COMMUNITY
New Zealand is an island nation in the southwestern Pacific Ocean. The country geographically comprises two main landmasses—the North Island and the and around 600 smaller islands. Because of its remoteness, it was one of the last lands to be settled by humans. New Zealand is a developed country and ranks highly in international comparisons of national performance, such as health, education, economic freedom and quality of life (Wikipedia). The preterm birth rate in New Zealand was 7.56% in 2010 per World Health Organization (WHO). The Global average is 11.1%; USA is at 12%. New Zealand notes and is researching the reasons for the significant disparity in Māori and Pacific New Zealand mothers compared to the general population. See Perinatal and Maternal Mortality Review Committee:http://www.hqsc.govt.nz/assets/PMMRC/Publications/tenth-annual-report-FINAL-NS-Jun-2016.pdf
Our Neonatal Womb Community is made up of a vastly diverse population of travelers and providers; some easily identifiable, others within the quiet spaces that keep us connected. Alistair Gunn is a Pediatric Scientist from New Zealand making significant contributions to our community.

Alistair Gunn, New Zealand -Pediatric Scientist
Alistair Jan Gunn, Professor, Physiology and Paediatrics, a Paediatrician-scientist in the Department of Physiology at the University of Auckland, has conducted groundbreaking research into the mechanisms and treatment of asphyxial brain injury, identifying compromised fetuses in labour and prevention of life threatening events in infancy.
His research helped to establish mild cooling as the first ever technique to reduce brain injury due to low oxygen levels at birth. This simple and effective treatment is now standard care around the world.
Full Source: http://www.newbornbrain2015.com/faculty/alistair-gunn/
BMC Pregnancy and Childbirth Morbidity and mortality among very preterm singletons following fertility treatment in Australia and New Zealand, a population cohort study: Alex Y Wang – Abrar A. Chughtai _ Kei Lui – Elizabeth A. Sullivan
The Abstract below addresses recent and ongoing research exploring preterm birth and risks of congenital abnormalities in relationship to Assisted Reproductive Technology (ART), Hyper-ovulation(HO) and Artificial Insemination (AI) in Australia and New Zealand. The studies find risk of congenital abnormality significantly increases after ART and AI; the risk of morbidities increases after ART, HO and AI. For me, one take-away is the recommendation that “Preconception planning should include comprehensive information about the benefits and risks of fertility treatment on the neonatal outcomes”. Research indicates that rates of mortality and morbidity among births following fertility treatment were higher than those conceived spontaneously.
Full Source: https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-017-1235-6
INNOVATIONS
 HELLO NanoString (State-of-the-Art Digital Technology)!
HELLO NanoString (State-of-the-Art Digital Technology)!
Promising new blood-test for preterm birth risk
14 February 2017
The researchers have already identified a unique molecular fingerprint in blood taken from women at 20 weeks of pregnancy who all went on to have their babies early. The fingerprint was not present in blood taken from women at the same stage in pregnancy who went on to deliver at term.
The team are now following up that pilot study with a two-year study that will test a bigger pool of samples, including samples taken at 15 weeks as well as at 20 weeks, to check whether the fingerprint is a reliable biomarker for preterm birth.
“This is exciting, as it could potentially lead to much better outcomes for the babies and their mothers, in the short and long terms, says study co-lead and Liggins Institute Professor Mark Vickers. “It could enable the targeting of existing and future therapies to delay or even prevent preterm birth.”
The potential biomarker revealed in the pilot study was derived from micro-RNA (miRNA) analysis. MiRNAs are small non-coding RNA molecules that play key roles in the regulation of gene expression. MiRNAs are also known to be involved in the development of and protection from a range of diseases. Recent studies in this fast-emerging field have highlighted the potential for miRNAs as biomarkers for osteoporosis, cancer and the pregnancy complication pre-eclampsia.
The Auckland researchers used state-of-the-art digital technology called NanoString that is much more sensitive and faster than other available methods.

