team, which can also help employees when they are caring for patients or working hard to solve a problem.
How do you encourage teamwork on healthcare teams?
It is important to encourage your team to work efficiently and collaboratively. A creative way to encourage teams to work together is by organizing team building activities for caregivers and other healthcare professionals.
Team building activities are sure to get your entire team working together as they have fun.
Source: https://teambuilding.com/blog/healthcare-team-building

PREEMIE FAMILY PARTNERS

If a baby is born before 37 weeks, they’re considered a preemie, and their senses might develop a bit differently from those of full-term babies. This doesn’t mean you need to worry! Knowing this can help you better understand and support your little one! During pregnancy, babies develop their senses in a specific order: touch, movement and balance, smell, taste, hearing, and vision. But once they’re born, these senses begin to work in reverse order. This means your preemie’s vision and hearing are quickly adjusting to the lights, sounds, and new environment around them. Preemies have their milestones adjusted for their corrected age, but their visual development might align more closely with their actual age. To help your baby’s vision, use toys with black, red, and white colors—these are easiest for them to see in the early months.

There are many different members of the health care team that you may meet in the NICU. Besides a bedside nurse, every baby has a NICU medical team managing the overall care of your baby. Each team is supervised by an attending neonatologist. Below is some basic information on the other members of your health care team.
Attending Neonatologists: Doctors who specialize in the care of newborns (neonates).
Chaplains: Give emotional and spiritual support to families and patients of all faiths and
cultures.
Clinical Leaders and Charge Nurses: Senior staff members who are able to take care of any problems or concerns.
Fellows: Doctors that are training to be neonatologists.
Lactation Team: Trained to help you reach your breastfeeding goals and answer any pumping/breastfeeding questions.
Licensed Practical Nurses (LPN): A nurse who works under the supervision of an RN to provide direct patient care. LPNs give much of the same care as RNs, except they do not give IV medicines.
Neonatal Nurse Practitioners (NNP): A nurse who has finished advanced graduate education and training. A NNP can help the Attending Neonatologists and Pediatric Surgeons treat babies and perform certain procedures.
Nurse Case Managers: Registered Nurses who provide care coordination for you and your baby while you are at the hospital. They will also help with the discharge process.
Nutritionists /Dieticians: Make sure babies are getting the right amount of calories and nutrients for the best growth and development. They will also give nutrition education for special diet needs.
Occupational Therapists (O.T.) and Physical Therapists (P.T.): Focus on babies’ movements and motor development. An O.T. may also help with feeding and oral stimulation.
Parent Advisors: Other parents who have had babies in the NICU. They give emotional support to families. Also, they lead the weekly Parent Pizza Night.
Patient Care Assistants (PCA): Also known as Patient Support Assistant (PSA), they work under the supervision of an RN. They can take vital signs, perform heel sticks, give baths, and feed babies.
Pharmacists: Help the doctor prescribe drugs for your baby. They also watch how well the drugs work for your baby and make sure the drug levels are right in the blood.
Registered Nurses (RN): Nurses who specialize in the nursing care of your baby. They assess your baby’s condition and progress and carry out the doctor’s orders. The RN will tell the doctor or NNP if there are any changes in your baby’s condition.
Residents: Doctors who are training to become pediatricians (a doctor who cares for children).
Respiratory Therapists: Manage and adjust the ventilators and other breathing equipment. They perform treatments that help with breathing and lung function.
Social Workers: Give emotional support, crisis intervention, information on community resources, and help with communication between families and the medical team.
Unit Clerks: Often the first people you meet when you enter the NICU. They answer the phone when you call to check on your baby and take care of many of the NICU’s administrative needs.
Volunteers: NICU volunteers have attended special training, and they help with many different tasks in the unit. They can hold and rock babies (if you wish) when parents are not able to.





HEALTHCARE PARTNERS
Tiny fingers grasp at invisible demons as the sterile beeps of hospital monitors become the haunting soundtrack to a newborn’s first memories. This haunting image raises a profound question: Can babies experience Post-Traumatic Stress Disorder (PTSD) from birth? As our understanding of infant mental health grows, researchers and healthcare professionals are increasingly exploring the possibility that even the youngest among us may be vulnerable to the lasting effects of trauma.
