Singapore, officially the Republic of Singapore, is an island country and city-state in Southeast Asia. The country’s territory comprises one main island, 63 satellite islands and islets, and one outlying islet. It is about one degree of latitude (137 kilometres or 85 miles) north of the equator, off the southern tip of the Malay Peninsula, bordering the Strait of Malacca to the west, the Singapore Strait to the south along with the Riau Islands in Indonesia, the South China Sea to the east, and the Straits of Johor along with the State of Johor in Malaysia to the north.
Singapore has a generally efficient healthcare system, even though health expenditures are relatively low for developed countries. The World Health Organisation ranks Singapore’s healthcare system as 6th overall in the world in its World Health Report. Singapore has had the lowest infant mortality rates in the world for the past two decades. In 2019, Singaporeans had the longest life expectancy of any country at 84.8 years. Women can expect to live an average of 87.6 years with 75.8 years in good health. The averages are lower for men.[479] Singapore is ranked 1st on the Global Food Security Index.
Source: https://en.wikipedia.org/wiki/Singapore
- GLOBAL PRETERM BIRTH RATES – Singapore
- Estimated # of preterm births: 8.2 per 100 live births/Global Average:
- Source- WHO Preterm Birth Rate (Per 100 Live Births)
- WHO Prematurity
- World Population Review
- WHO Country Consultation of Low and Preterm Birth Weight

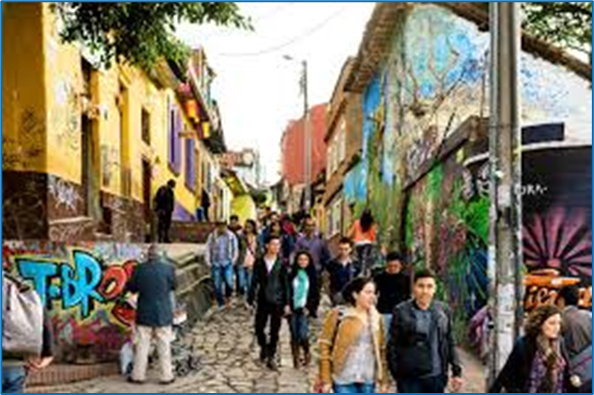
COMMUNITY
10 Surprising Facts About Doctors And Residents You Need To Know
By OnlineMedEd February 1, 2025
Key Takeaways:
- Financial Considerations: Medical professionals often face significant student loan debt, which can impact career choices and personal life decisions.
- Technological Integration: The integration of technology like telemedicine and electronic health records is transforming how doctors provide care and stay updated with medical advancements.
- Communication In Medicine: Effective communication skills significantly enhance doctor-patient relationships and improve treatment outcomes, emphasizing their importance alongside medical knowledge.
In the fast-paced and ever-evolving world of medicine, doctors and residents commit to a lifelong calling. These dedicated individuals spend countless hours honing their expertise, driven by a deep commitment to patient care and medical excellence. While the white coat and stethoscope symbolize readiness and a passion for their practice, the reality of their journey is far more complex, filled with challenges and responsibilities that often play a crucial role in shaping their careers and the care they provide.
This article goes beyond common perceptions, revealing ten surprising facts about doctors and residents that highlight the depth and complexity of their roles. Whether you’re a medical student preparing for the road ahead, an educator nurturing future providers, or a healthcare professional seeking deeper insight, these realities offer a fresh perspective on the field.
Understanding these intricacies fosters greater appreciation, resilience, and professional growth, ensuring that the next generation of physicians is equipped not only with medical knowledge but also with the tools to thrive in both their careers and personal well-being.
Fact 1: Many Doctors Face Student Loan Debt Long Into Their Careers
Becoming a doctor is one of the most rewarding professions, but the financial burden is significant. Many physicians graduate with over $200,000 in student loan debt, impacting career choices and personal milestones. Here are ways that student loan debt can impact medical professionals:
- Influences Specialty Decisions: Some choose higher-paying fields over passion-driven specialties.
- Delays Major Life Events: Homeownership, marriage, and family planning may be postponed until studies are completed.
- Requires Strategic Financial Planning: Understanding repayment options and budgeting is crucial.
Fact 2: Doctors Must Continually Update Their Knowledge
Medicine evolves rapidly, requiring lifelong learning to provide optimal patient care. Continuing education ensures physicians stay updated on the latest research, treatments, and technologies. Here are some reasons why:
- USMLE And CME Requirements: Ongoing exams and certifications keep doctors current.
- Medical Advancements: New treatments, AI tools, and clinical protocols evolve constantly.
- Efficient Learning Strategies: Consistent review of clinical content allows doctors to maintain their medical mastery and mitigate skill decline.
Fact 3: Technology Is Transforming How Doctors Practice Medicine
Technology is revolutionizing healthcare for the better and improving efficiency. Below are some ways technology is changing the healthcare game:
- Electronic Medical Records (EMRs): Digitally store and organize patient health information, improving accessibility, documentation accuracy, and care coordination.
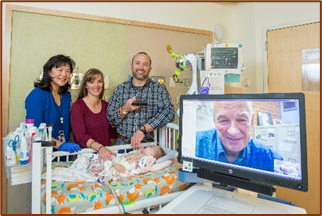
- Telemedicine: Expands access to remote and underserved populations.
- AI And Automation: Enhances diagnostics, workflows, and patient care.
Fact 4: Many Doctors Pursue Research Alongside Clinical Practice
For many doctors, the desire to discover new medical knowledge is as strong as the calling to patient care. Many doctors balance clinical work and medical research to push the field forward.
Medical research:
- Advances Evidence-Based Medicine: Research findings shape treatment protocols.
- Improves Patient Outcomes: Clinical trials lead to breakthrough therapies.
- Strengthens Analytical Skills: Evaluating data sharpens clinical decision-making.
Fact 5: Communication Skills Are As Important As Medical Knowledge
Beyond expertise, strong communication enhances patient trust and treatment outcomes by ensuring clarity, collaboration, and understanding. Below are some communication skills that medical professionals should value:
- Clear Explanations: Helps patients make informed decisions.
- Interdisciplinary Teamwork: Ensures seamless care coordination.
- Active Listening: Strengthens doctor-patient relationships.
Fact 6: The Number Of Female Physicians Is On The Rise
In recent years, the medical field has witnessed a transformative shift as the number of female physicians steadily increases. Women now make up over 50% of U.S. medical school students, creating a more inclusive healthcare environment.
This change not only reflects broader societal advancements but also heralds a new era where diverse perspectives lead to more comprehensive patient care. Here are a few reasons why this trend is a positive force in the medical community:
- Enhancing Patient Perspectives: Women in medicine improve representation and inclusivity.
- Expanding Leadership Roles: More female doctors are entering executive positions.
- Shaping Mentorship And Education: An increasing number of programs support future generations of female physicians.
As more women enter the field, efforts to support career advancement, mentorship, and leadership opportunities continue to grow. These changes contribute to a more balanced healthcare workforce, ensuring that medical education and patient care reflect the diverse needs of the communities they serve.
Fact 7: Residents Are Both Students And Employees
Residents face a tough battle, as they are expected to balance learning with employment. The responsibilities of patient care, combined with a deep, unyielding commitment to mastering the breadth and depth of medical knowledge, create a unique dynamic.
Residents deal with:
- Hands-On Experience: Residents manage cases under supervision, participate in medical procedures, and deliver expert care in high-stakes environments.
- Long Hours And High Stress: Demanding schedules prepare residents for independent practice.
- Balancing Education And Work: Requires strategic planning and smart time management to stay sharp.
Fact 8: Doctor-Patient Relationships Influence Treatment Outcomes
At the heart of every successful treatment plan lies a strong doctor-patient relationship. This dynamic significantly impacts treatment outcomes, as trust and communication form its foundation. Here’s why this bond is essential to a positive healthcare experience:
- Empathy Improves Patient Engagement: Positive experiences with doctors encourage patients to follow treatment plans accordingly.
- Communication Enhances Understanding: Simplified explanations of medical conditions and solutions lead to informed decisions.
- Trust Strengthens Compliance: Patients are more likely to return for follow-ups and engage in routine check-ups when they trust their healthcare provider.
Developing effective communication and interpersonal skills allows physicians to foster meaningful connections with their patients. When patients feel understood and respected, they are more likely to adhere to medical advice and treatment plans, ultimately leading to improved health outcomes.
Fact 9: Wellness Programs Are Becoming More Common In Medical Training
The rumors are true: Becoming a doctor is an incredibly long and arduous process. Thankfully, in recent years, wellness programs have been developed to support students and residents with healthy coping mechanisms. These initiatives, including the ones listed below, are a testament to the growing recognition of the demanding pressures faced by medical students and residents and their impact on mental health and overall well-being.
- Mental Health Support: Resources such as counseling help prevent burnout.
- Work-Life Balance Strategies: Encouraging self-care and mindfulness.
- Peer Support Networks: Strengthening community and resilience.
Fact 10: Global Health Opportunities Are Available To Doctors And Residents
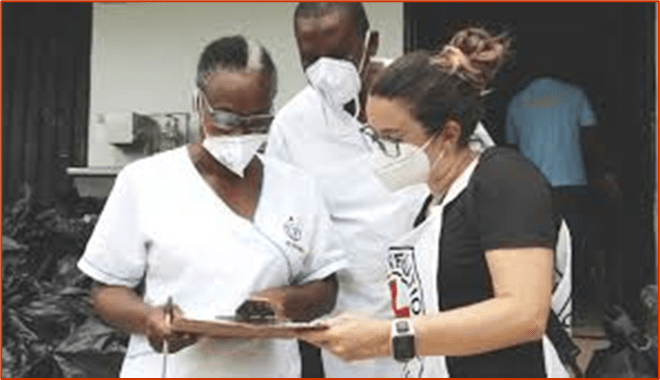
Joining global health initiatives allows medical professionals to see firsthand the different healthcare challenges that occur worldwide. This experience can be pivotal in developing resilience and adaptability, skills that are crucial in any medical setting. For residents, these opportunities can be eye-opening, offering real-world applications of their clinical skills in diverse environments. Here’s why global opportunities can be beneficial for the careers of doctors and residents:
- Exposure To Diverse Medical Environments: Broadens clinical expertise and adaptability to different clinical settings.
- Develops Problem-Solving Skills: Teaches current and aspiring healthcare providers how to work with resource-limited care strategies.
- Strengthens Public Health Impact: Contributes to underserved communities worldwide.
These opportunities enrich one’s medical expertise and broaden perspectives on health disparities, resource management, and cultural sensitivity.
Final Thoughts
The road to becoming a doctor is filled with challenges, sacrifices, and unexpected realities, yet it remains one of the most enriching careers. Understanding these crucial facts about doctors fosters greater empathy and appreciation for those dedicated to medicine. While the path is demanding, each step brings the opportunity to grow, refine skills, and make a meaningful impact on patient care.
By embracing a structured and comprehensive approach to medical education, future providers can develop true mastery. Investing in both clinical knowledge and personal well-being ensures not only success in training but also longevity and fulfillment in practice. Whether you’re a medical student, resident, or educator, every effort you make strengthens your ability to provide exceptional, compassionate care, shaping the future of healthcare for the better.
Source: https://www.onlinemeded.com/blog/facts-about-doctors