Premature birth linked to hurdles in later life – April 29, 2017 – Lorilei Mason
Hundreds of babies are born prematurely each year in New Zealand, some as early as 23 weeks gestation and many develop and grow into healthy children and adults.
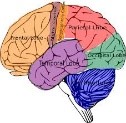
But the latest results from an internationally-acclaimed study following 110 New Zealand babies from birth has found that abnormalities in the brains of some born very prematurely persist into late childhood, affecting their motor skills, IQ and social skills.
The study, funded by the Health Research Council and the Neurological Foundation, has been following the babies – born at 32 weeks gestation or earlier – since 1998.
According to a highly-acclaimed study, abnormalities in the brains of a third of premature babies can persist into late childhood. Source: 1 NEWS
The researchers – Professor Lianne Woodward and neonatologists Professor Terrie Inder and Professor Nicola Austin – MRI scanned the brains of the trial babies at birth at Christchurch Hospital.
Their highly-acclaimed early work discovered that abnormalities within the developing white matter or “cabling networks” of the brain after birth could potentially explain the motor and cognitive impairments often experienced by children born very prematurely.
Please view their informative and interesting video here: https://www.tvnz.co.nz/one-news/new-zealand/premature-birth-linked-hurdles-in-later-life
Full Article Source: https://www.tvnz.co.nz/one-news/new-zealand/premature-birth-linked-hurdles-in-later-life
 And on The Other Hand ………………..
And on The Other Hand ………………..
Many Premature Babies Do Fine in School – By ASHLEY WELCH CBS NEWS June 12, 2017
The report, published in JAMA Pediatrics, finds that babies born early often catch up to their peers academically. Researchers report this recent study may ease the minds preemie families when it comes to how well their children may perform in school. The article shares the following interesting findings:
About 10 percent of babies in the U.S. are born prematurely — before 37 weeks of pregnancy, according to the Centers for Disease Control and Prevention.
“We know a lot about the medical and clinical outcomes [of premature babies] and we know some about short-term educational outcomes, but what we didn’t know is how the babies do once they get further out into elementary school and middle school,” the study’s first author Dr. Craig Garfield, associate professor of pediatrics and of medical social sciences at Northwestern University Feinberg School of Medicine, told CBS News.
The study found that two-thirds of babies born at only 23 or 24 weeks were ready for kindergarten on time. The researchers were surprised to see that nearly 2 percent of these extreme preemies even achieved gifted status in school.
Though extremely premature babies often scored low on standardized tests, preterm infants born 25 weeks or later performed only slightly lower than full-term infants. For babies born after 28 weeks, the differences in test scores were negligible.
The researchers point out important caveats to the study, including that babies who died in infancy were excluded from the data set. It also doesn’t take into account some of the infants’ medical issues related to premature birth or information about factors that may have helped these children performed well in school, such as their biological makeup or if they got extra support from family or school programs.
Garfield said that future research should look into what makes a difference in which babies go on to perform well in school and which do not.
“The next step is to ask how can we support babies who are born early as they transition into the school system and what can we do to help those families in helping them perform to the best of their ability in school,” he said.
 Full Article: http://www.cbsnews.com/news/premature-babies-preemies-catch-up-in-school-study/
Full Article: http://www.cbsnews.com/news/premature-babies-preemies-catch-up-in-school-study/

HEALTH CARE PARTNERS
NEW TECHNOLOGY DETECTS CRITICAL FEEDING PROBLEMS IN PREEMIES
– March 24, 2017

Many babies born prematurely have trouble eating because of swallowing difficulties, making new moms anxious during bottle feeding or breastfeeding. To better diagnose feeding issues, clinicians in the neonatal intensive care unit (NICU) at Baylor University Medical Center at Dallas developed an innovative new way to assess swallowing in the hospital’s tiniest patients, giving new moms more confidence to feed their newborns safely. They conducted a first-of-its-kind research study to prove the technology’s safety and effectiveness for swallowing assessment in newborns, recently published in the Journal of Perinatology.