PTSD, a mental health condition triggered by experiencing or witnessing a terrifying event, has long been recognized in adults. The American Psychiatric Association reports that approximately 3.5% of U.S. adults are affected by PTSD in any given year. However, the concept of PTSD in infants is a relatively new area of study, challenging our preconceptions about early childhood experiences and their long-term impacts.
As we delve deeper into the realm of infant mental health, it becomes crucial to consider the potential for trauma during the earliest stages of life. The birth process itself, along with the immediate postnatal period, can be a source of significant stress for newborns. This realization has led to a growing awareness of the importance of nurturing infant mental health from the very beginning.
The Possibility of PTSD in Babies: Exploring the Evidence
Current research on infant PTSD is still in its infancy, but emerging studies suggest that babies may indeed be capable of experiencing trauma-related stress responses. While the traditional diagnostic criteria for PTSD were developed with adults in mind, researchers are now adapting these frameworks to better understand and identify trauma in non-verbal infants.
One of the primary challenges in diagnosing PTSD in babies lies in their inability to verbalize their experiences and emotions. Unlike adults who can describe their symptoms and traumatic events, infants communicate their distress through behavioral and physiological cues. This necessitates a different approach to identifying and assessing trauma in the youngest patients.
Despite these challenges, healthcare professionals have identified several signs and symptoms that may indicate trauma in babies. These can include heightened startle responses, difficulty sleeping, excessive crying or irritability, and problems with feeding. Some infants may also exhibit a withdrawal from social interactions or show signs of hypervigilance, constantly scanning their environment for potential threats.
It’s important to note that while these symptoms may be indicative of trauma, they can also be associated with other developmental or medical issues. This underscores the need for comprehensive assessments and a nuanced understanding of infant behavior and development when evaluating potential trauma responses.
Potential Causes of Birth-Related Trauma in Infants
Several factors during the birth process and immediate postnatal period can potentially contribute to trauma in newborns. Complicated or traumatic deliveries, such as those involving emergency cesarean sections, forceps, or vacuum extraction, may be particularly stressful for infants. These interventions, while often necessary for the safety of mother and child, can introduce an element of physical and emotional distress that may have lasting effects.
Premature birth is another significant risk factor for infant trauma. Babies born before 37 weeks of gestation often require extended stays in the Neonatal Intensive Care Unit (NICU), exposing them to a range of stressful experiences. The NICU Stays and Babies: Long-Term Effects, Impact, and Potential for PTSD can be profound, influencing both physical and psychological development.
Separation from parents immediately after birth can also be a source of distress for newborns. The importance of early bonding and skin-to-skin contact is well-documented, and disruptions to this process may contribute to feelings of insecurity and anxiety in infants. This separation is often unavoidable in cases of medical emergencies or when babies require specialized care, but its potential impact on infant mental health should not be overlooked.
Medical interventions and procedures, while often life-saving, can be another source of trauma for newborns. Frequent blood draws, intubation, and other invasive procedures can be painful and frightening for infants, potentially contributing to a heightened stress response and increased risk of trauma-related symptoms.
PTSD in NICU Babies: A Closer Look
Babies who spend time in the Neonatal Intensive Care Unit (NICU) face unique challenges that may increase their vulnerability to trauma-related stress. The NICU environment, while designed to provide life-saving care, can be overwhelming for fragile newborns. Constant noise from medical equipment, bright lights, and frequent handling can disrupt an infant’s developing sensory systems and sleep patterns.
Research on the long-term effects of NICU stays on infant development has revealed a range of potential impacts. These can include delays in cognitive and motor development, difficulties with emotional regulation, and increased risk of behavioral problems later in childhood. While not all NICU graduates will experience these challenges, the potential for lasting effects underscores the importance of trauma-informed care in these critical early days.
Studies examining PTSD symptoms in NICU graduates have yielded intriguing results. A study published in the Journal of Perinatology found that infants who spent time in the NICU showed higher rates of PTSD-like symptoms compared to full-term infants who did not require intensive care. These symptoms included heightened startle responses, difficulty with emotional regulation, and problems with attachment.