Benjamin Kheng – REALLY IN LOVE (Official Music Video)

Benjamin Kheng Nov 28, 2024 #BenjaminKheng #REALLYINLOVE
REALLY IN LOVE Written by: Benjamin Kheng Produced by: Benjamin Kheng, Evan Low Performed by: Benjamin Kheng Mixed & Mastered by: Charlie Kurata Spatial Audio Master by: Luke Nicholas Foo

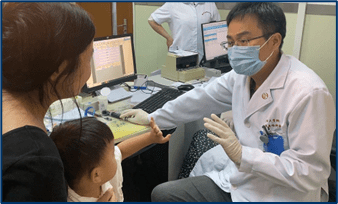
Team from KKH, SGH aims to develop screening tool to identify women at risk of premature births

Elisha Tushara UPDATED Oct 04, 2024, 01:00 PM
SINGAPORE – Her son weighed just 700g when he was born at 24 weeks after she spent the two weeks prior in hospital due to vaginal bleeding and cervix dilation.
Ms So Bee Leng’s son, Ethan Ang, was born in 2017 with multiple disabilities stemming from his extreme prematurity. At seven days old, he underwent his first major surgery when his intestines were operated on.
For the next five years, he underwent four more major operations, which included implanting a cochlear hearing device, laser eye surgery to help with his vision and placing a feeding device through his belly to the stomach.
It is currently a challenge to identify mothers at risk of giving birth to premature babies as the only gauge is when mothers have had previous preterm births, like Ms So, said Professor Teoh Tiong Ghee, director of maternal and child global health and care transformation at KK Women’s and Children’s Hospital (KKH).
To proactively reduce and prevent prematurity, a 10-member team of doctors specialising in newborn care and high-risk pregnancies from KKH and Singapore General Hospital (SGH) will start work on a new Preterm Pregnancy Prevention Programme in October.
The team aims to create a national database of all preterm pregnancies to identify risk factors, and then use this information to develop a screening prediction tool that can accurately assess the risk of preterm pregnancies.
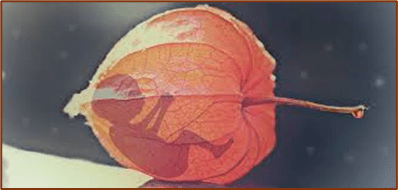
A baby born before 37 full weeks of pregnancy is considered to have been born preterm or prematurely. A preterm baby’s organs may not be fully developed.
A full-term pregnancy typically lasts about 40 weeks, and babies’ birth weights typically range from 2.5kg to 4.5kg.
Globally, 13.4 million babies – 10 per cent of all births – are born prematurely each year and one million die from preterm complications.
Prematurity is the leading cause of death for children under five.
In 2023, 8.2 per cent of births in Singapore were premature, slightly lower than the 8.8 per cent recorded in 2014.
Recalling the dilemma she faced when told she might deliver early and her baby would develop health complications, Ms So, 38, said: “I was given the choice to either terminate the pregnancy or continue with bed rest in the hospital until I gave birth.
“After weighing the pros and cons, and discussing with my husband, we decided to carry on and accept whatever may come in the future.”
When she conceived again in 2023, her doctor told her she was at risk of another premature delivery. She was referred to the Preterm Birth Clinic at KKH’s Stork Centre, where she was closely monitored.
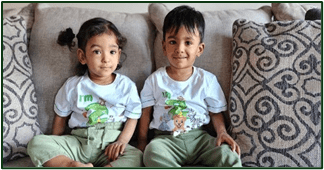
She underwent a procedure to stitch her cervix – the birth canal opening – when she was 12 weeks along, paving the way for the full-term birth of her daughter, Alysha Ang, at 38 weeks.
Called a cervical cerclage, the procedure is done to help the cervix hold a pregnancy in the womb to prevent preterm birth.
Dr Ilka Tan, a senior consultant at KKH’s department of maternal foetal medicine who oversaw Ms So’s care during her second pregnancy, said that infants are able to survive outside the uterus at 24 weeks.
She added that though there are rare cases of infants surviving when born at 22 or 23 weeks, the “outcome is still not very good” for these babies.
Acknowledging that there have been reports from around the world of some babies born around 22 weeks who have survived, she said: “Those are single anecdotal cases, but it’s not the norm.”
If diagnosed through screening and predictive tests early, mothers who are at risk of preterm births can undergo various treatments to help them bring the pregnancy to term, Dr Tan said.
These include taking the hormone progesterone and getting a cervical cerclage.
The Preterm Pregnancy Prevention Programme will use information collated to study common characteristics among women who deliver prematurely. This in turn can be used to develop a prediction tool to identify expectant mothers who are at risk of preterm births early, so that preventive measures can be taken.
“What we’re trying to do is to get all these demographics, and use biomarkers from blood and cervical length measurements, to try to predict each woman’s personalised risk so as to target with specific therapy,” said Prof Teoh.
The programme is funded by a $500,000 grant from Far East Organization.
Besides the child potentially suffering long-term health consequences and an increased risk of disability and developmental delays, the parents and the rest of the family experience long-term stress too, Prof Teoh noted.
“Some have to stop work to look after the kid. So not only does it have a psychological impact on the family, it’s got a big financial impact as well,” he added.
Dr Tan also leads the Preterm Birth Clinic at KKH that provides specialised care for women who may have a higher risk of having premature babies.
The clinic began operations in July 2021 and had 100 patients that year. In 2024, 402 patients were referred to the clinic from January to September.
Ms. So said she received personalised care and attention at the Preterm Birth Clinic to help her carry her second child to term.
“I was seen by the same doctor – it wasn’t random. So I felt well-looked after and relieved. I was assured that there was a plan to help me, and that was important.”

PREEMIE FAMILY PARTNERS

Credit: Pixabay/CC0 Public Domain

Skin-to-skin ‘kangaroo care’ found to boost neurodevelopment in preemies
by Erin Digitale Stanford University August 7, 2024
Skin-to-skin cuddling with a parent has lasting cognitive benefits for premature babies, according to a new Stanford Medicine study. Preemies who received more skin-to-skin contact, also known as kangaroo care, while hospitalized as newborns were less likely to be developmentally delayed at 1 year of age, the study found.
The research, which was published online July 11 in The Journal of Pediatrics, showed that even small increases in the amount of skin-to-skin time made a measurable difference in the babies’ neurologic development during their first year.
“It’s interesting and exciting that it doesn’t take much to really improve babies’ outcomes,” said the study’s senior author, Katherine Travis, Ph.D., who was an assistant professor at Stanford Medicine when the study was conducted and is now an assistant professor at Weill Cornell Medical School and Burke Neurological Institute.
The study’s first author is Molly Lazarus, a clinical research coordinator in pediatrics previously at Stanford Medicine and now at Weill Cornell Medical School.
The intervention is simple: With the baby only in a diaper, a parent holds the baby on their chest, next to their skin. But because hospitalized preemies are small and fragile, and often hooked to lots of tubes and wires, holding the baby can seem complicated. Parents may need help from their baby’s medical team to get set up. That work is worth it, the study showed.
“It didn’t matter if the baby was from a high- or low-income family; the effects we found were the same. And it didn’t matter if the baby was sicker or less sick—both responded to this treatment,” Travis said.
Neurological complications are challenging
Over the last 50 years, preemies’ survival rates have improved dramatically thanks to better treatments for many of the complications of prematurity, which is defined as being born at least three weeks early. For instance, neonatologists have developed effective approaches to help preemies breathe, even with immature lungs, while in the neonatal intensive care unit.
But premature birth still leaves babies at risk for long-term neurodevelopmental problems, including developmental delays and learning disabilities. Doctors and families have long hoped for treatments they could use during the newborn period to prevent such challenges.
“Ultimately, we want our patients to be healthy kids who can achieve the same milestones as if they didn’t come to the NICU,” said study co-author Melissa Scala, MD, clinical professor of pediatrics. Scala is a neonatologist who cares for preemies at Lucile Packard Children’s Hospital Stanford.
“Our finding legitimizes skin-to-skin care as a vital intervention in the neonatal intensive care unit to support our goal of getting that child out of the hospital, able to learn and develop,” Scala said.
Skin-to-skin care was first used in low-income countries to boost babies’ survival, where it is often used for healthy infants born after full-term pregnancies. In rural or impoverished areas, it is an essential way to keep newborns warm, promote parent-child bonding and facilitate the start of breastfeeding.
It’s been slower to catch on in the United States, especially for premature babies, who generally receive high-tech intensive care. But a growing body of research suggests that the practice has benefits for preemies’ brains, possibly because it could offer some of the same developmental inputs they would have received if they had not been born early.
More skin-to-skin was better
The research team reviewed medical records for infants who were born very prematurely, meaning at least eight weeks early, and were cared for at Lucile Packard Children’s Hospital Stanford between May 1, 2018, and June 15, 2022. Nurses in the hospital’s NICU had begun making notes in patients’ medical charts about developmental care practices, including the amount of time parents held babies skin-to-skin, shortly before the study began.
The study included 181 preemies who did not have genetic or congenital conditions known to affect neurodevelopment and who had received follow-up evaluations after they left the NICU. All very premature babies are eligible for care through California’s High Risk Infant Follow-Up program until age 3. The program provides developmental testing and connects families to appropriate therapists if their children have developmental delays.
The study used records from follow-up evaluations that the babies received at 6 and 12 months’ adjusted age, meaning their ages were corrected to account for how early they were born.
The evaluation included measures of visual-motor problem solving in standard tasks (such as dropping a cube into a cup) and expressive and receptive language skills (such as turning to see where the sound of a bell is coming from).
In addition to accounting for infants’ gestational age (how early they were born), the outcomes were adjusted for families’ socioeconomic status and for four common complications of prematurity: bronchopulmonary dysplasia, a breathing complication; brain hemorrhage, or bleeding; sepsis, an infection of the bloodstream; and necrotizing enterocolitis, an intestinal condition.
The infants in the study were born, on average, at about 28 weeks’ gestation, or about 12 weeks before their due dates. They stayed in the hospital for an average of about two and a half months.
Babies in the study averaged about 17 minutes a day of skin-to-skin care, usually in sessions lasting more than an hour but occurring less than two days per week. Seven percent of families did not do any skin-to-skin care, and 8% did more than 50 minutes per day.
Small increases in the amount of skin-to-skin care were linked to large differences in 12-month neurodevelopmental scores. An average of 20 minutes more per day of skin-to-skin care was associated with a 10-point increase on the scoring scale used for neurodevelopment. Similar to an IQ test, the scale has an average of 100 points; a score of 70 or less suggests significant developmental delays.
The frequency and duration of skin-to-skin contact predicted 12-month cognitive scores even after controlling for possible confounding factors, including the infant’s gestational age and medical complications, and the family’s socioeconomic status and frequency with which they visited the NICU.
How does it work?
Although the study was not set up to explore how skin-to-skin care benefits babies’ brains, the researchers have some educated guesses.
“We think of the womb as our benchmark for preterm babies. In utero, a fetus is physically contained, listening to the maternal heartbeat, hearing Mom’s voice, probably hearing her digest her sandwich,” Scala said. “In the NICU, they’re not next to anybody, and they hear the fan in the incubator; it’s a very different environment. Skin-to-skin care is probably the closest we can get to mimicking the womb.”
Parents can also benefit from skin-to-skin care, and this in turn may benefit their newborns, the research team said.
“The environment of the NICU is very stressful for parents and babies, and skin-to-skin care may buffer that,” Travis said, noting that it is not unusual for parents with a very tiny, sick baby to develop post-traumatic stress disorder.
In addition, many preemies are not developmentally ready to breastfeed, and skin-to-skin care can provide an alternate way to promote bonding between parents and babies.
The researchers hope their findings will motivate medical teams to help parents provide skin-to-skin care in NICUs across the country and will encourage parents by showing them the long-term benefits of this simple but important technique.
Packard Children’s recently expanded its infant developmental care program by hiring neurodevelopmental nurse practitioners, more physical and occupational therapists, a psychologist, and child life and music therapy experts for their NICU and intermediate care nurseries. The expanded team can make customized developmental care plans for high-risk infants.
Scala hopes other hospitals will follow suit.
“I would love for people to see this as part of the medical plan, not just something nice we’re doing, but to be really intentional about it,” Scala said. “Our findings underscore the value of having parents on the intensive care unit, doing this important part of infant care.”
Source:https://scx1.b-cdn.net/csz/news/800a/2024/preterm-infant.jpg