The science of nurturing and its impact on premature babies – PBS NewsHour (PART 2) – Published on May 31, 2017: A long-term study on helping preterm babies, using the simplest of interventions, is showing signs of promise. In part two of our story, William Brangham explores the study’s outcomes, as well as questions about the complex past of the doctor behind it.
PREEMIE FAMILY PARTNERS
Check out this innovative Child-Centered Program dedicated to healing patterns originating from prenatal and perinatal trauma as well as bonding and attachment challenges!
BEBA: A Center for Family Healing
What is BEBA? – BEBA is a child centered, family clinic that is dedicated to helping babies, children and families heal early restrictive patterns originating from prenatal and perinatal trauma, as well as bonding and attachment issues. These early experiences can have long term effects on one’s emotional, psychological and physical health and wellbeing. BEBA is a non-profit research and teaching clinic with branches in Santa Barbara and Ojai, CA.
BEBA’s Goal-BEBA’s goal is to expand our understanding of the nature of early stress and trauma from conception through the first years of life and its effects on human development. It is dedicated to researching these issues and educating the professional and public sectors about its findings. Early trauma can occur anytime during conception, gestation, birth, the events following birth and the bonding and attachment phases. It can leave restrictive imprints in the nervous system and affect future behaviors, emotions, belief systems, psychological orientations and physical health and wellbeing. BEBA supports the development of successful strategies and interventions to help babies, children and families heal and release negative and/or restrictive imprints from those early periods.
About Early Trauma-
EXPLORE and CONTEMPLATE THESE IMPORTANT QUESTIONS AND COMPELLING INFORMATION ADDRESSING THESE TOPICS!
- What is early trauma?
- Why is it important to heal early trauma?
- What scientific research supports the BEBA approach?
- What are some known causes of early trauma?
- What are some of the signs babies exhibit after experiencing trauma?
- What are some of the signs older children exhibit after experiencing trauma?
- What are common parental responses to child’s early trauma?
- What are common signs in teens and adults of early trauma?
Examples include:
- Hyperactivity
- Coordination and balance problems
- Gait problems
- Toilet training challenges
- Speech delays
- Learning disabilities
- Tantrums
- Inappropriate aggression/timidity
- Depression
- Nightmares
- Response out of proportion to stimulus
- Inability to make eye contact
- Inability to ask for help
- Rage toward parent(s) or others
- Hypersensitivity
- Health challenges like asthma and seizures
- Harmful behavior towards siblings
- Tactile defensiveness (desire to not be touched)

Full Source: http://beba.org/early-traum/
WARRIORS:
We are cultural creators empowered to create a better world.
Bruce reminds us that The Field gives shape to the material world and we have the potential to become Masters of our genes!
Wisdom of the Force – Jedi Master Bruce Lipton on Quantum Physics

Ricochet a surfing dog is most inspirational-
 Video Produced by CJ Albarran
Video Produced by CJ Albarran




 BLOG : Getting The “Hang” Of Neonatology In China
BLOG : Getting The “Hang” Of Neonatology In China


































 COMMUNITY
COMMUNITY 




 Not a Talker? (you kinesthetic travelers!)
Not a Talker? (you kinesthetic travelers!)












 +
+  = Innovations-
= Innovations-


 The publication “All AFRICA” provides us with a current perspective (09/23/16) regarding Kenya’s preterm birth challenges and proposed prevention and treatment solutions. Identification of factors contributing to the causes on neonatal deaths, preterm birth, and a focus on identifying current, cost effective and evidence based solutions are shared by the author, Muthoni Waweru.
The publication “All AFRICA” provides us with a current perspective (09/23/16) regarding Kenya’s preterm birth challenges and proposed prevention and treatment solutions. Identification of factors contributing to the causes on neonatal deaths, preterm birth, and a focus on identifying current, cost effective and evidence based solutions are shared by the author, Muthoni Waweru.
 (Part 3:
(Part 3: