Sierra Leone, officially the Republic of Sierra Leone, is a country on the southwest coast of West Africa. It is bordered to the southeast by Liberia and by Guinea to the north. Sierra Leone’s land area is 73,252 km2 (28,283 sq mi). It has a tropical climate and environments ranging from savannas to rainforests. As of the 2023 census, Sierra Leone has a population of 8,460,512. Freetown is its capital and largest city.
Sierra Leone is a presidential republic, with a unicameral parliament and a directly elected president. It is a secular state. Its constitution provides for the separation of state and religion and freedom of conscience. Muslims constitute three-quarters of the population, and there is a significant Christian minority. Notably, religious tolerance is very high.
Available healthcare and health status in Sierra Leone is rated very poorly. Globally, infant and maternal mortality rates remain among the highest. The major causes of illness within the country are preventable with modern technology and medical advances. Most deaths within the country are attributed to nutritional deficiencies, lack of access to clean water, pneumonia, diarrheal diseases, anemia, malaria, tuberculosis and HIV/AIDS.
Healthcare in Sierra Leone is generally charged for and is provided by a mixture of government, private and non-governmental organizations (NGOs). There are over 100 NGOs operating in the health care sector in Sierra Leone. The Ministry of Health and Sanitation is responsible for organizing health care and after the end of the civil war the ministry changed to a decentralized structure of health provision to try to increase its coverage.
Source: https://en.wikipedia.org/wiki/Sierra_Leone
- GLOBAL PRETERM BIRTH RATES – Sierra Leone
- Estimated # of preterm births: 10 per 100 live births/Global Average:
- Source- WHO Preterm Birth Rate (Per 100 Live Births)
- WHO Prematurity
- World Population Review
- WHO Country Consultation of Low and Preterm Birth Weight
- http://chartsbin.com/view/34987
- https://www.mamaye.org/resources/scorecards/mamaye-factsheet-preterm-birth-sierra-leone-2015.html

COMMUNITY
Margaret Yainkain Mansaray Becomes First Sierra Leonean to compete in the Africa Prize for Engineering Innovation
Posted on December 1, 2022 by Design in Design Innovation

Sierra Leonean Innovator and CEO of Women in Energy-SL Margaret Yainkain Mansaray became the first Sierra Leonean to be listed among Innovators competing for the Africa Prize for Engineering Innovation 2023. An award organized annually by the Royal Academy of Engineering UK (The United Kingdom’s national academy of engineering).
Mansaray, who is the only female rising to compete against 14 other innovators from ten countries across Africa was recognized for her invention of a Smart Green Stove. The smart green stove is a fast and efficient non-electric cooking device she designed to reduce greenhouse gas emissions and health risks that greatly affect women and girls in Africa.
The stove burns briquettes made from recycled local materials such as coconut and jelly shells which are usually discarded. The insulator absorbs most of the heat and makes the stove nearly smokeless, reducing the harmful soot which would otherwise be released into the environment.
“My team and I are working tirelessly to uplift women and girls by addressing time and energy poverty. I’ve always been the only woman in a room full of men, and so one of my aims is to educate women and girls, specifically on the role engineering can play in improving their lives.”, Mansaray said.
The Africa Prize for Engineering Innovation was launched in 2014 by the Royal Academy of Engineering. An award for ambitious African innovators creating local and scalable solutions to pan-African and international challenges. The innovations shortlisted in 2023 tackle challenges approaching the UN’s Sustainable Development Goals, including clean water and sanitation, sustainable cities and communities, clean energy, good health and well-being, and quality education.
According to the Royal Academy of Engineering, Innovators shortlisted for the Africa Prize will benefit from a special package of support including business incubation, mentoring, fundraising and communications. The package will also include access to the Academy’s global network of high-profile and highly experienced engineers and business experts in the UK and Africa. Four finalists will be chosen to direct their innovations and business plans to Africa Prize judges at an event in Accra, Ghana, on July 6th, 2023. The winner will have a take-home of £25,000, and three runners-up will win £10,000 each. An additional One-to-Watch award of £5,000 will be given to the most promising entrepreneur from the remaining shortlist.
Mansaray took to her Facebook handle and expressed her joy as she took pride in being that this is the first time Sierra Leone has been shortlisted for the Royal Academy Africa prize. She emphasized that her achievement is a win for the country and especially for vulnerable girls and women.
“I am happy to share that for the first time Sierra Leone has been shortlisted in the Royal academy Africa prize and I am the only female among 10 African countries.”, Mansaray wrote.

Papi J – Waterloo Waterloo
🎧 | 2025 SIERRA LEONE MUSIC 🇸🇱 | Music Sparks
The song “Waterloo” is amazing! We discovered it through a promotion by Jakey Jake and instantly fell in love. This talented artist, known as Papi J, deserves to be signed to a record label. In this song, Papi J describes his hometown, Waterloo—a place known for its cassava bread, fried fish, and hardworking community.


Long, yet concise and comprehensive, this article is abundant in its research, collaboration, big-picture perspective, and applicability. Well worth the read!
Recommendations of the Iberoamerican Society of Neonatology (SIBEN®) for “Transdisciplinary and Humanized care for the Newborn and the Family”: XIV SIBEN CLINICAL CONSENSUS (English Version)
Jorge Pleitez Navarrete, MD, Carmen Dávila-Aliaga, MD, Lordes Lemus-Varela, MD, María Teresa Montes Bueno MT, Cristian Muñoz, MD, Augusto Sola, MD, Sergio Golombek, MD, and participants of the XIV SIBEN Clinical Consensus of the Iberoamerican Society of Neonatology (SIBEN)

Abstract: A cultural change in Iberoamerican neonatal hospitalization units is imperative to guarantee respect for the rights of newborns and their families during hospitalization, with equity at different levels of care, without differences based on geographic areas or socioeconomic level. It is essential to train and improve the competencies of the health team, from managers to healthcare professionals, to provide transdisciplinary and humanized care (CTH) for newborns and their families. There is sufficient evidence that CTH positively impacts the outcomes of newborns and their families when their families are involved in the care of their hospitalized babies.
This paper summarizes the results of the XIV SIBEN® Clinical Consensus on “Transdisciplinary and humanized care for newborns and their families,” in which 50 SIBEN® members, neonatologists, and nursing graduates from 14 Iberoamerican countries actively participated during 2023, before, during and after the face-to-face meeting held in Mar de Plata, Argentina in November 2023. This article answers questions based on the best available evidence and describes recommendations of clinical significance for truly providing transdisciplinary and humanized care (CTH).
Introduction:
In the 19th century, infant deaths were considered part of the natural order 1. In 1802, the first pediatric hospital, L’Hôpital des Enfants Malades, was founded in Paris, which promoted breastfeeding and the emotional needs of children.
Neonatology emerged in the 20th century owing to technological advances that increased neonatal survival but with reduced parental involvement. Research, such as the “Citizens’ Committee for Children of New York City” and the “Platt Report” in the United Kingdom, influenced the acceptance of parental presence in hospitals, demonstrating that their presence did not increase infection rates. Spitz coined the term “hospitalism” to describe the adverse effects of prolonged hospital confinement . In the 1980s, the family-centered model of neonatal care was introduced, demonstrating its effectiveness in caring for premature infants.
In 1984, the European Parliament approved the Charter of Patients’ Rights. In 1986, it adopted the European Charter for Hospitalized Children, which recognized 23 rights, including the right to be accompanied by their parents or primary caregivers for as long as possible. This charter was adopted by international organizations such as the WHO and UNICEF. Western countries began to ease visitation restrictions on parents as early as 1990.
Not all neonatology units in Ibero-America had adequate conditions to implement CTH by 2016. A study by the Ibero-American Society of Neonatology (SIBEN®) revealed that 63% of the units offered space for mothers to stay with their infants (27% overnight), and in 60% of cases, there were time restrictions for parental visits. This demonstrates the need for a cultural change in Ibero-American NICUs to guarantee respect for the rights of neonates and their families during hospitalization.
Concept and principles of transdisciplinary humanized care (CTH) for newborns and families
In recent years, different denominations have incorporated families into the care of hospitalized newborns. We consider that this care is provided by many disciplines to the newborn (NB) and its family in an integrated, simultaneous, non-hierarchical, organized manner, according to the needs of the newborn and, above all, in a humanized way; therefore, SIBEN calls this model of care “Transdisciplinary Humanized Care (CTH) for the newborn and its family.”
With a comprehensive approach, the CTH for the NB and its family emphasizes family participation, respect for their needs, and transparent communication . These interventions reduce neonatal stress, favor their development, reinforce the family’s caregiver role, and improve family bonding and quality of care.
The fundamental principles of CTH are respect, honoring families’ diversity, flexibility, exchange of information, no medical terminology, participation and decision-making, collaboration between the patient, family, and health care providers, and family empowerment to discover their strengths.
Levels of Intervention of CTH for the Newborn and Family :
• First level: Support parents through psychoeducational, communication, and environmental interventions to help them cope with hospitalization and prepare them for the newborn’s follow-up.
• Second level: Interventions provided by the parents focused on improving the development and recovery of the newborn, with psychological and physical benefits for parents who received education from the clinical team.
• Third level: Collaborative care models, where parents are fully involved in newborn care.
Elements of CTH (12)
According to the currently available scientific evidence, we agree with the following elements:
• Recognition of the family as an important and indispensable part of the care of hospitalized neonates
• Constant participation of the family in decision-making, as well as the procedures carried out
• Facilitate family/professional collaboration at all levels of care.
• Communication and exchange of information by health personnel at all times with the family.
• Recognition of family diversity, including ethnicity, socioeconomic, educational, racial, geographic,
etc., thus avoiding value judgments.
• Incorporate models that contribute to parents’ learning regarding the care of their children through courses and educational programs.
• Unrestricted access at all times and the family can always be involved in the care of their child
• Creation of family support networks.
• Recognize the family’s strengths, feelings, emotions, concerns, and ability to help and contribute,thus validating them as an important, fundamental, and indispensable part of the NB’s care.
• Facilitate the parents’ stay as much as possible by providing a comfortable space for them to be close to their child for as long as possible.
In 2011, the book Neonatal Care, Discovering the Life of a Sick Newborn by Sola, A introduces and emphasizes the concept that: “parents are not visitors” and that there should not be limited hours for a mother to be with her baby who is in the neonatal intensive care unit (NICU).
Changes, benefits, and tools for performing CTH:
* promote the newborn’s neurological and physical development
* humanize care
* reduce stress
* improve health
* improve adherence to treatment
* facilitate breastfeeding
* optimize discharge care and transition to home care
* increase the quality of care
* increase parental satisfaction
The following are some essential strategies to achieve this objective:
1. Information and awareness-raising: Promote the benefits of BFHC through programs aimed at medical teams, families, and public policymakers.
2. Staff training: Implementation of workshops, courses, and internships to train staff in CTH.
3. Involve parents from the beginning: Encourage their presence and participation in medical procedures and daily care to strengthen bonding.
4. Empower parents: Provide them with tools and training so that they can actively participate in making decisions about their babies’ health.
5. Adapt physical spaces: Design areas that allow parents to stay close to their children.
6. Ongoing emotional support: Offer psychological support programs to help families manage stress and emotional difficulties.
7. Planning and evaluation: Ensure gradual implementation with constant adjustments and collaboration of professionals, parents, and the community to achieve more humane and effective care.
Some tools to promote parental involvement in neonatal care include:
a) Welcome Kit: This kit contains educational information on neonatal care, educational resources,and guidance for parental involvement.
b) Skin-to-skin contact: improves thermal stability, facilitates breastfeeding, and reduces stress in parents and infants (7,18)
c) Care diary: Parents record the baby’s daily activities, such as feeding, diaper changes, and procedures, which allows them to feel more engaged in their care and evaluate their progress as caregivers.
d) Medical rounds participation program: Parents can discuss the baby’s condition and treatment, ask questions, and express concerns.
e) Training classes and workshops: Educational resources on neonatal care and child development are provided.
f) Mobile applications and online platforms: Allow parents to access up-to-date information on their baby’s condition, schedule visits, and communicate with medical staff.
g) Support groups and counseling: Facilitate mutual support among parents, share experiences, and get involved in their child’s care.
Difficulties or obstacles in the CTH process:
Including the family in the care of the hospitalized neonate is a humanized and recommended practice, although it is not always implemented in all neonatal units. Some professionals consider that the presence of parents is not necessary, arguing that they may generate anxiety, not be prepared for invasive procedures, or that the physical space is insufficient. In addition, lack of knowledge about family-centered care and institutional regulatory barriers negatively affect the care of the infant and family.
Skin to skin contact: Skin-to-skin contact (SSC) has ancestral origins in different cultures and times, and it is a common practice between mothers and their healthy or sick babies. In protocolized form, it began in the 1970s in Bogota, Colombia; the maternal body heat allowed it to stabilize physiologically and provide comfort and security to neonates. Since 1990, the success of this practice has spread, and it has been adopted in several countries as a neonatal care option.
SSC is beneficial for both term and preterm newborns, and it is applied immediately after delivery, during the first hour of postnatal life, during hospitalization, and even at home. It is associated with decreased maternal postpartum depressive symptoms, improved perspective on motherhood, and intrinsic and extrinsic gratification, especially being able to care for her baby. Lower maternal salivary cortisol levels have been reported at one week and one month postpartum.
In addition, recent studies have shown a significant prolongation of breastfeeding at six months (5.08 months vs. 2.05 months). Other findings highlight additional benefits, such as increased weight gain of the NB, reduction of hospitalization time, strengthening of the mother-child bond, and contribution to the overall development of the NB.
CTH and the advantages of breastfeeding
CTH includes the concept of 24-hour “open-door units” where fathers are encouraged to be present during breastfeeding and participate in feeding, either directly from the breast or by expressed milk. This approach promotes bonding, analgesia, neurodevelopment, milk production, and breastfeeding.
CTH and family satisfaction:
Parents of hospitalized NBs may experience acute or posttraumatic stress, affecting their physical, psychological, and social health, as well as their relationship with their children. Parents’ confidence increases when they know how to act and the impact of their actions on their infant’s health.
When CTHs are established, the family is recognized as a permanent reference in the child’s life, even during hospitalization. Family members become involved in the care, take an early part in it, and participate in decision-making regarding their child, promoting the parent-child bond .
The most important dimensions of neonatal care for parents are safety, care, communication,information, education, environment, monitoring, pain management, and participation .
SIBEN® recommends:
1. Change the paradigm and improve the communication skills of healthcare personnel to meet the family’s needs regarding the illness, treatment, and recovery of the neonate.
2. Encourage empathy, accessibility, and confidentiality in communication with families, increasing their participation in decisions about care and treatment. In addition, family functioning is considered to be crucial support during the newborn’s hospitalization.
3. Apply CTH from the admission of the newborn, integrating the family as active and competent caregivers of their child.
Family satisfaction helps in dealing with grief.
The NICU neonatal health team focuses on preserving the newborn’s life through therapeutic interventions . When parents face the loss of an infant, the grief they experience requires compassionate accompaniment by multidisciplinary teams that pay attention to psychological, emotional, and spiritual aspects of the family and offer empathy and respect for the parents to mitigate their pain .
Infrastructure to Implement CTH for the Newborn and Family
The World Health Organization (WHO) recommendation of 24-hour parental presence in the NICU has motivated the construction of neonatal units with private rooms, encouraging these indications. The implementation and use of private rooms in the NICU as a recommendation dates back to approximately 1990.
Impact and Advantages of private rooms for the newborn.
• Reduction of infections. Decreases the spread of nosocomial infections and makes the isolation of patients colonized by potentially pathogenic microorganisms possible.
• Increased weight gain. Preterm infants who remained in private rooms with their parents in the short term had a higher rate of weight gain during hospitalization.
• Less pain, with fewer procedures and lower pain scores in infants in private rooms compared to infants in shared rooms.
• Better neurobehavioral outcomes. Infants in private rooms had significantly less physiological stress, hypertonicity, and lethargy.
• Lower noise levels. In the shared NICU model, 20 decibels were found to be 20 decibels higher.
• Fewer days of hospitalization. More infants were discharged early.
• Increased breastfeeding. 90% achieved breastfeeding in private rooms compared to only 66% is shared.
• Fewer episodes of apnea. In the group stratified on the PEMR (Physician’s Estimate of Mortality Risk) scale, there was a 57% decrease in total apnea events in preterm infants.
• Reduction in direct cost.
• Reduction in illumination. Neonates admitted in open and private NICU rooms at Sanford Children’s Hospital in Sioux Falls, USA, were compared, and a reduction in illumination was shown: 48.4 lux and only 6.4 lux in private rooms (p < 0.05), with longer sleep time in neonates.
• Post-discharge: fewer consultations and hospitalizations. Comparing two groups of preterm infants it was found that they had lower rates of rehospitalization and requests for medical care at discharge.
• Higher cognitive scores. At an 18-month follow-up, Bayley III cognitive language and motor scores were compared in private and shared rooms in preterm infants under 30 weeks of gestational age. Infants with high maternal involvement in both NICUs had improved cognitive scores.
Disadvantages and risks of private rooms
The optimal types and frequencies of stimulation for very preterm brain development are unknown. Still, the isolation of these infants in relatively dark and quiet private rooms may be going in the wrong direction. However, auditory stimulation, such as parental voices, is considered positive in the NICU environment, being associated with better motor and language outcomes. Therefore, the need for greater parental permanence and involvement in the single-family room is emphasized, as otherwise, this aspect may be considered a disadvantage.
NICU nurses are at greater risk of fatigue, anxiety, and depression than nurses in general wards. Burnout in neonatal nurses continues to be a problem.
Is family presence during neonatal resuscitation or other invasive procedures advisable? ANSWER: YES. Parents or family members should be welcome to be present during an inpatient procedure and should not be asked to leave the room if they wish to be there.
SIBEN® Position. There is no scientific evidence to justify separating parents from critically ill NBs or those requiring advanced cardiopulmonary resuscitation. On the contrary, numerous studies report the beneficial effects on the parents, family, and even their approach concerning the care received. They always respect the parents’ decision to participate and are accompanied by health personnel who explain the situation and what they are seeing.
It is advisable, after the presence of the parents during the resuscitation, to carry out a joint analysis with their presence, to provide feedback to explain the procedures performed, to clarify their doubts, and also to consider their observations and concerns to improve the quality of the procedures performed in our units.
A philosophical concept to be taken into account is the following, which establishes a position in this regard: “Thus, from Anthropology, it can be noted that throughout the history of mankind, women have sought assistance at the time of childbirth, while the rest of mammals do it alone. It is considered that this is due to the complexity implied by the bipedestation, the pelvic cavity, and the human cephalic perimeter.”
Recommendations to implement transdisciplinary care in Neonatal Units:
• The importance of names: the name of the NB and his/ her parents. Knowing and referring to the mother, father, and newborn by name is essential. Never call or refer to the newborn as: “the baby in incubator number such and such”.
The art of communication. The importance of listening and making yourself understood.
Use simple and straightforward language to ensure that what has been expressed has been understood, especially when listening to the family’s concerns and encouraging them to ask questions and express emotions. Respect the family’s cultural and religious beliefs and customs.
We are part of the same team—”Parents Are Not Visitors” The importance of encouraging, facilitating, and accompanying the participation of the mother and family. Encourage skin-to-skin contact.
We should also consider the participation of the newborn’s brothers or sisters, grandfathers and grandmothers, or other designated persons, with the authorization of their mothers and/or fathers.
Interpreting beyond words. The importance of feelings and mental health support. Health care professionals should identify situations where the mother expresses fatigue, anguish, hopelessness, sadness, frustration, depression, crying, etc.
They are not alone. The importance of the peer support network and parent associations (such as FAMISIBEN)
In 2021, SIBEN®, with the FAMISIBEN working group, drafted recommendations for parents of neonates in the NICU. These recommendations are available in digital format on its website, https://sites.google.com/siben.net/famisiben/, free of charge for family members, caregivers, health professionals, and the general public.
Common questions for implementing CTH in the NICU:
- Should the pacifier be banned? Answer: NO. Why? Non-nutritive sucking (NNS) is an integral part of infant developmental physiology. Based on the available evidence, the “SIBEN Mini Clinical Consensus / 2021” authors recommend initiating stimulation with a pacifier (NNS) at 28-29 weeks gestational age. Centers that “prohibit or forbid” the use of pacifiers, teats, or whatever it is referred to should review this restriction and know that this is not baby-friendly but quite the opposite.
- Should the mother be made to feel welcome for 1440 minutes each day? Answer: YES “Parents are not visitors.” CTH for the family promotes stress reduction for the parents and a more positive relationship between the parents and the newborn.
- Can the mother stay 24 hours a day in the hospital where the NICU is located? Answer: YES. We should encourage the mother or father to stay close to the baby even in the NICU; mothers and fathers in single family nurseries care more for their baby, including skin-to-skin contact compared to mothers in the open NICU, improving infant growth and neurodevelopmental outcomes.
- d. Is there a minimum or maximum length of stay for at least one parent in the NICU? Answer: NO. There is evidence that the separation of hospitalized patients alters the dynamics of parental care and affects all family group members.
- e. Will the family member (mother, father, or whoever the mother indicates) be able to participate in NICU care? Answer: YES. Family involvement is a key element in all infants’ physical, cognitive and psychosocial development, including those in the NICU.
- f. What are the benefits of performing a blood sampling, vaccine placement, peripheral vein cannulation, or other pain-generating procedure with the infant nestled, held, and sucking? The SIBEN® Clinical Consensus on the diagnostic and therapeutic approach to pain and stress in the newborn recommends non-nutritive sucking when performing procedures that cause mild to moderate pain. Breastfeeding is considered the first choice treatment because of its safety, ease of administration, and availability, in addition to its multiple benefits, which have been extensively studied both nutritionally and immunologically.
- What is the role of the “schools for parents” in the CTH for the newborn and the family? The schools are a training space for parents whose roles are as follows:
1. To allow conscious and active participation of parents in neonatal care.
2. Teach parents about the child’s physiological states, biorhythms, and adaptation mechanisms.
3. To offer knowledge for post-discharge care of the newborn.
4. To instruct on the benefits of breastfeeding and newborn feeding.
5. To teach and promote skin-to-skin contact.
6. Teach parents about hygiene, care, and medication administration.
7. To teach warning signs, infection prevention, and infant cardiopulmonary resuscitation.
8. Provide tools to work on psychomotor development stimulation, forms of stimulation, and
expected emotions of the newborn in different circumstances to ensure adequate growth and
development of children.
h. What key actions are indispensable and essential for CTH to exist?
1. First and foremost, a paradigm shift is necessary, associated with a theoretical/practical
educational plan for all personnel, providing them with specific tools and skills to promote
change.
2. Achieving the multidisciplinary participation of all neonatology staff without dissonant or
opposing voices (“everyone cooperates”).
3. It must be recognized that discussing this type of neonatal care is not enough since
implementing CTH in action requires facing and overcoming many challenges in different areas.
4. Modify the environment: It is essential to have areas, offices, and spaces for private conversations
with parents and family.
5. Partnering with health care administrators and financiers in the task
i. In the NICU of an institution certified as “mother and child friendly,” is CTH practiced for the care of the newborn and its family? In many NICUs, even in many hospitals certified as “mother friendly”, mothers are still separated from their babies, and there is little or no space for mothers, and a chair or bed is not always provided next to the newborn’s incubator.
Key points from SIBEN® about CTHs in the NICU:
• The brain’s structural plasticity is in response to maternal auditory stimulation.
• The quality of experience significantly influences the brain and the function and structure of the
developing central nervous system
• The presence of the family in neonatal care has beneficial effects, including improved bonding of
the NB with the family and improved quality of care.
• It should be emphasized that “parents are not visitors.”
• Smooth transition from the hospital environment to the home: no rush and no pressure. Ideally,
this occurs during pre-hospitalization, especially in prolonged hospitalizations of more than three
weeks.
• Setting concrete, everyday actions and deeds (not just words or documents) into practice, such as
those discussed in this manuscript, is very useful in achieving the best results.
• Periodically carry out critical and continuous self-evaluation of the neonatal team.
Source: https://neonatologytoday.net/newsletters/nt-apr25.pdf

International cooperation and solidarity are essential in tackling global challenges, including efforts to ensure the effective realization of the right to health for all nations.
As proclaimed by the United Nations, promoting international cooperation and solidarity is a duty of States.
In this context, we express our profound appreciation, gratitude, and recognition to Cuban health professionals who have provided—and continue to provide—their services in multiple nations.
Since 2019, and with even greater intensity now, a dishonest campaign has been unleashed to discredit Cuba’s international medical cooperation, exert pressure on recipient governments, and deprive populations of essential healthcare services.
No one with a basic sense of honesty can doubt that this is an attack on multilateralism, a manipulation for political purposes, and a continuation of aggression and hostility against Cuba.
Access to healthcare is a human right, and millions of people cannot be deprived of this inalienable right for political reasons.
Attempts to delegitimize Cuban medical cooperation overlook the fact that the shortage of health professionals is a pressing issue worldwide, whose solution demands greater international cooperation and solidarity, not unfounded attacks.
Cuba has devoted considerable efforts and resources to health care and today has one of the highest ratios of doctors per capita in the world, enabling it to make a significant contribution to global health.
Cuban international medical cooperation has made it possible to provide high-quality health care to millions of people around the world.
Over the past 60 years, more than 605,000 Cuban health collaborators have completed missions in 165 nations.
Their feats are notable in the fight against Ebola in Africa, blindness in Latin America and the Caribbean, cholera in Haiti, and the COVID-19 pandemic. Numerous brigades from the Cuban International Contingent of Doctors Specialized in Disasters and Major Epidemics ‘Henry Reeve’ have carried out humanitarian work in many nations.
Cuban professionals and technicians participating in these programs do so exclusively upon the express request of the concerned countries, offering their expertise and services freely and voluntarily.
Many of them work in remote rural areas to save lives, even at the risk of losing their own. They provide care to all patients without distinction, refraining from getting involved in internal political affairs and strictly respecting the laws and customs of the countries where they work.
Additionally, Cuba has provided free medical training to 43,000 healthcare professionals from 120 nations. In numerous countries, medical faculties have been established with Cuban professors.
It is imperative to defend and recognize the valuable contributions of thousands of Cuban health professionals who, through immense personal sacrifice, continue to offer their cooperation.
Neither discrediting campaigns nor the devastating effects of the intensified economic, commercial, and financial blockade have succeeded in preventing Cuba from continuing to save lives and share its limited resources with other nations in need.
Cuban medical cooperation will remain a symbol of hope, dedication, humanity, and solidarity.
(Cubaminrex-Permanent Mission of Cuba in Geneva)
***The Non-Aligned Movement is a forum of 120 countries that are not formally aligned with or against any major power bloc, and dedicated to representing the interests and aspirations of developing countries. It was established in 1961.

HEALTHCARE PARTNERS

ProgenyHealth Releases 2025 Key Trends and Insights Report on Maternal & Infant Health
ProgenyHealth Jan 15, 2025
Report identifies 7 of the most pressing industry trends that will shape the months and years ahead
ProgenyHealth, LLC, a recognized national leader in Maternity and NICU Care Management, today announced the release of its 2025 key trends and insights report, “Steep Challenges & Uneven Progress.” This year’s highly anticipated annual report identifies critical areas within maternal and infant health to watch in the year ahead, for health plans, hospitals, and healthcare providers.
The state of maternal and infant health in America remains precarious. By now, the sobering data has become all too familiar – The United States’ mortality rate is the highest of all high-income nations. Tragically, as many as 80% of maternal deaths, many of which occur in the first 42 days after giving birth, are preventable.
“While many challenges exist, there is continued hope on the horizon, as an increasing volume of healthcare-focused experts strategize to turn this situation around—and as new trends emerge to offer fresh opportunities and solutions,” said Linda Genen, Chief Medical Officer, ProgenyHealth. “These shifts promise to upend the present state of maternal and infant health, setting the nation on a new and better path forward.”
Key findings and predictions of the 2025 trends report include:
- Maternal Decision-Making Will Take Center Stage. The concept of self-determination in the birthing process is being taken more seriously by medical institutions that are piloting programs to create dedicated care teams to listen to, work with and support those going through the birthing process. Research continues to show that providing women with a more empowered birthing experience pays dividends down the road.
- Neonatology Will Continue to Advance the Viability of Micro Preemies. Until recently, very few infants born before 26 weeks were likely to survive. Today, many infants born as early as 22 weeks are not only surviving but thriving due to medical advancements. These extraordinary advancements have entirely improved the outlook for those born too young and too early.
- Payers Will Increase Focus on Postpartum Support for Women. Between 2017 and 2019, nearly 30% of pregnancy-related deaths happened in the six weeks to 12 months after women gave birth, CDC data shows. Notably, many of these deaths were tied directly to mental health issues, which tend to go both undetected and untreated in the postpartum period. It is estimated that 50% of all postpartum depression cases go undiagnosed.
- Amid Rising Costs, Employers Will Demand Alternatives to Standard Insurance Products. Since total birth costs are one of the top cost categories for health coverage, employers will likely begin to focus on proactive managed care partnerships to provide additional support during this complex period.
- Increased Birth Anomalies Will Require More Complex Care. Congenital anomalies are among the chief causes of infant mortality, and as births increase across the nation—particularly in states with reproductive health restrictions in place—these anomalies are expected to climb. Children born with such anomalies may require surgical intervention, ongoing physical or occupational therapy, long-term educational support, or an array of assistive devices—needs that may evolve and last for life.
- Whole Genome Sequencing Will Become a Game-Changer for Newborn Care. Rapid Whole Genome Sequencing (rWGS) testing for newborns may soon address this widespread genetic disorder blind spots. This genetic test can be used to identify and diagnose numerous conditions, including developmental delays, seizure disorders, conditions that affect hearing, vision, and immune deficiencies. rWGS is faster and more accurate than other genetic testing and considers a person’s full DNA sequence. While rWGS remains unavailable to many families, that situation is likely to change in the years ahead.
- The Rate of Home Births Will Keep Rising – as Will Insurers’ Potential Role in Covering Them. Given the growing number of home births, some states are now exploring ways in which supporting this birth choice—and making it safer and more routinized, with intervention available in case of emergency—may help to combat certain aspects of the maternal health crisis


Newborn Health Resources: Trainings and Tools for Improving Newborn Health in Humanitarian Settings

In 2018, the Global Health Cluster lead by the World Health Organization (WHO) conducted a capacity survey of Global Health Cluster partners to capture information on partners’ self-assessment of their technical, operational, and coordination capacities. The results showed that most international and national partners reported a lack of capacity and expertise to provide maternal and newborn health (MNH) services. Less than half reported an ability to provide Basic Emergency Obstetric and Neonatal Care (BEmONC) and Comprehensive Emergency Obstetric and Neonatal Care (CEmONC) at primary and secondary level respectively, and only 42% of the international partners and 50% of the national partners reported providing Essential Newborn Care (ENC).
To accelerate newborn health services in humanitarian settings, recent global interagency efforts have led to the development of the 2018 Inter-Agency Working Group on Reproductive Health in Crises (IAWG)-endorsed Newborn Health in Humanitarian Settings: Field Guide (NBFG); the Newborn Care Supply Kits for Humanitarian Settings; and a Roadmap to Accelerate Progress for Newborn Heath in Humanitarian Settings: 2020–2024.
In addition, these resource cards were developed to facilitate capacity building of humanitarian stakeholders. To build these cards, a consultant conducted a mapping of key maternal and newborn health trainings across the development and humanitarian sectors using a methodology that included a desk review of existing trainings, stakeholder interviews, and a short online survey delivered to Health Cluster Coordinators. The findings of the mapping exercise were presented and discussed at an experts meeting organized by Laerdal Global Health, Maternity Foundation, and Save the Children in Stavanger, Norway in 2019.
Overall, the mapping identified a great variety of existing training programs, mainly for clinical health care providers, on all aspects of newborn care and at all levels of care provision. Existing trainings for program managers were somewhat scarce, and access to available tools and guidelines could be improved.
Thus, we have packaged these resource tools as a quick pocket reference to aid program managers and implementers in humanitarian and fragile settings with identifying and accessing the most relevant trainings, tools, implementation guidance, and clinical guidance

Rethinking Platelet and Plasma Transfusion Strategies for Neonates: Evidence, Guidelines, and Unanswered Questions
Rozeta Sokou, Eleni A. Gounari, Alexandra Lianou, Andreas G. Tsantes, Daniele Piovani,,Stefanos Bonovas , Nicoletta Iacovidou, Argirios E. Tsantes
Abstract
The transfusion of platelets and fresh frozen plasma (FFP) to critically ill neonates in neonatal intensive care units (NICUs) is a common intervention, yet it is still widely performed without adhering to international guidelines. The guidance itself on the therapeutic management of neonatal coagulation disorders is generally limited due to the absence of strong indications for treatment and is mainly aimed at the prevention of major hemorrhagic events such as intraventricular hemorrhage (IVH) in premature neonates. Historically, the underrepresentation of neonates in clinical studies related to transfusion medicine had led to significant gaps in our knowledge regarding the best transfusion practices in this vulnerable group and to a wide variability in policies among different neonatal units, often based on local experience or guidance designed for older children or adults, and possibly increasing the risk of inappropriate or ineffective interventions. Platelet transfusion and, particularly, FFP administration have been linked to potentially fatal complications in neonates and thus any decision needs to be carefully balanced and requires a thorough consideration of multiple factors in the neonatal population. Despite recent advances toward more restrictive practices, platelet and FFP transfusions are still subject to wide variability in practices.
This review examines the existing literature on platelet and FFP transfusions and on the management of massive hemorrhage in neonates, provides a summary of evidence-based guidelines on these topics, and highlights current developments and areas for ongoing and future research with the aim of improving clinical practices.
Source:https://www.thieme-connect.com/products/ejournals/abstract/10.1055/a-2601-9364

PREEMIE FAMILY PARTNERS

- Understanding Preterm Development: How It Helps With Bonding
- Bonding with Your Premature Baby in the NICU
- Make Bonding Moments with Your Preemie at the NICU
Connecting with your premature infant in the Neonatal Intensive Care Unit (NICU) may seem overwhelming and complicated. It can be a unique and challenging experience since it involves the emotional well-being of the parents and the development of the baby.
However, with the proper knowledge, resources, and support, bonding with your preemie may be a lovely and joyful experience. With the appropriate guidance and techniques, these may foster a closer relationship with your infant in its new surroundings.
Every baby and every situation is unique. Be patient with yourself and your baby as you navigate the NICU. Understand preemies’ distinct needs and the most significant ways to help them. This article will delve into everything you need to know about bonding with your premature baby in the NICU.
Understanding Preterm Development: How It Helps With Bonding
Preterm and full-term newborns have a developmental trajectory, even if preterm babies grow at a different rate. Premature infants, or preemies, as they’re fondly called, have a distinct development.
A clear understanding of preterm development is critical to the bonding process between parents and their preemies—a great way to get closer to your baby. You can still establish a connection with your preemie while in the NICU by being aware of their developmental milestones.
Parents must understand their unique requirements and developmental stages to effectively care for and support them. Some of these characteristics include:
Small Body, Thin and Delicate Skin
Overall, premature babies have significantly low birth weight; hence, their physical size is relatively small. Additionally, they have thin and delicate skin. These unique features require special care in handling and bathing them.
Sensitivity to Touch
Premature babies learn about the world mainly through touch. More importantly, a sense of touch is the key for parents to bond with them. However, they’re more sensitive to touch than full-term babies, so providing a gentle and comforting touch is critical.
Vulnerability to Overstimulation
Light and noise are two stimuli that easily overwhelm premature babies. It’s best to create a calm and quiet environment that makes them feel more secure and facilitates bonding.
Delayed Bone and Muscle Development
As advised by medical experts, involve your premature infant in gentle exercises and motions to help support their development and create opportunities for bonding.
Premature babies may have delayed physical development, including muscle and bone development. Late preterm babies, born between 34 and 36 weeks, may have fully developed organs but still have changes happening in their brains.
Premature babies born earlier than 28 weeks and babies born with an extremely low birth weight of less than 1 kg have the highest chance of developing problems.
Potential for Neurodevelopmental Challenges
Premature babies may experience long-term effects on their cognitive and neurological development, including learning disabilities, attention-deficit/hyperactivity disorder (ADHD), and difficulties with executive functioning.
Parents must be aware of these developmental challenges; hence, bonding and interaction with their baby should consider these disabilities.
Needs Specialized Care
Premature babies in the NICU require specialized medical care, which makes it challenging for parents to bond with them. However, being involved in their care, such as participating in diaper changes or helping with feeding, can still contribute to their bonding success.
Potential for Longer Hospital Stays
Premature babies need to stay in the hospital for an extended period, which can be emotionally challenging for parents. Finding ways to stay connected and involved with their care can help maintain the bond during this time.
Understanding these unique characteristics helps parents bond with their premature babies. By being aware of their baby’s needs and sensitivities, parents can provide a comforting and supportive environment that promotes bonding and development.
Bonding with Your Premature Baby in the NICU
Managing the difficulties and uncertainties of having a preemie could be complex. You need to focus on developing a strong bond, even while in the NICU. By prioritizing this bond, you provide your baby with love and encouragement despite hardship.
Maintaining a deep bond with your baby through care and engagement is essential for their development and general well-being throughout their stay in the NICU. Premature infants who receive loving care are more likely to experience favorable developmental outcomes.
Remember that every baby and family’s situation is unique, so it’s important to tailor your approach based on the specific needs and guidelines provided by the NICU staff
There are many ways to develop a bond with your baby. Here are some tips to consider:
1. Spend quality time.
Find time to visit your baby regularly at the NICU and make the most of the time you have together. Even if your baby is sleeping or connected to monitors, your presence creates a sense of familiarity and constant support.
Your presence alone provides a long-term positive impact on your baby’s development and gives you confidence as a parent too. Spending time with your baby is such an important part of bonding in the NICU.
2. Learn your baby’s cues.
With your regular visits to your preemie, you take time to learn your baby’s cues. Get involved in their care, especially on how to make your baby comfortable at all times. You may ask the NICU staff for guidance on how to interact with your baby.
3. Kangaroo care.
Also known as skin-to-skin contact, kangaroo care is highly encouraged and affords numerous benefits to premature babies. This involves holding the baby against your bare chest with only a diaper on for an extended period.
Hold your baby against your chest so they can hear your heart beating. For a premature baby, such moments are crucial for physical and emotional bonding.
This skin-to-skin contact helps regulate the baby’s temperature, heart rate, and oxygen levels, promotes breastfeeding and breathing, and reduces stress for both the parent and baby. It also promotes weight gain and digestion. All these benefits foster bonding with your preemie.
4. Gentle touch.
Premature babies are sensitive to touch due to their underdeveloped nervous system. Use a light and gentle touch to stroke your baby’s skin, hands, and feet. This tactile stimulation helps promote relaxation and bonding—a soothing effect that helps establish a connection with the parent.
These comforting touches provide reassurance and make the baby feel loved and secure. Your care team will guide you to feel comfortable while touching your baby. They will guide you in specific ways that your baby will be looking for and can tolerate.
Some NICU infants can be held right away, while others may need an alternative approach. Once their condition is stable, massage can also help them relax. They will feel calm, cared for, and supported. You could hold your baby’s hand or stroke their head, for example.
5. Talk, sing, and read.
Premature babies benefit from hearing their parent’s voices. Even though they may seem too small to understand or respond to, talking, singing, and reading softly to them create a sense of familiarity and connection. It helps them recognize and connect with your voice, promoting bonding.
Engage in gentle conversation and sing lullabies. Your voice will become familiar to them, providing a sense of security. Your baby recognizes your voice from when they were inside the womb, so hearing it can be comforting and soothing—a source of bonding during the NICU stay.
6. Help with care tasks.
Discuss with the NICU staff if you could participate in your baby’s care routine as much as possible. Changing diapers, feeding if permitted, and bathing your baby enhance your bonding experience and help you feel more connected with your little one.
Other simple tasks could just be providing comfort through swaddling and positioning. These activities help establish a sense of parental responsibility that promotes bonding.
7. Create a sense of normalcy.
Despite a highly medicalized environment, try to create a sense of normalcy by personalizing the baby’s space. You can bring familiar items, such as a blanket or a small toy, to make the surroundings feel more like home.
8. Leave your scent.
Check with NICU staff to learn what cloth items are appropriate to place in your baby’s space. Sleep with that item or wear it all day tucked under your clothing, then place it in your baby’s space. In this way, you’re establishing a connection with your baby through your scent.
Sweet premature baby in an incubator with oxygen and unrecognizable mom caressing baby trying to calm him down
9. Take care of yourself.
Prioritize self-care during this challenging time, taking care of your physical and emotional well-being during this stressful period. Have a balanced diet, get enough rest, and engage in activities that give you joy and relaxation.
When you’re calm and well-rested, it positively impacts your interactions and connection with your baby.
10. Seek emotional support.
The NICU experience can be emotionally overwhelming and exhausting, especially for moms. It’s essential to seek support from your partner. Also, from healthcare professionals, therapists, family, friends, and support groups specific to parents of premature babies.
Sharing experiences and emotions can help cope with the challenges and strengthen the bond during this critical period. They can provide comfort, understanding, and guidance, which are essential for maintaining a healthy emotional state during this challenging time.
11. Seek support from NICU staff.
Ask the medical staff for guidance and support on ways to bond with your premature baby. They have experience working with families in similar situations and can offer valuable advice and resources.
12. Ask questions.
Don’t hesitate to ask questions or seek clarification from the medical team regarding your baby’s condition, progress, and care plan. Being well-informed helps alleviate anxiety and empowers you to initiate more meaningful interactions with your baby.
13. Celebrate milestones.
Premature babies often reach developmental milestones later than full-term babies. Celebrate each small achievement, such as gaining weight, moving to an open crib, or starting to breastfeed.
These milestones testify to your baby’s progress and strengthen the bond between you and your little one. Maintaining a positive outlook can help strengthen your bond and offer hope during the NICU journey.
Make Bonding Moments with Your Preemie at the NICU
Nothing is as unique as a parent’s and baby’s bond, despite the challenges. Even in the NICU, you can create lasting memories and form a connection that will grow as your baby grows. Understand your baby’s growth and foster a happy atmosphere with your preemie.
Bonding happens over time, and it’s built on everyday moments like smiling at your baby, touching them, using loving words, and responding to their needs. With the strategies outlined in this article, determine which technique works best for you and your baby.
While every baby is different, you may try various approaches. Enjoy every bonding moment. Your preterm baby may be physically small, but they’re strong and have a lifetime of love and opportunity ahead of them.
Source:https://www.omegapediatrics.com/bonding-your-premature-baby-in-the-nicu/

Our twin pregnancy
In late 2021, I was pregnant with twins, 2 little siblings for my son Rico. The pregnancy was very exciting, and we couldn’t wait to meet them. We wanted to do a gender reveal, but sadly we didn’t get the opportunity.
At 21 weeks, I had a scan which found that my cervix was open. I had to have an emergency cerclage on New Year’s Eve 2021, and was in hospital for 2 weeks.
A week after being sent home, my waters broke. I was 24 weeks pregnant at this point and very scared. I rushed back to hospital where they told me I would remain until the twins were born.
Giving birth
10 days later, after multiple scans, I went into labour. My beautiful twins were born at 25 + 6 weeks at 2:03am (Luna) and 2:36am (Luca).
Both babies were transferred to NICU to begin their fight.
At 4 days old, suddenly and unexpectedly, our baby boy Luca died. We had to wait 6 months for his postmortem results to find out why, which is when we were told he’d died of NEC. Our survivor Luna spent 87 days in NICU before coming home.
How I coped
The early days of grief I just shut myself away from people. I was at the hospital everyday with Luna and I just engrossed myself in caring for her. I had bereavement therapy which didn’t really help me, but what did help immensely was PTSD therapy.
I’ve also used the Facebook community to reach out to other people who have been through similar situations. I’ve made friends through those communities and we regularly message and support each other when things get tough.
Honouring Luca
We miss Luca every day. Having a surviving twin is such a complex mix of emotions – we feel happy and sad at the same time. We honour Luca daily and include him in our family.
We have a garden for him at home and in my parent’s garden. I also wear jewellery to remind me of him, and have lots of little ornaments around the house in his memory. On the twin’s birthday, we had a cake for both of them (pink and blue).
Every year, I try to do something for charity in his name. Last year I raised over a £1000 in a swimming challenge and this year I took part in Tommy’s Walk for Hope and managed to raise £400.
Advice for others
My advice to anyone who loses a twin baby would be:
Embrace the feelings of happiness and sadness. Losing a baby is something that no one should have to go through, but you’re a twin parent and your survivor will always be a twin.
Reach out to support through charities, and take counselling if you can. You will probably be suffering from some form of PTSD and working through that really helped me.

Led by trained PSI facilitators, our online NICU group is intended for parents of babies who are currently or formerly in the NICU. This peer support group is for those with babies up to two years old who experienced a NICU stay for any reason. Connecting with others who have experienced the uniquely stressful environment of a NICU will provide parents with understanding, as well as helpful tools and resources. Whether your baby is currently in the NICU or you have finally returned home, our NICU Postpartum Parents support group is here for you.
Note: This group is not for people processing the details and trauma of pregnancy and/or infant loss. Please join one of our Loss and Grief Support Groups for this important support.
PSI Support Groups
All of our groups are FREE and virtual. When registering for Sharewell for the first time, skip the unlimited offer on the payment page.
What to Expect
Our groups are 90 minutes (1.5 hours) in length. The first ~30 minutes is spent providing information, education, and establishing group guidelines. The next ~60 minutes is “talk time,” in which group members share and talk with each other. Group members must be present for the group guidelines before joining in the discussion or “talk time.”
Student and clinical observations are not allowed in our group spaces due to confidentiality and creating a safe space.
- Cameras are required during introductions for the safety of all group members. Please make sure your technology allows you to turn on your camera at least briefly for this portion of the session.
- The session will take place via Zoom (from the ShareWell website), so make sure your device is compatible with the Zoom app. This may require updating or downloading the Zoom app.
Student and clinical observations are not allowed in our group spaces due to confidentiality and creating a safe space.
Registration Information
PSI Support Groups are hosted on ShareWell and are split into different “wells.” Click on the registration link above to go to the Well, which includes support groups in each category.
When signing up for groups and making an account:
- Skip the unlimited offer on the payment page (all of our groups are free!)
- Access PSI support groups in each dedicated community
- Reach out to groups@postpartum.net if you have any questions
In this new platform, we will no longer have a waitlist function. **We will allow up to 16 group members to enter the group, so please arrive on time to get a spot. Once we reach 16 members OR we have started talk time, the group space will be closed.
Source:https://postpartum.net/group/nicu-postpartum-parents/

Sick or premature babies: tips for family and friends

Key points
- Parents of sick or premature babies have a lot of stress in the early months of their babies’ lives.
- Practical help and emotional support from friends and family can help parents cope.
- It’s good to ask parents exactly how you can help.
Supporting parents of sick or premature babies
Parents of sick or premature babies go through a lot of emotional ups and downs in the early weeks and months of their babies’ lives.
When they get practical help and emotional support from family and friends, parents often cope a lot better with the experience. And when they’re managing well, they’re better able to look after their babies.
Here’s how you can help
- Celebrate as you usually would when a baby is born
Offer congratulations, send a card or flowers, and ring the new parents. By celebrating the birth of their baby in this way, you’re helping them celebrate as well. Give a gift if this is what you’d usually do. Small gifts for the parents can help them feel nurtured too.
If you’re thinking of giving clothes for the baby, make sure they’re very easy to put on and take off – loose necklines and armholes are good. If the baby is premature, size 00000 clothes can also be useful, because many parents won’t have bought these smaller sizes. Baby clothes for later are wonderful too, because they help the parents think about the future, when their child is at home.
Another gift could be a voucher for hospital parking. Or you could give a voucher for a restaurant close to the hospital, so that parents can have a meal and some time together but not be far from their baby.
You might be able to contribute to or help the parents organise cultural or religious traditions or ceremonies to celebrate their baby’s birth.
2. Offer practical help
Parents will be visiting the hospital as often and for as long as they can for days, weeks or months to come. This means that everyday chores are hard to fit in or don’t get done, which can be stressful.
Here are helpful things you could offer to do:
- Mow the lawn or walk the dog.
- Prepare meals or do the weekly grocery shopping.
- Take older siblings to preschool or school or look after the other children in the evening.
- Give parents a lift to the hospital – parking and transport can be very expensive.
- Set up a messaging group or social media page, so that parents can send updates to just one source.
3. Support parents in whatever way they need
It’s OK to ask parents what they need. Some parents want to shut themselves off and cope with the situation alone or with a few close friends and family. Respect their wishes, but also let them know that you’re thinking of them. You could try to offer help when they seem ready.
Some parents need a lot of people around for support. These parents might love having company at the hospital. You could offer to drive, have lunch or just sit with them. Some parents want to talk about things other than the baby. Parents’ needs can change as their baby grows and changes.
4. Stay in touch with parents
A text message, an email, a quick phone call or voice message, or even an old-fashioned card in the mail – these are simple ways to let parents know you’re thinking of them. They help parents feel supported and remembered.
Try to understand how stressed the parents are and avoid judging them if they forget a birthday, can’t get to a family gathering, or take less interest in what’s happening in your life. It’s not that they don’t care – it’s just that right now, all their energy and focus is on their baby.
5. Say positive things about the baby
You can show your support by saying positive things like ‘Your baby is growing fast already’, or ‘They’re strong just like you’.
Avoid talking about setbacks that might happen or challenges that the baby could face, unless the parents bring it up with you. Also avoid giving advice about the baby.
6. Don’t expect to cuddle the baby
Sick or premature babies are very sensitive to touch, noise, infection and other things in their environment, so cuddling or touching is often limited or not allowed. Parents can also be very protective of their babies.
You might not even be able to see the baby, because there are usually limits on the number of visitors allowed at one time. Often it’s only 2 visitors. Sometimes only family is allowed – often this is only the baby’s parents. Each hospital has its own set of rules. Instead, you could ask to see photos of the baby (if the parent feels up to sharing them) or have a coffee with the parents at the hospital café.
Don’t be surprised if you still can’t have a good cuddle when the baby goes home. Many babies are still easily overwhelmed and might need to be protected from too much handling and too many new people.
If you’re sick, it’s important to avoid visiting a family with a baby in the neonatal intensive care unit (NICU) or the special care nursery. Sick or premature babies can get illnesses and infections very easily.
7. Listen to parents
Parents are likely to have mixed and strong feelings about their sick or premature baby and their experiences of the birth or hospital. These might not surface for weeks, months or even years.
Be open, let them talk and avoid giving advice unless it’s asked for. Avoid comparing them with other parents who’ve had a hard time. If you listen more than talk and follow the lead of the baby’s parents, you’re more likely to be helpful.
8. Keep offering help after the baby comes home
Parents might be tied to the house for some weeks once the baby comes home. Having someone organise shopping or preschool and school runs can really help.
Premature babies, or “preemies,” are born before 37 weeks gestation.
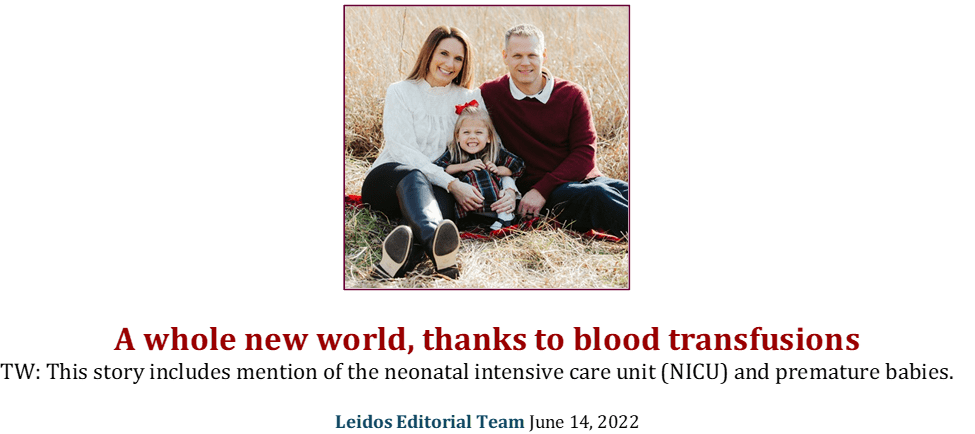
Hailey Petersburg was born at 24 weeks and five days.
Considered a “micro-preemie” and weighing just one pound and seven ounces, Hailey had a 40% chance of survival and a long road ahead of her in the Neonatal Intensive Care Unit (NICU). She spent 133 days in the NICU, where she underwent multiple surgeries and was treated for anaemia of prematurity. “Every day was a rollercoaster,” said Hailey’s mother and Leidos Data Scientist Allison Petersburg. “She was in a critical stage where her condition changed so rapidly every day.”
Before Hailey even reached what would have been full-term at 40 weeks, she received almost two dozen transfusions, which were crucial to her treatment plan.
Hailey’s tiny body was working as hard as it could, often enduring bradycardic events where her heart was beating too slow. Her medical team provided blood and platelet transfusions to help carry oxygen throughout her body; their impact was immediate, improving Hailey’s health and significantly increasing her vital signs.
In the United States, someone is in need of blood or platelets every two seconds. For many months, Hailey was one of those people. She received blood or platelet transfusions almost daily in the first weeks of her life, decreasing over time as she grew stronger each day. “Throughout the NICU experience of being in day-to-day survival mode, the gift of blood was a vital stability for Hailey,” said Allison.
Blood and platelets can’t be manufactured and must be donated. They also have an expiration date, so there is always a need for more blood donors. Since the beginning of the COVID-19 pandemic, the American Red Cross has seen a decline in blood donations, resulting in a national blood crisis. Between blood, platelets, and plasma, “nearly 16 million blood components are transfused each year in the United States.”
“Whenever Hailey had a transfusion, she would immediately begin breathing better, her heart rate was stable. As she received blood, the bradycardic and oxygen desaturation events decreased and all her vital signs improved,” said Allison. “They were lifesaving.”
After almost four and a half months in the hospital, Hailey Petersburg was ready to go home. Fast forward five years, and now Hailey is a recent preschool graduate, who, according to her mother, “is doing absolutely amazing.”
She’s an active soccer player, swimmer, and dancer, as well as an avid Disney princess fan, currently infatuated with Jasmine from Aladdin. Allison thinks Hailey intuitively knows how hard she had to fight soon after she was born, citing her joie de vivre, “she’s just the happiest little girl.”
Hailey is an example of why it’s so imperative to donate blood if you’re able. With nearly 30,000 units of blood needed each day, the Red Cross is continually in need of donors and one pint of blood can save up to three lives.
Even during a global pandemic, Leidos remained committed to diminishing the national blood crisis, collecting more than 311 units over the past two years. Since 2016, we’ve hosted 23 blood drives at our Global Headquarters in Reston, VA, thanks to 674 donors. Other offices, including our Columbia, MD, and San Diego, CA, locations regularly host blood drives, as well as one of our subsidiaries, QTC. The Columbia Leidos office has collected 125 units of blood since 2017.
Not only is donating blood so important, but the process is very quick, only taking about 20 minutes for the physical donation. For perspective, if just 1% more of all Americans donated, blood shortages “would disappear for the foreseeable future.”
“It was clear that the donated blood Hailey received in her transfusions saved her life,” said Allison. “I don’t know if my daughter would be with us today if not for blood donors.”
Schedule an appointment to donate blood today – and save a life.
Source: https://www.leidos.com/insights/whole-new-world-thanks-blood-transfusions
INNOVATIONS


The still predominant siloed, vertical structure of academia, health care systems, funding institutions/mechanisms, and public health organizations around the world pose an important challenge to tackle complex societal and health challenges for people, animals, and ecosystems. Understanding and acknowledging the delicate interdependence between ecosystem, human, and animal health is needed to design and implement comprehensive and holistic health strategies, beyond just human health. Infectious diseases with a zoonotic component have caused widespread human suffering in recent decades, with increased interactions between human and animal populations making people ever more vulnerable to new infections, given the rapidly and constantly changing global ecosystem. Additionally, socio-cultural, political, and economic factors impact the ability of systems to better prevent, detect, and respond to public health challenges at the human, animal, and environmental interface. This complex landscape applies to non-communicable diseases as well, requiring multisectoral approaches well beyond the traditional, narrow biomedical model. Hence, a wholesale shift is needed in how we approach public health. Instead of equating public health only with human health, we need to recognize what it truly is: the inter-related health of the world’s people, animals, and the environments we all share.
The complete interdependence between human, animal, and ecosystem health has been long recognized within Indigenous communities; however, the emergence and rapid expansion of the fields and practice of both One Health (OH) and Planetary Health (PLH) are recent developments in the right direction [1]. While the OH approach has been advocated for mostly in the context of addressing global threats related to zoonotic diseases and antimicrobial resistance, this approach is also relevant for several major public health challenges including pollution management, the environmental/agricultural component of food safety, food security, and nutrition. For example, the OH approach may lead to ecologically sustainable dietary patterns impacting the prevention and management of chronic conditions, such as cardiovascular disease.
The OH/PLH approaches have experienced considerable growth and expansion in academia, and within governmental and non-governmental organizations (NGOs)—with greater traction occurring in the past decade . While OH and PLH are highly complementary approaches based on transdisciplinary, multisectoral, and system-based approaches to health, challenges remain when translating ideas into policy and practice. “Overall, One Health and Planetary Health provide an opportunity to build a stronger research community to collectively address pressing public and global health issues in a truly integrated way”.
In March 2023, the Quadripartite organizations: the Food and Agriculture Organization of the United Nations (FAO), United Nations Environment Programme (UNEP), World Health Organization (WHO), and World Organisation for Animal Health (WOAH), issued an unprecedented call for enhanced global action to use the OH approach to “achieve together what no one sector can achieve alone”, emphasizing the need to translate the OH approach into policy action. Additionally, the Quadripartite institutions, in December 2023, published the One Health Joint Plan of Action with recommendations to implement OH approaches at national levels. Similar movements are occurring within the PLH space. For example, a National Planetary Health Action Plan (NPHAP) is being developed in Malaysia “to mainstream planetary health in all national policies and plans through a holistic and whole-of-nation approach”. Having endorsements from national and international organizations are important; however, there are still elements lacking when considering the implementation of OH/PLH to ensure human, animal, and ecosystem health.
What is next? Local community leadership and involvement is needed to build upon progress to date at the global level. To tackle complex public health challenges, a “bottom-up” approach is needed that complements global and national efforts. An emphasis on local, practical, and feasible solutions are also needed to address complex problems, while engaging local stakeholders and affected communities. A key aspect, however, of implementing OH and PLH approaches into public health strategies is to account for the socio-cultural, religious, and economic factors among local and rural communities. This is especially important when working with those most marginalized, such as Indigenous and rural communities, who are often already closely and directly attached to having strong connections with the ecosystem they inhabit.
Scientific, biomedical, and health knowledge is necessary, but not sufficient alone. Successful public health interventions that work at the human-animal-ecosystem interface require the broad and committed collaboration of members from all levels of society. A coordinated, multisectoral approach that involves animal health and public health authorities, health practitioners, physicians, veterinarians, environmental workers, politicians, researchers, experts in social, cultural, and communication issues, as well as economists, farming and agricultural groups, and local communities is necessary. Importantly, bold and courageous political leadership is essential to co-lead while securing public support for health policy decisions and implementation [5]. It is key to develop a OH/PLH “business case” (e.g. cost-benefit analysis), with governments enabling, facilitating, and supporting implementation processes both financially and within appropriate legal frameworks. This will ensure the recognition for not only the importance of economic benefits derived from reducing a specific health issue, but also for assessing the broader public health and societal benefits and impacts.
While OH and PLH offer a rational systems approach for safeguarding health in an interconnected world, to secure its benefits, public health must do what humans, animals, and plants have always done—evolve!
Source: https://academic.oup.com/eurpub/article/35/1/3/7815848

Comparison of maternal and neonatal outcomes of midwifery-led care with routine midwifery care: a retrospective cohort study
Shirin Shahbazi Sighaldeh, Elaheh Eskandari, Shahla Khosravi, Elham Ebrahimi, Shima Haghani & Fatemeh Shateranni
BMC Nursing volume 24, Article number: 158 (2025)
ABSTRACT
Introduction
Globally, the management of low-risk pregnancies by midwives often leads to a more natural childbirth process, which enhances physical and psychological outcomes for mothers and their babies. Midwives implement various models of maternal care in practice. This study investigates and compares maternal and neonatal outcomes associated with midwifery-led care versus routine midwifery care in private hospitals in Iran.
Methods
This retrospective cohort study was conducted in Iran in 2022. The study population consisted of two groups including 387 women in the Routine Care Group (RCG) and 397 women in the Private Care Group (PCG). Participants were selected through continuous sampling in accordance with the inclusion criteria. The two groups were compared in terms of some maternal and neonatal outcomes. The research data collection tool was a researcher-made checklist with variables adjusted according to the ‘Iman’ system of the Iran Ministry of Health. Based on this tool, the data were extracted from the mentioned system and analyzed with SPSS software.
Findings
The results indicated no significant difference between the two groups in terms of the type of delivery (p = 0.999), the use of forceps or vacuum (P = 0.5) and transferring the mother to the operating room (OR) or the intensive care unit (ICU) immediately after delivery (P = 0.744). However, there was a statistically significant difference between the two groups in terms of labor pain control (P < 0.001), induction of labor (P < 0.001), and the use of episiotomy (P < 0.001). Regarding neonatal outcomes, there was no statistically significant difference between the two groups in relation to the average infant weight (P = 0.46), Apgar score (P = 0.75), need for resuscitation (P = 0.999), skin-to-skin contact (P = 0.626), initiation of breastfeeding (P = 0.241) and admission to the neonatal intensive care units (NICU) (P = 0.66).
Conclusion
Given the positive impact of private care on key maternal outcomes, it is recommended that health policymakers create the conditions necessary for establishing a continuous midwifery care model in both governmental and private hospitals. Besides, more quantitative, qualitative, and especially mixed methods research should be conducted to explore the challenges and facilitators of this model across various settings.
Source: https://bmcnurs.biomedcentral.com/articles/10.1186/s12912-025-02789-4
Early prediction of preterm birth in cell-free RNA could reshape prevention strategies
by European Society of Human Genetics edited by Sadie Harley, reviewed by Robert Egan
May 24, 2025
Children born before 37 weeks of gestation have a considerably increased risk of dying before they reach the age of five. Predicting the risk of preterm birth (PTB) and hence implementing preventive strategies is complicated by the heterogeneity of the condition, the many unknown mechanisms involved, and the lack of reliable predictive tools.
Now, however, researchers have been able to show that blood cell-free RNA (cfRNA) signatures can predict PTB over four months before delivery date. The research was presented at the annual conference of the European Society of Human Genetics.
Dr. Wen-Jing Wang, an associate researcher at BGI Research in Shenzhen, China, together with team leader Professor Chemming Xu from the Obstetrics and Gynecology Hospital of Fudan University, Shanghai, China, and colleagues analyzed blood plasma samples from 851 pregnancies (299 PTB cases and 552 controls) at about 16 weeks gestation to identify cfRNA markers associated with spontaneous PTB, and found significant alterations in cfRNA between PTB and birth at term.
The study included both preterm births with intact membranes and premature rupture of membranes (when the waters break before labor starts), with fewer than 3% having a prior preterm birth.
“Being able to detect these predictive signals over four months suggests early biological priming for PTB, far earlier than current clinical recognition,” she says. “This extended window could revolutionize prevention strategies.”
Annually, about 13.4 million newborns worldwide are delivered prematurely, accounting for approximately one in 10 of all live births. Nearly one million of these preterm infants die each year, and PTB remains the primary cause of mortality in children under five.
Because children born preterm have immature organs that are not yet prepared for life outside the womb, it means that they will have a far higher risk of complications than those born at term. This can lead to a range of health issues such as respiratory problems, jaundice, feeding difficulties, and infections.
Long-term health problems for these children include cerebral palsy, epilepsy, and blindness, and impose substantial emotional and financial burdens on families.
“Practically, our method uses the same blood draw timing as routine Non-Invasive Prenatal Testing (NIPT), enabling dual testing. Current cfRNA sequencing costs are similar to NIPT pricing, but future optimization using targeted qRT-PCR panels could reduce expenses significantly. This creates a potential route to both monitoring patients at high risk and for wider population-level screening,” says Dr. Wang.
Before this diagnostic technique can be used more widely, the researchers say that standardized protocols for sample handling need to be developed, given RNA’s instability compared with DNA.
Prediction algorithms need to be developed in diverse population studies, and the causes of different PTB subtypes explored to be able to guide targeted interventions. The team is pursuing these goals and seeking to collaborate with other institutions in order to accelerate the use of their findings in clinical practice.
Chair of the conference, Professor Alexandre Reymond, said, “Advances in sequencing and analysis technologies are now offering many new diagnostic possibilities. This is a fascinating example of the use of sequencing readouts to evaluate risk, rather than assessing genetic background to assess predisposition.”
Source: https://medicalxpress.com/news/2025-05-early-preterm-birth-cell-free.html



Saving Tiny Lives: The Critical Need for Blood and Platelet Donations for Preemie Babies Undergoing Surgery
Premature infants, especially those born before 32 weeks of gestation, often face life-threatening challenges that require surgical intervention. These delicate babies are at heightened risk for bleeding complications due to their underdeveloped organs and fragile blood vessels. In fact, studies indicate that platelet transfusions are administered to 5.8%–53.0% of neonates with a gestational age at birth below 32 weeks, underscoring the critical need for these life-saving donations.
When it comes to blood versus platelets, it’s essential to understand the differences. Blood transfusions typically involve the whole blood or red blood cells, which help provide oxygen to the body’s tissues. For preemie babies, blood transfusions are often required to address anemia, a condition where the body doesn’t have enough red blood cells to carry sufficient oxygen. Platelet transfusions, on the other hand, are crucial for babies who are at risk of bleeding or have low platelet counts, which are essential for blood clotting. While blood transfusions address oxygen needs, platelet transfusions play a vital role in preventing severe hemorrhaging in these tiny patients.
The impact of blood and platelet transfusions on preemie babies cannot be overstated. For instance, a study involving neonatal surgeries revealed that 14% of neonates received perioperative red blood cell transfusions. Among those transfused, 30-day mortality rates were significantly higher, and they also experienced increased rates of complications such as wound dehiscence, mechanical ventilation beyond 48 hours, cardiac arrest, and septic shock. Platelet transfusions, however, are often the key to minimizing bleeding risks during surgeries and promoting recovery in fragile babies.
Recognizing the importance of these donations, I recently contributed by donating platelets to support children undergoing cardiac surgery. This experience highlighted the profound difference that blood and platelet donations make in the lives of critically ill children. Each donation has the potential to save lives and improve outcomes for these vulnerable patients. If you’re considering how you can make a tangible impact, donating blood or platelets is a powerful way to help. Your donation could be the one that gives a tiny baby the chance to grow, thrive, and lead a healthy life. To learn more about how you can donate and make a difference, visit your national blood donation agency’s website. Your generosity can be the lifeline these babies desperately need.




Surf’s up in Sierra Leone
Sierra Leone’s beaches and waves make them attractive for surfers. But the country has just one surf club. It tries to get boys and girls off the streets and into the water, despite equipment and personnel being in short supply. Sierra Leone is still infamous for its civil war and poverty. But it’s also incredibly beautiful. Enjoy the breathtaking views from Bureh Beach — a perfect spot for surfing.