Imagine giving birth at 22 weeks—facing the uncertainty, the emotional rollercoaster, and the challenges of an 8-month NICU stay. For Asma, this journey was life-changing, but it also ignited her passion for advocacy, helping other parents navigate the NICU experience with confidence and strength. Join us as Asma shares: ✅ Her raw & real experience as a NICU mom to baby Cylia Maria ✅ The emotional & logistical challenges of a long NICU stay ✅ The transition home—what she wishes she knew ✅ How sharing her story has fueled her passion for advocacy & parent empowerment ✅ Guidance for parents: questions to ask & how to take an active role in their baby’s care.

International Parent support Resources

Parent and patient organisations International
International Council of Multiple Birth Organisations / ICOMBO
International Federation of Spina Bifida and Hydrocephalus / IFSBH
International Patient Organistion for Primary Immunodeficiencies / IPOPI
Country Specific Organizations
Resources for NICU Families
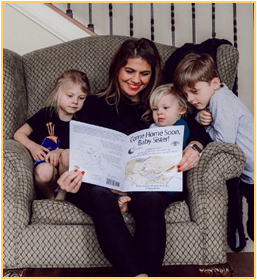
It can be very stressful having a baby in the NICU. During this time, it is helpful to include siblings as much as possible; to explain in simple terms what is happening with your new baby; to reassure them that they have not caused the baby to be early, sick, or small; and to remind them that they are not the source of your current worries. Most of all, you should reserve special time just for them, and remind them daily of your constant and unconditional love. More than ever, they need to feel secure, valued, safe, and loved by you and others.
Platypus Media is proud to offer a number of NICU sibling support resources. We hope these will be meaningful and useful for families experiencing the difficulty of having a child in the NICU.
The Come Home Soon coloring book series (available for baby boys and girls, in both English and Spanish) will help you guide your children to an understanding of why their baby sister or brother is in the NICU, and what they can do to help.
Rich and Creamy for Our Preemie, by Naomi Bar-Yam, ACSW, Ph.D., available in English and in Spanish, is a coloring book about how the NICU, milk banks, and families work together to help preemies.
Here is a list of other NICU sibling support resources:
- Hand to Hold sibling support webpage (www.HandToHold.org) offers sample activity pages and NICU video tour.
- No Bigger than My Teddy Bearby Valerie Pankow describes the NICU experience through the eyes of a new big brother.
- My Brother is a Preemie/My Sister is a Preemie:A Children’s Guide to the NICU Experienceby Abraham R. Chuzzlewit & Dr. Jos. A. Vitterito II gives a child-friendly introduction to the NICU.
- The Invisible Stringby Patrice Karst reassures children that even when loved ones are apart, they are always in each other’s hearts.
Keep reading for a list of organizations that help preemie families…
Different Dream serves as a gathering place for parents with special needs children.
Hand to Hold provides resources and support to parents of preemies, babies with special health care needs and new parents who have lost a baby.
Human Milk Banking Association of North American provides information and resources on donor milk banking for parents and health care providers. It also sets safety guidelines for all non-profit mothers’ milk banks in North America.
Kangaroo Mother Care promotes skin-to-skin contact, a universally available and biologically sound method of care for all newborns, and preemies in particular.
La Leche League International is a mother-to-mother breastfeeding support organization. They are a source of information and firsthand accounts related to providing preterm babies with breastmilk.
Managing the Neonatal Intensive Care Unit is an article from the Loyola University of New Orleans’ online nursing resource center. A great resource for students, professionals, and even parents of babies in the NICU.
March of Dimes (MOD) has a wealth of information about the NICU. They support an online community especially for NICU families. March of Dimes NICU Family Support programs operate in many NICUs. (Also available in Spanish.)
National Premature Infant Health Coalition consists of a variety of support organizations focused on improving the lives of parents and their preemies.
NICU Parent Support Site provides information, resources, and encouragement to reassure and support NICU parents.
Prematurity strives to support preemie parents by providing information on prematurity and preemie care.
Preemie Parent Alliance(PPA) represents a number of organizations that help support the parents of preemies and strives to improve the quality of the care they provide.
Preemie World brings together parents and professionals in the NICU. They strive to educate and help make the transition to home easier for everyone.
Ronald McDonald House serves as a home away from home for families with children receiving medical treatment. Families can do laundry, eat freshly cooked meals, sleep in private rooms, and gain/give support with other families.
Supplemental Security Income (SSI) and Medicaid Programs provide financial assistance for NICU medical expenses. Eligibility for assistance is determined by a baby’s birth weight rather than an income. You must apply for these programs shortly after your baby is born. Ask your social worker or care manager for assistance.
WIC (Women, Infants, and Children) provides nutritious foods to supplement diets, information on healthy eating, and referrals to health care for women, infants, and children up to 5 years. Even if you have been denied Medicaid due to financial reasons, you might still qualify for WIC.
This list can be found in the Resource for NICU Families section of our award winning Coloring Book for the Big Brothers and Big Sisters of the NICU.
Source: https://www.platypusmedia.com/resources-for-nicu-families

HEALTHCARE PARTNERS
Fetal heart rate (FHR) patterns are a critical tool for assessing a baby’s well-being during pregnancy and labor. Nurses must understand how to interpret these patterns to ensure safe care. Here are the key takeaways:
- Baseline FHR: Normal range is 110-160 bpm. Below 110 bpm (bradycardia) or above 160 bpm (tachycardia) may signal distress.
- Variability:
- Moderate (6-25 bpm): Healthy oxygenation.
- Absent or minimal: Potential concern.
- Marked (>25 bpm): Possible distress.
- Decelerations:
- Early: Harmless, mirrors contractions.
- Late: Indicates uteroplacental issues, requires action.
- Variable: Linked to cord compression, may need intervention.
- Three-Tiered Classification:
- Category I: Normal.
- Category II: Indeterminate, needs closer monitoring.
- Category III: Abnormal, requires urgent action.
Nurses must act quickly on abnormal patterns by repositioning the mother, administering oxygen, or preparing for emergency delivery. Accurate monitoring, documentation, and clinical judgment are essential for ensuring the safety of both mother and baby.

Fetal Heart Rate Patterns: Normal and Abnormal FindingsFetal Heart Rate Patterns: Normal and Abnormal Findings, VEAL CHOP – Maternity Nursing
Code Blue in The NICU

Joseph B. Philips, III, MD
The moonlighter had just returned with our dinners when the code alarm sounded. Almost simultaneously, our pagers went off “Code infant 3312.” We all knew who it was. The 23-week gestation, two-day-old baby had coded earlier in the afternoon and had been doing poorly since. Oxygen saturations were in the low 80s despite maximal support, and blood pressures were marginal on dopamine, dobutamine, and epinephrine drips. Upon entering the room, we found the infant with saturations in the 40s and a heart rate in the 50s. We quickly assumed our positions around the warmer. The resident began chest compressions, the respiratory therapist hand bagged, the fellow at the head of the bed assessed the airway and ordered fluid pushes and medications, the bedside nurse administered the medications, and I, the attending physician, oversaw it all. The nursing staff also rapidly began their roles, one opening the crash cart and drawing up drugs, another charting, and multiple others observing and ready to assist if needed.
We quickly fell into our all-too-familiar routine, counting “one, two, three” for chest compressions, followed by “breath.” Over and over again. “Ten mils normal saline,” said the fellow, followed by “epi, point 0 five” every five minutes. The intern took over the chest compressions after about 10 minutes, but the cadence remained the same. Blood was bubbling up the endotracheal tube, indicating the presence of a pulmonary hemorrhage. A nurse was dispatched to retrieve emergency-release blood from the blood bank. The saturation and heart rate were steadily falling.
The mother was literally rolling on the floor, wailing, “Save my baby! Save my baby!” over and over again.
Despite several rounds of fluids and epinephrine plus a push of the blood, the baby continued to deteriorate. I knelt beside the mother, put my hand on her shoulder, and asked her to listen. She immediately stopped her wailing and looked me in the eye. I told her that her baby was dying, that we were going to stop CPR as it was not working, and that her baby’s brain had been irreversibly damaged. She nodded in agreement.
“Stop,” I said. The scene instantly shifted from the hustle and bustle of a code to a stony silence pierced only by the sobs of the mother whom the nurses had assisted into a recliner chair. The monitor was turned off, the ventilator and lines were disconnected, syringes and other debris were removed from the bed, and the baby was wrapped in a blanket and placed in mom’s arms. The nurses began their familiar postmortem care routine. The fellow auscultated the baby’s chest and confirmed the death.
We returned to the workroom and ate Chinese takeout. I had cashew shrimp. I conducted a debrief during our meal, asking everyone how they felt. The intern was visibly shaken, with a tear trickling down her cheek. It was July, and this was the first death of a patient in her charge since she had become a real doctor. “His life slipped through my hands when you told me to stop,” she said. One of the upper-level female residents hugged her as she sobbed for a while before regaining her composure and resumed picking at her food.
For myself and the fellow, this death was one of many, but each death is new all over again and is a fresh reminder of our human frailty.
Few outside our world would understand a situation like this. We were eating while a baby had just died and a mother was grieving. For her, life had just changed forever. For us, we had to nourish ourselves to have the strength to continue caring for the living. Nothing taught in medical school can prepare one for these moments. They must be experienced first-hand, processed, and reflected upon. Doing so is what gives us the strength to move forward.
Source:https://www.neonatologytoday.net/newsletters/nt-feb25.pdf
4 actions health leaders must take to show doctors they are valued
It takes more than words to show gratitude to physicians. These concrete steps can help doctors feel valued and protect against burnout.
Physician Health – By Georgia Garvey, Contributing News Writer Mar 18, 2025
Good health care leaders realize that physicians need more than free food and thank yous to thrive. Well-meaning expressions of appreciation that do not address the root cause of burnout or stress cannot alleviate physicians’ stress or stave off burnout the way that truly feeling valued can.
But it takes more than knowledge to change a work environment—it takes concrete action.
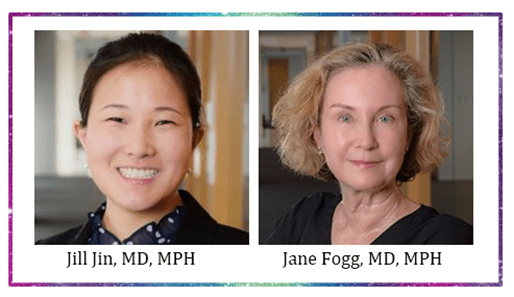
“Many leaders know the importance of teamwork and communication,” said Jill Jin, MD, MPH, an internist and senior physician adviser for professional satisfaction and practice sustainability at the AMA. “But where they kind of struggle is, how do you actually support the individual at a level that is meaningful for them?”
Dr. Jin discussed “muffin rage,” a phrase that came about as a result of a 2021 Los Angeles Times op-ed by Jillian Horton, MD, when she—deep in the throes of work-related burnout and distress—happened upon a “resident appreciation” event handing out muffins.
“Muffin rage is what we feel when there is a vast chasm between our actual needs and what another person or an institution thinks we need,” Dr. Horton wrote.
Dr. Jin spoke alongside Jane Fogg, MD, MPH, physician director of organizational transformation for the AMA, in a recent webinar on how health care organizations can make doctors feel valued, which highlighted an AMA STEPS Forward® playbook on the topic.
During the event, Drs. Jin and Fogg touched on some of the ways that health systems, organizations and leaders can take actions that will make physicians feel valued in a way that avoids muffin rage, a crucial effort with implications for physician well-being, burnout and even the quality of patient care.
Understand feeling valued, burnout link
Physician burnout rates have fallen somewhat from their historic highs during the COVID-19 public health emergency, but too many physicians continue to suffer its damaging effects. And when physicians quit or cut back their hours due to overwork and overstress, the impact is felt by patients and colleagues.
In fact, physician turnover can cost organizations anywhere from $500,000 to $1 million or more for every physician who leaves.
“Aside from it being the humane thing to do, there is also a financial benefit—a business case—for investing in your people,” Dr. Jin said.
For those looking to lessen the load on physicians, a key avenue to pursue is helping them understand the crucial role they play in their organization. Dr. Jin pointed out that research shows feeling valued correlates strongly with lower burnout rates, mentioning a 2022 study published in JAMA Health Forum that found physicians who felt valued had a 37% burnout rate, compared with 69% for those who did not.
As the leader in physician well-being, the AMA is reducing physician burnout by removing administrative burdens and providing real-world solutions to help doctors rediscover the Joy in Medicine™.
Help physicians know their worth
Once the importance of feeling valued as a key mitigator for physician burnout has been understood, Drs. Jin and Fogg said, the next step is determining what, exactly, helps physicians know and understand their worth in an organization.
Instead of superficial gestures like the one described in Dr. Horton’s piece, Dr. Jin said there are ways to effectively communicate gratitude to physicians. Those ways have much more to do with actions than with words.
Some key ways to show doctors they are valued, as described by Drs. Jin and Fogg, were to support:
- Schedule flexibility and autonomy.
- Paid time off (PTO).
- Professional development.
- Individual resilience and self-care.
- Care during and after trauma.
Make work-life balance a priority
Often it can be difficult to justify costly changes aimed at improving physicians’ work conditions, said Dr. Fogg, but overwork and lack of autonomy in matters such as scheduling result in burnout, which is even more expensive.
“Productivity is a pressure that we often feel because of falling revenues across the health care landscape,” she said. “With pressure to fill our schedules, we can lose valuable time for our continuity patients. This tension between being productive and being available to our own patients often lies in how we design and manage our schedules.”
The key, Dr. Fogg said, is giving doctors the ability to “co-design the scheduling processes with their operational team. Make sure you partner with operational leaders to have a physician voice in designing the optimal schedule system for patient access, continuity, and work life balance.”
PTO is another area of concern for organizations looking to create a culture of value, Dr. Jin said.
Health care leaders can be role models in taking time off themselves, and organizations can proactively block off vacations, celebrate time off and resist the impulse to praise working while out of the office. Physicians’ responsibilities should also be fully covered when they’re on vacation, and compensation models and appointment schedules should take PTO into account.
Support the physician as a person
To show a physician that they are more than just a cog in the machine, their professional development must be supported, recognizing their individual aspirations and passions beyond the clinical practice of medicine.
“Feeling valued means the people around you—your supervisor in particular—know who you are, what excites you and what makes you passionate” outside the confines of the clinic or hospital corridor, Dr. Fogg said. “Asking physicians about their long-term goals and offering opportunities to get involved in a variety of activities outside of clinical practice can create a stronger sense of feeling valued. Some opportunities for growth include teaching, research, process improvement initiatives, leadership, community engagement and more.
And, said Dr. Jin, while “self-care” is not a replacement for—and should not be the major focus of—systemic efforts to reduce burnout, organizations can support an individual’s resilience by helping physicians set boundaries, prioritize tasks and limit their distractions. Leadership also should provide resources for and support physicians in self-care, promote collegiality and create spaces for breaks.
Health care organizations should address both individual and collective trauma, Dr. Fogg said, by creating peer-support programs and providing confidential mental health services. They should consider developing develop suicide-prevention plans and response teams in some situations.
Additionally, the credentialling process should remove questions about mental health care so they don’t discourage physicians from seeking care if needed.
“Burnout is not a sign of mental illness, but there is a lot of overlap that happens when we are severely distressed by the way in which we’re practicing and what we’re witnessing in our practices,” she said.
For more information on this and other topics, explore the AMA STEPS Forward open-access toolkits and playbooks, which offer innovative strategies that allow physicians and their staff to thrive in the new health care environment. These resources can help you prevent burnout, create the organizational foundation for joy in medicine and improve practice efficiency.
Combat physician burnout
Event: American Conference on Physician Health (ACPH) Sept. 11-13, 2025, focusing on steps organizations can take to improve physician well-being
CME: How health systems can reduce physician burnout
Calculate: See the cost of physician burnout to your organization
Video: Latest trends in physician burnout by specialty
Playbook: Wellness-centered leadership

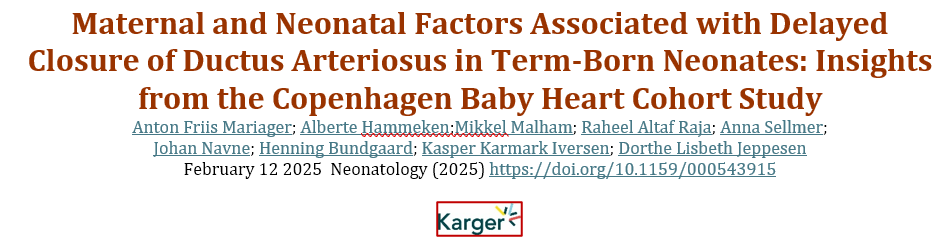
Short-Term and Long-Term Mortality Risk After Preterm Birth
Original Investigation Pediatrics November 20, 2024

Asma M. Ahmed, PhD, MD, MPH1; Sonia M. Grandi, PhD, MSc2; Eleanor Pullenayegum, PhD, MA2; et alSarah D. McDonald, MD, MSc3; Marc Beltempo, MD, MSc4; Shahirose S. Premji, RN, PhD, MScN5; Jason D. Pole, PhD, MSc6; Fabiana Bacchini, MSS7; Prakesh S. Shah, MD, MSc8; Petros Pechlivanoglou, PhD, MSc2
JAMA Netw Open. 2024;7(11):e2445871. doi:10.1001/jamanetworkopen.2024.45871
Key Points
Question Do individuals born preterm have a higher risk of short-term and long-term mortality compared with those born at term?
Findings In this cohort study of 4 998 560 births, individuals born preterm had a higher risk of mortality from birth to age 36 years, with the highest risk observed from birth through early childhood. The risk of mortality varied by gestational age at birth and was more pronounced at lower gestational ages.
Meaning The findings of this study suggest that preterm birth is associated with increased risk of death from infancy to adulthood.
Abstract
Importance Preterm birth (PTB) is a leading cause of neonatal mortality. However, evidence on mortality beyond the neonatal period is limited, especially in North America.
Objective To examine associations of PTB with all-cause and cause-specific mortality from birth through 23 to 36 years of age.
Design, Setting, and Participants This population-based matched cohort study of live births in Canada included individuals born between January 1, 1983, and December 31, 1996, and followed up until December 31, 2019. Data were analyzed from June 1, 2023, to April 30, 2024.
Exposure PTBs, between 24 and 37 weeks’ gestation (with gestational age [GA]-specific subcategories of 24 to 27 weeks, 28 to 31 weeks, 32 to 33 weeks, and 34 to 36 weeks) compared with term births (37-41 weeks’ gestation).
Main Outcomes and Measures All-cause mortality and cause-specific mortality were the main outcomes. Risk differences (RDs) and risk ratios (RRs) were estimated for all-cause mortality using log-binomial regressions and hazard ratios were estimated for cause-specific mortality using Cox proportional hazards regression models (censoring individuals who died from other causes) within prespecified age intervals (ages 0-11 months and ages 1-5, 6-12, 13-17, 18-28, and 29-36 years). Observed confounding was accounted for using coarsened exact matching on baseline characteristics.
Results Of 4 998 560 births (54.2% male), 6.9% were born preterm (with GA-specific subcategories of 0.3% born at 24-27 weeks, 0.6% at 28-31 weeks, 0.8% at 32-33 weeks, and 5.1% at 34-36 weeks). During a median of 29 years of follow-up, 72 662 individuals died (14 312 born preterm and 58 350 at term). PTB was associated with an increased risk of death in all age intervals, with the highest RDs and RRs from birth through infancy (ages 0-11 months) (RD, 2.29% [95% CI, 2.23%-2.35%]; RR, 11.61 [95% CI, 11.09-12.15]) and in early childhood (ages 1-5 years) (RD, 0.34% [95% CI, 0.31%-0.36%]; RR, 2.79 [95% CI, 2.61-2.98]) and the lowest RDs and RRs among those between ages 18 and 28 years (RD, 0.07% [95% CI, 0.04%-0.10%]; RR, 1.13 [95% CI, 1.07-1.19]). We identified increased risks of mortality associated with several causes, including respiratory, circulatory, and digestive system disorders; nervous system, endocrine, and infectious diseases; cancers; congenital malformations; and conditions originating in the perinatal period. No associations were found for external causes of deaths. Associations by GA categories suggested lower risks with higher GA.
Conclusions and Relevance The findings of this population-based matched cohort study suggest that individuals born preterm were at an increased risk of death from birth until their third and fourth decades of life, with higher risks as GA decreased. Some of these associations may have been partly due to underlying health determinants that affected PTB and mortality. These findings suggest that PTB should be recognized as a risk factor for mortality and could inform preventive strategies.
FULL STUDY


INNOVATIONS


EDITORIAL article Front. Pediatr. , 12 January 2025 Volume 13 – 2025 | https://doi.org/10.3389/fped.2025.1552262
This article is part of the Research Topic What is new on the Horizon in Neonatology? Recent Advances
Minesh Khashu1Karel Allegaert2,3,4*
- 1Department of Neonatology, University Hospitals Dorset NHS Foundation Trust, Dorset, United Kingdom
- 2Department of Development and Regeneration, KU Leuven, Leuven, Belgium
- 3Department of Pharmaceutical and Pharmacological Sciences, KU Leuven, Leuven, Belgium
- 4Department of Hospital Pharmacy, Erasmus MC, Rotterdam, Netherlands
Neonates and infants are commonly referred to as “therapeutic orphans” due to the overall scarcity of therapeutic interventions that have been developed and tailored to their needs and specific characteristics (1, 2). This is well known by care providers and researchers active in this field, but is perhaps less on the radar of authorities, funding bodies or the broader public. There is significant health inequity when comparing newborns to other age populations in terms of specific drug and device development and therapeutics (1, 2). In addition there are health inequities in the provision of neonatal care globally which require special attention in terms of improvement (3).
Bronchopulmonary dysplasia, neonatal seizures, poor growth, necrotizing enterocolitis (NEC) and short bowel, hypoxic-ischemic encephalopathy, retinopathy of prematurity (ROP), neonatal infections and sepsis hereby serve as a non-exhaustive list of “orphan conditions” in need of more equity, through adequately and urgently funded research and improvement.
The good news is that there have been increased efforts, in recent years, by researchers and regulatory bodies to focus on the provision of drugs, devices, and treatment modalities tailored for neonatal use, while further advocacy remains an obvious need (2, 4, 5). This brings perspective and explains the initiative taken to organize a focused research topic on what is on the horizon as well as recent advances.
Overview of the topics covered
We targeted emerging or new aspects related to monitoring, diagnostics and therapeutics in neonatal care for the current research topic. Fortunately, this research topic was perceived as very relevant by the research community, as 135 authors expressed their interest as contributors, resulting in 20 accepted papers. This serves as a signal of the importance to continue to work on this topic.
Post-hoc, and in a somewhat arbitrary way (because of overlap in these subcategories) these papers were subdivided by the editors into different subcategories, with focus on (1, 5 papers) perinatal biomarkers in blood and urine and how these relate to or predict outcomes, (2, 6 papers) adaptations of existing and newly emerging equipment in neonatal units, (3, 3 papers) needed advances in pharmacotherapy, (4, 3 papers) machine learning or deep learning applications in neonatal care, and finally, (5, 3 papers) underreported aspects of contemporary NICU care, with a focus on the holistic nature of care for the infant and the family.
Perinatal biomarkers in blood and urine and how these relate to or predict outcomes
Two papers focused on biomarkers related to gestational diabetes, with reflections and data on maternal and neonatal outcomes. Postnatal maternal levels of glycated albumin and hemoglobin A1c in mothers of large-for-gestational-age (LGA) informed us of the relevance of accurate diagnosis during pregnancy. This is because postpartum women without diagnosis during pregnancy had higher glycated albumin values, associated with LGA and associated complications (Železnik et al.). Interestingly and related to this paper, Yin et al. reported on a untargeted metabolomics study in women with gestational diabetes, with the recommendation of a maternal serum metabolite panel to forecast neonatal adverse outcomes (hypoglycemia and macrosomia) (Yin et al.).
Other papers focused on the use of vitamin D, acid-base and biomarkers associated with fetal growth restriction with impaired neurodevelopmental outcome. In a cohort of 217 preterm neonates, a multivariate regression analysis identified antenatal steroids as protective, and lower birth weight, duration of ventilation, sepsis and the serum 25-(OH)D vitamin as risk factors to develop ROP (Yin et al.). Musco et al. reported on a systematic review on blood biomarkers indicating risks of adverse neurodevelopmental outcome in fetal growth restricted infants (Musco et al.). While the authors retrieved some data on neuron specific enolase and S100B, the overall conclusions reflect a call for further research. Finally, an association between lactate levels in umbilical cord blood and cerebral oxygenation in preterm neonates was studied as a secondary outcome analysis (Dusleag et al.). In non-asphyxiated preterm neonates with respiratory support, lactate levels were negatively associated with cerebral and arterial oxygenation. In term neonates without respiratory support, no associations were observed.
Adaptations of existing and newly emerging equipment in our units
In a review on emerging innovations in neonatal monitoring, Krbec et al. concluded that there is an urgent, still unmet need to develop wireless, non- or minimal-contact, non-adhesive technology, capable to integrate multiple signals in a single platform, tailored to neonates (Krbec et al.). Related to this call of action, Svoboda et al. reported on their pilot experience with contactless assessment of heart rate, applying imaging photoplethysmography (Svoboda et al.). Rectal and axillary temperature monitoring on admission were compared in a cohort of preterm (n = 80, <32 weeks gestational age) by Halabi et al., reporting that rectal measurement was likely more reliable in the event of hypothermia (Halabi et al.). Ultrasound-guided measurement of anterior cerebral artery resistive index in the first week of life in 739 preterm neonates (<35 weeks) was not associated with subsequent co-morbidities on admission or during neonatal stay (asphyxia, sepsis, NEC) (Singh Gill et al.). A case series of neurally adjusted ventilatory assist to rescue pulmonary interstitial emphysema in 5 extremely low birth weight infants illustrated the potential value of this ventilatory equipment and strategy and need for further study (Chen et al.). Finally, van Rens et al. compared a conventional to a modified Seldinger technique (a dedicated micro-insertion kit) for peripherally inserted central catheter (PICC) placement, illustrating the relevance of developing “low risk, high benefit” type of medical devices, adapted to the specific needs of neonates (van Rens et al.).
Advances needed in pharmacotherapy
The currently available medicines and dosing regimens in neonatal care are limited and there is an urgent need for improvement in this domain. This was illustrated by articles on sepsis, septic shock and steroids. Inequity in provision of neonatal care across the globe ought to be a major focus of improvement. Gezahegn et al. described the outcome in neonates admitted with sepsis in Harar (Ethiopia). Low white blood cell count, desaturation, preterm birth, absence of prenatal maternal care, and chorioamnionitis were important risk factors for sepsis-related mortality (Gezahegn et al.). Addressing these prognostic factors hold the promise to act as levelers to improve outcomes. A pilot study compared noradrenaline and adrenaline as first line vasopressor for fluid-refractory sepsis shock (Garegrat et al.). Both interventions were comparable to resolve the septic shock, while the overall mortality (13/42, 30%) remained significant, highlighting the need for better diagnostic and therapeutic options. Finally, in a systematic review, outcome of postnatal systemic corticosteroids (hydrocortisone to dexamethasone) were compared as reported in randomized controlled trials (Boscarino et al.). The authors concluded that dexamethasone appeared to be somewhat more effective than hydrocortisone in improving respiratory outcomes, but with inconclusive but relevant concerns on the uncertainties on long-term neurodevelopmental outcome, again highlighting the need for better therapies for prevention and management of chronic lung disease of prematurity.
Machine learning or deep learning applications in neonatal care
Artificial intelligence is a rapidly advancing area with fast evolving clinical applications in healthcare, including in the NICU (6). It is no surprise that the current research topic also contains papers illustrating its relevance to improve our practices and outcomes. Two papers hereby focused on NEC, and a 3rd paper on prediction of significant patent ductus arteriosus (PDA). In a mini-review, Cuna et al. reports on the various pathophysiological processes underlying NEC endotypes, and how artificial intelligence holds the promise to influence further understanding and management (Cuna et al.). An approach to enhance surgical decision making in NEC is illustrated by Wu et al. Based on x-rays from 263 neonates diagnosed with NEC (94 surgical cases), a binary diagnostic tool was trained and validated, with Resnet18 as approach applied (Wu et al.). For PDA, an ultrasound-based assessment of ductus arteriosus intimal thickness in the first 24 h after birth was applied in 105 preterm neonates. A prediction model for closure on day 7 included birth weight, mechanical ventilation, left ventricular end-diastolic diameter, and PDA intimal thickness (Hu et al.). Such models can be considered to better target future study, integrated in a precision medicine approach. Use of AI and big data have the potential to significantly improve our understanding of neonatal conditions and also support neonatal researchers in asking better research questions.
Underreported aspects of contemporary NICU care, holistic care
As part of this research topic, we also accepted papers reporting on the use of music on pain management, on multisensory stimulation to improve maternal milk volume production, and parents’ experiences related to congenital cardiac surgery. All these 3 papers reflect the need for holistic care and to further integrate the perspectives of (former) patients and parents into neonatal practice.
In a systematic review, Ou et al. demonstrated that music is an effective intervention to relief procedural pain (e.g., Premature Infant Pain Profile score) in preterm neonates, as it reduced some markers of stress, and improved blood oxygen saturation (Ou et al.). Multisensory stimulation (audiovisual, or audiovisual + olfactory) compared to a control setting improved maternal milk volume production, with evidence of positive effects of both interventions, even more pronounced if both interventions are combined (Cuya et al.). Finally, a quantitative analysis of parent’s experiences with neonates admitted to NICU with a congenital heart disease reinformed us on the importance of actively focusing on parental experiences of care (Catapano et al.).
From advances in neonatal care to implementation
In our opinion, this research topic nicely illustrates the diversity in ongoing clinical research activities, that all hold the promise to improve our clinical management practices, with the overarching aim to improve neonatal outcomes. There is an urgent need to focus on the current health inequities in the provision of care to neonates (3). The trend towards a “neuro” dedicated NICU care is an illustration on how relevant progress may occur. This progress is based on improved neuromonitoring techniques (7), improved management and precision medicine in the field of anti-epileptic drugs (8), and integrating families as partners in neonatal neuro-critical care and similar improvement programs (9). The good news is that we are already experiencing a shift in the right direction. The neonatal community and all other relevant stakeholders need to work better together to improve the pace and scale of this improvement.
Source: https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2025.1552262/full

Improvement Project to Reduce Uncontrolled Pain and Improve Staff Satisfaction

Sprecher, Alicia MD; Roeloffs, Kimberly NNP; Czarnecki, Michelle L. APN; Labovsky, Kristen MD; Kissell, Anna PharmD; Hornung, Genesee MSN, RN; Uhing, Michael MD Editor(s): Dudding, Katherine PhD, RN, RNC-NIC, CNE; Nist, Marliese D. PhD, RNC, Section Editors Advances in Neonatal Care 25(1):p 18-27, February 2025. | DOI: 10.1097/ANC.0000000000001234
Abstract
Background:
Postoperative pain management in the neonatal period is an area of high variability and a source of staff dissatisfaction. Pain management is a key component of high-quality care; however, pain assessment in infants is difficult and analgesics can negatively impact the developing brain.
Purpose:
We aimed to improve postoperative pain control for infants in our neonatal intensive care unit (NICU), limit variability in the approach to pain management, and increase staff satisfaction.
Methods:
This project was completed between April 2019 and March 2022 with sustainment tracked through December 2023. Interventions took place in a 70-bed level IV NICU using quality improvement methodology. Interventions included efforts aimed at improving pain assessment as well as development and implementation of a pain management guideline. Outcome measures included frequency of uncontrolled postoperative pain and measures of staff satisfaction. Process measures included compliance with pain assessment cadence and guideline recommendations. Opioid exposure within 24 hours of surgery was included as a balancing measure.
Results:
Pain management was assessed in 811 infants: 392 prior to guideline implementation, 273 during implementation, and 146 during sustainment period. Uncontrolled postoperative pain decreased from 26% pre-implementation to 18% post implementation and into the sustainment period. Staff satisfaction improved from 67% to 83%. These improvements were associated with decreased variability in postoperative pain management and a decrease in postoperative opioid exposure.
Implications for Practice and Research:
The use of a postoperative pain management guideline can improve pain control, decrease drug regimen variability, decrease opioid exposure, and increase staff satisfaction.

Health Care Heros – Environmental Service Workers

Healing Forward: Health & Wellness
In Singapore, where skyscrapers rise and medicine meets innovation, a new kind of wellness journey is unfolding—one led by the smallest among us.
Our Womb Warriors who began life in the NICU are not just survivors—they are thrivers, growing through challenges and emerging with strength forged in the most fragile beginnings. Today, health and wellness for these preemie survivors extends far beyond the hospital walls. It means developmental follow-up, skin-to-skin care, nutrition support, and emotional well-being—not just survival, but quality of life.
Singapore’s approach is inspiring. With personalized risk assessments, neurodevelopmental care programs, and parent-empowering tools like kangaroo care, the wellness journey begins from day one. And studies now confirm what many NICU parents already knew in their hearts: the closeness, love, and presence of family are as powerful as any machine.
As our Warriors grow, their wellness becomes more than a checklist—it becomes a rhythm. Physical therapy. Play. Sensory exploration. Nourishment. Love. And for the parents walking beside them? Wellness looks like deep breaths, long walks, and the quiet courage to ask for help.
Whether your little one is a few months or a few years out of the NICU, this season is a reminder: wellness isn’t a destination—it’s a daily act of love.
Spring into Strength
Spring is a season of becoming—of blooming boldly, stretching softly toward the light, and waking up to what’s possible. For our Womb Warriors, it’s also a reminder that wellness is not about perfection—it’s about progress, presence, and power.
Whether you’re a preemie kid discovering new abilities, a teen navigating your story, or an adult survivor reclaiming your narrative, this season invites you to grow on your terms. Your early beginnings may have been fragile—but your spirit is anything but.
Health and wellness don’t have to look the same for everyone. What matters most is listening to your body, honoring your journey, and celebrating how far you’ve come.
🌸 For Kids
- Make movement magical—build obstacle courses, splash in puddles, or stretch like your favorite animal.
- Explore foods that help you grow strong: yogurt parfaits, rainbow fruit plates, or protein-packed pancakes.
- Practice deep breathing with bubbles or belly-breathing “dragon breaths.”
🌱 For Teens
- Journal your thoughts under a tree or start a mood-boosting playlist for mental clarity.
- Try out yoga, trail walks, or a new sport—your strength isn’t defined by speed, but by showing up.
- Fuel yourself with purpose: balanced snacks, hydration, and sleep that heals.
🌞 For Adults
- Redefine strength: maybe it’s finishing a workout, setting boundaries, or resting when you need to.
- Revisit your NICU beginnings—use them to empower your healthcare choices and connect with your past.
- Create a spring ritual: a morning stretch, a quiet walk, or a personal mantra. Wellness isn’t trendy—it’s transformative.
In Singapore, hospitals are leading the way in early screenings and personalized care to help preemies not just survive, but thrive. That same spirit of innovation and renewal lives in each of us.
So here’s to you—this spring, let’s grow wildly. Heal gently. Thrive loudly.
Because once a Neonatal Womb Warrior, always a Warrior—and you are in full bloom.
The Path to Wellness | Alysha Aziz | TEDxHolyTrinitySchool

Wellness is a journey. In this insightful talk, learn about the PATH model: Perception, Analysis, Trial and Error, and Habits, as a framework for achieving personal well-being. This talk empowers audiences to embrace the process and find a path to a healthier, more fulfilling life. Hi everyone, I’m Alysha! I am a student in grade 11 and I’m one of the speakers for TEDEd’s Empowerment event. Having been part of the club since grade 9 and now as president, I’m really excited to share my talk with everyone! I’ll be talking about wellness and taking autonomy over your own mental health. I’m super excited that this is our first charitable event and can’t wait to see you all there!
10-minute guided meditation for kids 🧘 mindfulness for kids 🕊 Bye Bye Worry Balloons🎈 Worry-Free 💛

Relax, breathe, and feel calm with this simple meditation for kids. In this guided meditation for kids, we’ll say ‘bye-bye’ to worries and hello to happy thoughts. ☀️🎈



Would You Rather? Spring Edition! | Fun Fitness For Kids | This or That | Spring Workout | GoNoodle

Mr. Hassell’s Brain Breaks
Exercise your body and mind with this Spring themed brain break! In this fun and engaging workout video, we play a game of “Would You Rather” by picking our favorite Spring choices and performing exercises!! Perfect for a PE warmup, classroom brain break and at home workout!

Written by published children’s author, Jennifer Marino Walters, “Surprising Spring” tells the simple story of the beauty that Spring brings and its many flowering surprises.
[OFW] WAVEHOUSE Sentosa | Surfing in Singapore

5 years ago Renan El Viajero
Wave House Sentosa located on the sandy beaches of Sentosa is Asia’s only installation in an archipelago of global Wave Houses that stretches from Durban in South Africa, San Diego in California, Santiago in Chile, and Mallorca in Spain. Singapore has long been a crossroads for surfers seeking the perfect waves at beaches around Southeast Asia, however the island itself lacks the giant waves which surfers long for. With its opening, Wave House Sentosa puts Singapore on the global surfer destination map with its perfect and world famous 10′ FlowBarrel wave.