Malaysia is a country in Southeast Asia. A federal constitutional monarchy, it consists of 13 states and three federal territories, separated by the South China Sea into two regions: Peninsular Malaysia and Borneo‘s East Malaysia. Peninsular Malaysia shares a land and maritime border with Thailand and maritime borders with Singapore, Vietnam, and Indonesia. East Malaysia shares land borders with Brunei and Indonesia, as well as a maritime border with the Philippines and Vietnam. Kuala Lumpur is the national capital, the country’s largest city, and the seat of the legislative branch of the federal government. Putrajaya is the administrative centre, which represents the seat of both the executive branch (the Cabinet, federal ministries, and federal agencies) and the judicial branch of the federal government. With a population of over 34 million, the country is the world’s 43rd-most populous country. Malaysia is tropical and is one of 17 megadiverse countries; it is home to numerous endemic species. Tanjung Piai in the Malaysian state of Johor is the southernmost point of continental Eurasia.
Healthcare in Malaysia is under the purview of the Ministry of Health of the Government of Malaysia. Malaysia generally has an efficient and widespread system of health care, operating a two-tier health care system consisting of both a government-run public universal healthcare system along with private healthcare providers. Within the public universal healthcare system, specialist services are either free or have low user fees for procedures (however, appliances are fully self-funded out of pocket by the patient, even within the public healthcare system); as such the public healthcare system suffers from high demand, routine congestion, long wait lists, chronic widespread delays along with persistent shortages in healthcare personnel, medical equipment and healthcare supplies.
Therefore, private healthcare providers play a pivotal role in providing specialist consultants and general practitioner (GP) services to the Malaysian population; the private healthcare providers complements or supplants the public healthcare system in terms of availability, types of treatments provided and types of materials used.
Source: https://en.wikipedia.org/wiki/Malaysia
- GLOBAL PRETERM BIRTH RATES – Malaysia
- Estimated # of preterm births: 12.3 per 100 live births/Global Average: 10.6
- Source- WHO Preterm Birth Rate (Per 100 Live Births)
- World Population Review
- WHO Country Consultation of Low and Preterm Birth Weight

COMMUNITY


Introduction
Reducing neonatal deaths in premature infants in low- and middle-income countries is key to reducing global neonatal mortality. International neonatal networks, along with patient registries of premature infants, have contributed to improving the quality of neonatal care; however, the involvement of low-to-middle-income countries was limited. This project aims to form an international collaboration among neonatal networks in Asia (AsianNeo), including low-, middle- and high-income countries (or regions). Specifically, it aims to determine outcomes in sick newborn infants, especially very low birth weight (VLBW) infants or very preterm infants, with a view to improving the quality of care for such infants. Methods and analysis Currently, AsianNeo comprises nine neonatal networks from Indonesia, Japan, Malaysia, Philippines, Singapore, South Korea, Sri Lanka, Taiwan and Thailand. AsianNeo will undertake the following four studies: (1) institutional questionnaire surveys investigating neonatal intensive care unit resources and the clinical management of sick newborn infants, with a focus on VLBW infants (nine countries/regions); (2) a retrospective cohort study to describe and compare the outcomes of VLBW infants among Asian countries and regions (four countries/regions); (3) a prospective cohort study to develop the AsianNeo registry of VLBW infants (six countries/regions); and (4) implementation and evaluation of educational and quality improvement projects in AsianNeo countries and regions (nine countries/regions). Ethics and dissemination The study protocol was approved by the Research Ethics Board of the National Center for Child Health and Development, Tokyo, Japan (reference number 2020–244, 2022–156). The study findings will be disseminated through educational programmes, quality improvement activities, conference presentations and medical journal publications.
ABSTRACT
Introduction Reducing neonatal deaths in premature infants in low- and middle- income countries is key to reducing global neonatal mortality. International neonatal networks, along with patient registries of premature infants, have contributed to improving the quality of neonatal care; however, the involvement of low- to- middle- income countries was limited. This project aims to form an international collaboration among neonatal networks in Asia (AsianNeo), including low-, middle- and high- income countries (or regions). Specically, it aims to determine outcomes in sick newborn infants, especially very low birth weight (VLBW) infants or very preterm infants, with a view to improving the quality of care for such infants. Methods and analysis Currently, AsianNeo comprises nine neonatal networks from Indonesia, Japan, Malaysia, Philippines, Singapore, South Korea, Sri Lanka, Taiwan and Thailand. AsianNeo will undertake the following four studies: (1) institutional questionnaire surveys investigating neonatal intensive care unit resources and the clinical management of sick newborn infants, with a focus on VLBW infants (nine countries/regions); (2) a retrospective cohort study to describe and compare the outcomes of VLBW infants among Asian countries and regions (four countries/regions); (3) a prospective cohort study to develop the AsianNeo registry of VLBW infants (six countries/regions); and (4) implementation and evaluation of educational and quality improvement projects in AsianNeo countries and regions (nine countries/regions).Ethics and dissemination The study protocol was
approved by the Research Ethics Board of the National Center for Child Health and Development, Tokyo, Japan (reference number 2020–244, 2022–156). The study findings will be disseminated through educational programmes, quality improvement activities, conference presentations and medical journal publications.

A Critical Need For Breastmilk Collection Centres For High-risk Premature Babies
Authors: Wan Mazwati Wan Yusoff, International Islamic University Malaysia Mashitah Zainol Abidin
Abstract
Premature babies are very vulnerable and exposed to various life-threatening diseases. World Health Organization reported that many premature babies were saved from morbidity and mortality when they were fed with breastmilk starting from within the first hour after their birth. The rate of premature birth in Malaysia has increased exponentially since 2018—more than 20 percent premature births. Therefore, hospitals should have enough supplies of breastmilk to save the lives of the precious premature babies. However, only one hospital in Malaysia provides supplies of breastmilk on demand. This study employed philosophical method to argue for the establishment of breastmilk collection centre. It examined the concept of maqāṣid al-sharīʿah to justify the proposal of the establishment of breastmilk collection centres in hospitals throughout Malaysia to save the lives, intellects, and progenies of the at-risk premature babies. The primary issues resulting from breastmilk sharing according to Islamic perspective were examined and practical steps were proposed to rectify them. The steps involved obtaining signed consent from wet nurse and her husband; screening of wet nurse’s health and personality characteristics; screening of the breastmilk by the milk collection centre; obtaining signed consent from the premature baby’s parents; feeding breastmilk to the premature baby with the consent of witnesses; meeting between wet nurse and her family and the baby’s parents and family; and completing wet nursing document to be given to the newly formed milk kinship family.
Source:https://doi.org/10.31436/alburhn.v7i2.310
Tuni Sundatang – Diwato (Live)



Building Trusting Teams – A Pathway to Organizational Excellence
Rody Azar, MHA, RRT-NPS