It’s important to note that while these findings suggest a potential link between NICU experiences and trauma-related symptoms, more research is needed to fully understand the relationship. The complex interplay of medical, environmental, and developmental factors in the NICU makes it challenging to isolate the specific causes of these symptoms.
Recognizing and Addressing Trauma in Infants
Identifying trauma in non-verbal infants requires a keen eye and a deep understanding of infant behavior and development. Behavioral and physiological indicators of infant distress can include changes in sleep patterns, feeding difficulties, excessive crying or irritability, and withdrawal from social interactions. Some infants may also exhibit physical symptoms such as increased heart rate, rapid breathing, or sweating in response to perceived threats.
The importance of early intervention cannot be overstated when it comes to addressing potential trauma in infants. Research has shown that early experiences play a crucial role in shaping brain development and laying the foundation for future mental health. By identifying and addressing trauma-related symptoms early, healthcare providers and caregivers can help mitigate the long-term impacts and promote healthy development.
Trauma-informed care for newborns and NICU babies is an emerging approach that recognizes the potential for early life experiences to impact long-term well-being. This approach emphasizes creating a nurturing environment that minimizes stress and promotes healing. Key elements of trauma-informed care include minimizing painful procedures when possible, promoting skin-to-skin contact with parents, and creating a calm, low-stimulation environment.
Supporting Infant Mental Health and Preventing PTSD
Promoting infant mental health and preventing trauma-related stress begins with recognizing the importance of early bonding and attachment. Skin-to-skin contact, also known as kangaroo care, has been shown to have numerous benefits for both full-term and premature infants. This practice helps regulate an infant’s body temperature, heart rate, and breathing, while also promoting feelings of security and reducing stress.
Minimizing separation between infants and parents is another crucial aspect of supporting infant mental health. When possible, rooming-in arrangements that allow parents to stay with their newborns can help promote bonding and reduce stress for both babies and parents. In cases where separation is necessary due to medical needs, efforts should be made to facilitate frequent visits and involvement in care routines.
Creating a calm and nurturing environment for newborns is essential, particularly in hospital settings. This can involve reducing noise levels, dimming lights during rest periods, and minimizing unnecessary handling or procedures. In the NICU, practices such as clustered care (grouping necessary interventions to allow for longer periods of undisturbed rest) can help reduce stress on fragile infants.
Providing support for parents of traumatized infants is also crucial. Postpartum PTSD: Recognizing and Overcoming Birth Trauma is a reality for many parents, particularly those who have experienced complicated deliveries or have babies in the NICU. Offering counseling, support groups, and education about infant mental health can help parents better understand and respond to their baby’s needs while also addressing their own emotional well-being.
As our understanding of infant mental health continues to evolve, it becomes increasingly clear that the experiences of our earliest days can have profound and lasting impacts. While the concept of PTSD in babies may still be controversial in some circles, the growing body of research suggests that infants are indeed capable of experiencing trauma-related stress responses.
Ongoing research in the field of infant PTSD is crucial to further our understanding of how early life experiences shape long-term mental health outcomes. As we continue to explore this complex topic, it’s essential to approach newborn and NICU care with a trauma-informed perspective, recognizing the potential for both positive and negative impacts on infant development.
By acknowledging the importance of infant mental health and implementing practices that support early bonding, minimize stress, and promote healing, we can work towards ensuring that every child has the best possible start in life. As we move forward, it’s crucial that healthcare providers, researchers, and policymakers continue to prioritize the mental health needs of our youngest and most vulnerable patients, recognizing that the foundations of lifelong well-being are laid in these earliest moments of life.
Source: https://neurolaunch.com/can-babies-have-ptsd-from-birth/

Abstract
Introduction
Premature infants require specialized care, and nurses need to have specific skills and knowledge to provide this care effectively.
Objective
To evaluate the impact of an on-the-job training program on the improvement of nurses’ knowledge and practice related to creation of a healing environment and clustering nursing procedures.
Methods
From January to April 2022, a study utilizing a one-group pre- and post-test design was conducted at NICUs in governmental hospitals. The study participants involved 80 nurses working in these NICUs. Researchers used predesigned questionnaire and checklist practice to collect the data pre and post the intervention.
Results
37.5% of the participants were aged between 25 and less than 30 years, with a mean age of 28.99 ± 7.43 years. Additionally, 73.7% of the nurses were female, with a mean experience of 9.45 ± 3.87 years. Prior to the intervention, the study found that a majority of the nurses (62.4%) demonstrated poor knowledge. However, after the intervention, a significant improvement was observed, with 60.0% of the nurses demonstrated good knowledge. Likewise, prior to the intervention, the study revealed that the majority of the nurses (83.8%) exhibited incompetent practice. However, post-intervention, a substantial improvement was observed, with 81.3% of the nurses demonstrated competent practice.
Conclusion
On-the-job training had significant improvements in nurses’ knowledge and practices regarding applying healing environments and clustering nursing care. On-the-job training is suggested as an adaptable, effective and low-cost technique to train nurses. To maintain the improvement achieved, ongoing instruction, feedback, assessment/reassessment, and monitoring are encouraged.

Abstract: Effective leadership in today’s dynamic environments rests not simply on experience, but on intentional coaching and apprenticeship. This article explores how coaching emerging leaders through structured apprenticeship models foster transferable skills, organizational continuity, and leadership identity. Drawing on scholarly research in leadership education, youth development, and coaching theory, it outlines actionable strategies for embedding coaching-as-apprenticeship within professional settings. Case studies and frameworks highlight how critical reflection, mentor guided practice, and identity formation synergize to elevate both individual and organizational performance.
Closing teaser: If you are ready to transform your leadership legacy by raising apprentices, not just subordinates, read on to discover how to build, guide, and sustain the next generation of leaders
Introduction: The Leadership Gap and the Coaching Imperative Organizations often struggle with leadership continuity, not because of a shortage of talent, but due to the lack of developmental pathways for emerging leaders. Traditional training is often episodic, outcome-focused, and disconnected from real-world work. In contrast, apprenticeship-style coaching integrates on-the-job practice, guided reflection, and mentor scaffolding, offering a more durable model for leadership development. This approach recognizes that leadership is not merely a set of competencies, but a mindset and identity forged over time. The urgency to shift from transactional leadership development to transformational apprenticeship-based coaching is underscored by the increasing volatility of organizational environments, where agile and empathetic leadership is critical. Coaching emerging leaders through apprenticeship enables them to learn by doing, internalize the organization’s values, and develop the confidence necessary to lead effectively in complex situations.
Coaching Young Leaders: Foundations and Key Benefits:
Research increasingly supports the idea that coaching has a disproportionate impact when targeted at younger or less experienced leaders. Not only do these individuals exhibit higher growth trajectories in leadership identity and self-efficacy, but they also tend to show increased engagement and retention. Coaching becomes a vehicle for establishing positive habits, fostering psychological safety, and creating alignment with core organizational values at the earliest stages of one’s leadership journey. Coaching supports the holistic development of young leaders, improving both their technical capabilities and their emotional intelligence. Moreover, when coaching is introduced early, it becomes embedded in their leadership DNA, making them more likely to coach others in the future. This creates a ripple effect of development, where coaching becomes not just a practice but a cultural norm. Organizations that invest in coaching young talent are investing in a long-term, sustainable leadership pipeline.
Apprenticeship as a Leadership Model:
Unlike ad hoc mentorship, apprenticeships are structured to emulate expert-apprentice learning paradigms found in fields such as medicine or skilled trades. These involve a deliberate, phased progression: observation, participation, leadership with supervision, and finally autonomous execution. Apprenticeships in leadership also emphasize the social construction of leadership identity. Through cycles of feedback and reflective inquiry, the emerging leader gradually integrates personal values with professional expectations. This model positions leadership as an evolving identity, not a static role. Apprenticeship also enables learning from lived experience rather than abstract instruction, reinforcing the importance of real-world exposure, feedback loops, and relationship based development. It fosters humility in the coach and curiosity in the apprentice, setting the stage for deep trust and mutual growth. Apprenticeships elevate leadership development from sporadic training to an intentional journey of transformation.
Shared and Super-Leadership: Enabling Young Leaders:
Shared leadership refers to distributing leadership responsibilities across roles rather than concentrating them in a single position. When younger leaders are empowered to co-lead projects, they not only gain experience but also receive validation as future in-fluences. This approach builds confidence, fosters innovation, and enhances team collaboration. Super-leadership, defined by the ability to help others lead themselves, offers another powerful coaching mindset. Rather than creating dependents, leaders cultivate autonomy, encouraging apprentices to develop their own leadership identities and decision-making capabilities. Super leaders invest in unlocking the potential within others by fostering critical thinking, self-direction, and ownership. These frameworks challenge traditional hierarchical models, favoring instead a collaborative environment where every team member is seen as capable of contributing leadership value. By doing so, organizations not only enhance their leadership capabilities but also foster cultures of empowerment and resilience.
Designing a Coaching-Apprenticeship Program:
Building a coaching-apprenticeship program begins with intentional matching; coaches should be trained not only in their disciplines but also in delivering feedback and reflective questioning. Programs should incorporate a phased structure with clear goals per stage, shadowing opportunities, and assigned leadership responsibilities. Embedding reflection points, journaling, peer discussions, or coach debriefs, creates a feedback-rich environment that accelerates development and reinforces critical thinking. Designing such a program also entails aligning the apprenticeship with the organization’s strategy. What leadership behaviors and mindsets are most critical for your future? These should be embedded in coaching conversations, project assignments, and developmental goals. Regular check-ins, performance reviews, and cross-functional exposure can enhance the apprentice’s understanding of broader business operations. Moreover, integrating the program into HR and L&D systems ensures sustainability, scalability, and accountability.
Case Examples & Research Evidence:
Data from academic institutions and corporations demonstrate measurable improvements in leadership capability, confidence, and identity when coaching and apprenticeship programs are implemented in tandem. One study found that undergraduates who received leadership coaching outperformed their peers in self-evaluation, initiative-taking, and communication. Similarly, organizations that pair junior executives with seasoned leaders on real-world projects report greater succession readiness and improved cultural continuity. For instance, a healthcare system implemented a year-long leadership apprenticeship for high-potential clinical managers, resulting in a 25% increase in internal promotions and significantly reduced turnover. These examples underscore the power of experiential learning and the trust it fosters between generations. The most impactful programs are those that strike a balance between structure and flexibility, allowing apprentices to stretch while remaining supported. The case for apprenticeship is not just anecdotal; it is data-driven and results-proven.
Overcoming Challenges in Coaching Apprentices:
Leaders struggle to find time for coaching or mistakenly default to giving directives. An effective apprenticeship requires a shift in mindset: from command to inquiry, from short-term results to long-term development. Another challenge is the temptation to clone oneself—coaches must resist imposing their exact styles. Instead, they should encourage apprentices to explore and refine their voices, emphasizing authenticity and self-discovery over replication. Leaders must also learn to relinquish control, allowing apprentices to make mistakes, learn, and recover. For the apprentice, imposter syndrome and fear of failure can hinder growth, coaches must be adept at building psychological safety and modeling vulnerability. Lastly, organizational structures must support this effort; when performance metrics favor only short-term outcomes, coaching can be deprioritized. Addressing these challenges requires intention, effective communication, and a commitment across all leadership levels.
Measuring Success and Institutionalizing the Practice:
To sustain apprenticeship models, organizations must define clear metrics of success and integrate coaching into their leadership pipelines. Effective metrics include observable behavior changes, feedback from peers and supervisors, and progression into formal leadership roles. Making coaching part of job expectations, and distributing time in calendars and budgets, signals organizational commitment and reinforces its strategic value. Institutionalizing the practice also requires training and support for coaches. Not everyone is naturally equipped to coach; it must be seen as a skill to be developed. Recognition and reward systems can further encourage participation and excellence. Over time, the goal is to normalize coaching-as-apprenticeship as a cultural standard, not a temporary initiative. When embedded deeply, it becomes self-perpetuating: today’s apprentices become tomorrow’s coaches.
Action Plan – Six-Month Coaching Apprenticeship Template: Month Activity
1. Identify apprentice and coach pair; set mutual goals. Clarify expectations and agree on communication rhythm.
2. Shadowing senior leader in meetings, decision-making, and interpersonal scenarios. Focus on observation and questioning.
¾. Apprentice leads small initiatives or portions of projects under supervision. Provide real-time feedback and adjust tasks as needed.
5. Deep reflection session: discussing key learnings, identify growth areas, and recalibrate developmental objectives.
6. Final project debrief: summarize progress, co-create a personal leadership vision statement, and develop a transition roadmap.
This plan is not a rigid template but a guide for phased development. Each month’s focus allows for a gradual transition from observation to ownership. Coaches facilitate experiences while ensuring support and reflection. By the end of six months, apprentices should not only demonstrate enhanced skills but also articulate a personal leadership philosophy shaped by feedback and experience.
Conclusion:
Coaching young leaders through an apprenticeship approach creates multiplier effects, developing not only leadership skills but also leadership identity, confidence, and organizational continuity. This shifting paradigm, from managing tasks to growing people, challenges leaders to measure legacy by who they raise, not just what they achieve. Investing in apprenticeship coaching today helps ensure stronger, more adaptive organizations tomorrow. By embracing apprenticeship as a strategic imperative, leaders cultivate a lasting impact, one that extends far beyond their tenure and
shapes the trajectory of future generations.
More importantly, the coaching-as-apprenticeship model restores a human-centric ethos to leadership development. It recognizes the power of relationships, trust, and long-term investment in others. It transforms organizations into learning communities, where leaders are not only accountable for business outcomes but also for building capacity in others. The impact ripples outward, from individual apprentices to teams, departments, and entire institutions.
Every seasoned leader has the opportunity —and the responsibility —to create space for others to grow. Leadership, at its best, is not a destination but a legacy to be passed down. Moreover, that legacy is measured not only in profit margins and productivity metrics, but in the readiness, values, and courage of those who follow. Coaching future leaders as apprentices ensures that the mission and values we lead with today endure and evolve through those we mentor tomorrow.
Challenge question: As a leader, are you merely managing today’s results, or are you actively shaping tomorrow’s leaders through intentional apprenticeship?
Source:https://neonatologytoday.net/newsletters/nt-jul25.pdf

INNOVATIONS

Health care challenges have long stood in the way of Liberia’s national development. With limited access to quality medical services, many Liberians have found themselves traveling abroad or relying on prayer and hope in the face of serious illness.
But a new chapter is unfolding, one driven by local leadership, global standards, and a bold commitment to change.
Located along the Congo Town back road, WPMC delivers safe, customer-centered, world-class services, all provided by Liberian professionals. Its offerings range from advanced laboratory diagnostics to outpatient care and medical screenings for international visa applicants.
Metering system installation services.
WPMC’s practices are in line with national and international standards and are supported by technologies sourced from the U.S., Europe, and Asia. From the outset, the center has been designed to restore trust in Liberia’s medical system.
The official launch ceremony brought together distinguished guests, including former President Ellen Johnson Sirleaf, health sector leaders, staff, and the general public. The event not only marked a major milestone in health care delivery but also celebrated the vision and leadership that made it possible.
At the heart of WPMC is Dr. Nicole Cooper, the facility’s Medical Director. A passionate health leader, who shared the journey that led to the creation of the center.
“I’ve seen too many people praying outside hospital rooms, hoping that everything aligns just to save a life,” she said. “Too many are forced to leave the country for basic health care because they don’t trust that it can be done here.”
That reality, Dr. Cooper explained, planted a seed back in 2009, the early inspiration behind what would eventually become Wellness Partners. In 2021, she returned to Liberia with the goal of building a system that met international standards but remained accessible and reliable for all Liberians.
She began with Wellness Partners Clinic, a small pilot that tested health care delivery models, affordability, and customer care strategies. From those humble beginnings, the initiative expanded into the full-fledged Wellness Partners Medical Center.
“We’re different,” she said. “We invest in our people, prioritize quality and safety, and put transparency at the center of what we do.”
“Our vision is bold yet simple: to become the safest, most reliable, and most convenient network of medical care in Africa,” she told attendees. “This is what’s possible when we believe in ourselves and build from the inside out.”
Representing the WPMC Board of Directors, Mrs. Monique Cooper Liverpool echoed that sentiment, calling the center “a homegrown solution led by Liberian talent with world-class expertise.”
Also speaking at the event was Mrs. Sophie Parwon, CEO of Benson Hospital, who highlighted the growing contribution of the private sector in Liberia’s health care ecosystem.
“While the government remains the main provider of health services, the private sector is increasingly stepping up, contributing to service delivery, financing, innovation, and capacity building,” she said.
Mrs. Parwon praised Dr. Cooper as a “public health icon” and called on government and development partners to strengthen support for private health initiatives that align with national priorities.
As WPMC opens its doors, it does more than offer medical services. It offers hope, hope for a health care system where Liberians no longer need to look abroad for basic care, where dignity and quality go hand in hand, and where innovation is driven from within.
Source:https://thenewdawnliberia.com/a-homegrown-medical-facility-emerges/
Abstract
Objective To assess the feasibility and clinical utility of daytime polysomnography (PSG) in infants ❤ months of age.
Methods A prospective observational study of a convenience cohort analysing PSGs that were conducted for clinical purposes in infants less ❤ months of age, between 1 May 2021 and 31 May 2024. A comparison was made between results for daytime PSG in the neonatal intensive care unit (NICU) and overnight PSG in the sleep laboratory. The type of PSG performed (daytime vs overnight) was based on the workflow of the sleep laboratory. Primary outcomes were successfully completed PSGs (feasibility) and per cent sleep efficiency (clinical utility). Secondary outcomes compared other sleep parameters between groups. Patient and public feedback directly informed the development of the research question and outcome measures.
Results Of 60 PSGs, 28 were daytime and 32 were overnight. Daytime studies had a younger age (median 18 vs 55 days, p<0.001) and shorter median recording time (8.2 vs 10.4 hours, p<0.001). All daytime PSGs were successful, indicating feasibility. After adjusting for age at PSG and total recording time, per cent sleep efficiency was equivalent in the two groups (95% CI −12.4 to 5.7; p 0.456), indicating their clinical utility. For secondary outcomes, daytime PSGs had a higher % rapid eye movement (REM) sleep by 9.9% points (95% CI 1.1 to 18.8; p 0.028) compared with overnight PSG. Parameters that were not different included: frequency of spontaneous arousals, REM latency, sleep latency, Apnoea-Hypopnoea Index and Obstructive Apnoea-Hypopnoea Index. A decline in requests for overnight PSGs and a corresponding increase in daytime PSGs over the course of the study were observed.
Conclusion Daytime PSGs performed in NICU were feasible and provided clinically useful results in infants ❤ months of age. Availability of daytime PSGs performed at the infant’s bedside expands resource capacity and has the potential for cost savings.
Source: https://bmjpaedsopen.bmj.com/content/9/1/e003641
With support from the World Health Organization (WHO), the National Public Health Institute of Liberia (NPHIL) and the Ministry of Health concluded a residential hands-on in-country training on genomic sequencing and bioinformatics at the National Public Health Reference Laboratory (NPHRL) from 29 September to 19 October 2024 in Margibi County. Facilitated by a team of experts from the Noguchi Memorial Institute for Medical Research in Ghana, a total of 10 national laboratory technicians received a 2-week intensive training followed by a 1-week practice session.
Genomic surveillance plays a critical role in tracking emerging pathogen variants. It has become a fundamental global public health tool for detecting, monitoring, and responding to infectious disease outbreaks, as demonstrated by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic. During the in-country training, national laboratory scientists analyzed additional mpox-positive samples and detected another mpox strain, clade IIb.
“Before the training, we were reliant on international laboratories to identify the circulating pathogen strains. Now, we have the capability to conduct sequencing and bioinformatics analysis in-country, enabling us to rapidly identify emerging pathogens and their geographic origins,” Francis Omega Somah, laboratory technologist at the National Reference Laboratory in Liberia.
This training is a significant milestone in the integration of pathogen genomics and bioinformatics into public health surveillance, outbreak detection, and investigation, which will enhance disease control and prevention efforts in Liberia. “This is a game-changer for the country as we will now have the national capacity to sequence and characterize pathogens of epidemic prone diseases in our country. We thank WHO for this strategic investment and their continuous technical and financial support towards strengthening Liberia’s capacity to detect and manage epidemics,” said Dr Dougbeh Nyan, Director General of NPHIL.
In 2022, WHO published a global genomic surveillance strategy to support countries in expanding their capacities. Unfortunately, 50% of Member States, including Liberia, lacked domestic sequencing capacity. To address this gap, WHO, under the AFRO HERA project, is supporting six African nations: Liberia, Burundi, the Central African Republic, Comoros, Eritrea, and Togo to establish and strengthen genomic sequencing and bioinformatics capacity, thereby expanding detection and genomic surveillance of epidemic-prone priority pathogens across the African Region. WHO has significantly invested on the continent in infectious disease and genomics surveillance.
“The most important aspect of capacity building is training the right experts. When a country has skilled professionals with the right platform, expertise, and infrastructure, they can respond swiftly and effectively to public health emergencies,” said Dr. Coulibaly Sheik, WHO AFRO Lead Diagnostic and Laboratory Services Unit.
Dr. Peter Clement, WHO Country Representative, thanked the team of facilitators and WHO AFRO for supporting Liberia through the EU-funded project which will strengthen the country’s laboratory systems. “By empowering local experts with the skills to conduct genomic sequencing and bioinformatics analysis, we are ensuring that Liberia is better prepared to rapidly identify emerging threats and implement timely interventions,” said Dr. Peter Clement, WHO Liberia Representative.
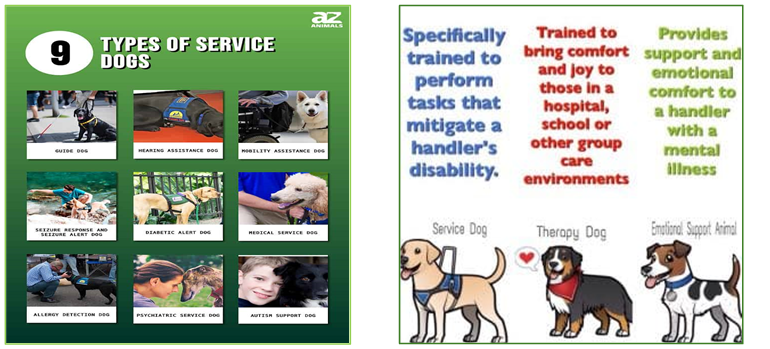

The Healing Power of Comfort Pets in Children’s Hospitals
In the high-stakes environment of a children’s hospital, every source of comfort matters. Beyond the dedicated medical staff and cutting-edge technology, one often overlooked hero is the comfort or service pet. These animals, specially trained to provide emotional support, offer more than companionship—they bring a sense of calm, joy, and connection during some of the most challenging times in a young patient’s life.
For pediatric patients, comfort pets can help reduce anxiety, ease feelings of isolation, and even promote healing. A gentle nuzzle or playful paw can break through the walls of fear that sometimes build during hospital stays. Studies have shown that interaction with therapy animals can lower stress hormones, improve mood, and provide a sense of routine and normalcy for children who are often navigating complex medical treatments. In the neonatal context, while the infants themselves may not directly interact with pets, families of NICU babies experience the calming presence of therapy animals, helping them manage stress, fear, and the emotional weight of having a critically ill newborn.
Families may benefit greatly from the presence of comfort pets. Parents and siblings frequently carry their own anxieties as they support a hospitalized child. In the NICU, where the emotional toll is heightened by uncertainty and intensive care routines, therapy animals offer brief but meaningful moments of relief, allowing families to smile, laugh, and connect. These moments can strengthen the parent-child bond, provide emotional grounding, and even support parents’ ability to be present and engaged in their baby’s care.
Healthcare workers often report the positive impact of comfort pets. Long shifts, high emotional demands, and the intensity of neonatal and pediatric critical care can take a toll on staff well-being. Therapy animals provide a moment of grounding and a reminder of the simple joys in life, helping to reduce burnout and improve morale.
In NICUs and pediatric wards alike, the presence of a comfort pet is a win-win: patients receive care enriched by joy, families feel supported, and staff experience a boost in their own emotional resilience.
Our very own Bennie Boo (hypoallergenic, gentle, and loving) may be a perfect candidate for comfort care training in his future. This is a pathway we may consider next year when he turns two.





Anthony gets a lesson from Liberia’s first ever surfer, Alfred Lomax. He doesn’t catch a wave, but locals manage to catch more than enough fish for a fresh seafood feast, served with a beer, of course!