Introduction:
Trust is an essential element of effective teamwork. It fosters an environment where team members feel safe communicating openly, sharing ideas, and collaborating towards common goals. Without trust, relationships become strained, communication breaks down, and organizational performance suffers. According to a study by Gallup, organizations with high employee engagement, which is closely related to trust, report 21% higher profitability (Gallup, 2020). This paper explores trust in teams, examining how it can be fostered and its profound impact on organizational success.
The Importance of Trust in Teams:
1. Enhanced Communication: Trust creates a safe space where team members can share their thoughts and feelings without fear of judgment. This openness leads to improved communication, enabling teams to function more effectively. When team members trust each other, they are more likely to engage in candid discussions, ask for feedback, and share constructive criticism. This process encourages continuous improvement and innovation.
2. Improved Collaboration: Teams characterized by trust collaborate more seamlessly. Trust encourages team members to share resources, support one another, and seek each other’s abilities. This collaborative spirit leads to better problem-solving and decision-making, as individuals are more willing to listen to diverse perspectives.
3. Increased Engagement: Trust enhances commitment and engagement within teams. Employees who feel trusted and valued are more likely to invest their time, energy, and creativity into their work. This higher level of engagement results in better performance and productivity, as engaged employees are motivated to achieve team goals.
4. Effective Conflict Resolution: Conflict is a natural occurrence in any team dynamic. However, team members are more likely to address conflicts directly and constructively in a trusting environment, allowing them to express their disagreements without fear of damaging relationships. This approach leads to more effective and quicker resolutions, which helps support a positive team atmosphere.
5. Greater Accountability: When trust exists within teams, members are more likely to hold themselves and each other accountable for their roles and responsibilities. Trusting teams create a culture of accountability where individuals take ownership of their work, leading to higher standards and better performance.
Characteristics of Trusting Teams:
- Open Communication: Team members communicate transparently and honestly, fostering a culture of openness and inclusivity.
- Mutual Respect: Trusting teams recognize and appreciate each other’s strengths, value
diversity, and promote an inclusive environment.
- Shared Goals: All team members are aligned with common goals, reinforcing collaboration
and commitment.
- Empathy and Support: Team members show care and understanding for one another,
creating a supportive atmosphere that encourages sharing and vulnerability.
- Reliability: Trusting teams foster a sense of reliability, where members can depend on each
other to fulfill commitments and responsibilities.
Strategies for Building Trusting Teams:
Building trust is an ongoing process requiring intentional effort from leaders and team members. Below are strategies to cultivate trust in teams:
1. Lead by Example: Leaders play a crucial role in shaping team dynamics. By showing trustworthy behaviors, such as honesty, integrity, and accountability, leaders set the standard for others to follow. Vulnerability in leadership (e.g., admitting mistakes and seeking feedback) can also strengthen trust within the team.
2. Foster Open Communication: Encourage team members to openly share their thoughts, ideas, and feedback. Create an environment where communication is valued, and actively listen to team members. Regular check-ins, team meetings, and one-on-one discussions can help open dialogue and build trust.
3. Encourage Collaboration: Design opportunities for team collaboration across various projects. Creating diverse project teams allows members to collaborate, share knowledge, and build relationships. Activities such as brainstorming sessions or team-building exercises can strengthen interpersonal connections.
4. Recognition and Appreciation: Regularly acknowledge and celebrate the contributions of team members. Recognition fosters an environment of appreciation, reinforcing the value of individual efforts. Simple gestures such as expressing gratitude during meetings or highlighting achievements can significantly boost trust within the team.
5. Create a Safe Environment for Risk-Taking: Encourage team members to take thoughtful risks and innovate without fear of negative consequences. Providing autonomy and support for innovative ideas helps build trust, as team members feel empowered and valued for their contributions.
6. Establish Clear Roles and Expectations: Clarify the roles and responsibilities of each team member. When individuals understand their specific roles and expectations, it fosters accountability and reduces uncertainty. Clear roles create a sense of security, allowing team members to trust that everyone is working towards the same goals and can depend on one another to fulfill their responsibilities.
7. Promote Team-building Activities: Engaging in in-person or virtual team-building activities can significantly strengthen team members’ interpersonal relationships. These activities should encourage collaboration, promote understanding, and foster positive interactions outside of day-to-day work. Such experiences can help individuals develop personal connections, creating a more profound sense of trust.
8. Provide Opportunities for Professional Development: Encouraging continuous learning and professional growth shows team members that the organization values their development. Offering training, workshops, and mentorship opportunities improves individual skills and reinforces trust, as team members see that their organization is invested in their success.
9. Practice Transparency: Transparency is a key part of trust. Leaders should share relevant information about the organization’s goals, decision-making processes, and performance metrics with their teams. When team members are informed about what is happening within the organization, they feel more involved and valued, strengthening trust.
10. Encourage Feedback: Creating a culture where feedback is valued encourages trust among team members. Implementing regular feedback mechanisms—such as one-on-one check-ins and anonymous surveys—allows team members to express their thoughts and concerns. Moreover, showing that feedback is taken seriously and leads to action, reinforcing the notion that everyone’s input is valuable.
The Impact of Trusting Teams on Organizational Success:
The presence of trusting teams can lead to transformative outcomes in an organization:
1. Higher Performance and Productivity: Organizations with trusting teams have been shown to achieve higher performance levels. Trust enhances collaboration and reduces time spent on conflicts, resulting in teams completing projects more efficiently and effectively.
2. Improved Employee Well-being: A trusting environment improves employee morale and job satisfaction. Employees who feel trusted are less likely to experience stress and burnout, resulting in a healthier workforce with higher retention rates.
3. Greater Innovation: Trust allows teams to embrace creative solutions and explore innovative ideas without fear of failure. This environment fosters innovation as team members confidently share their insights and experiment with novel approaches to work.
4. Stronger Organizational Culture: A trust-based culture promotes a sense of belonging and shared purpose. Employees are more likely to feel aligned with the organization’s mission and values, which enhances overall engagement and loyalty.
5. Resilience to Change: Organizations characterized by trust navigate change effectively. Trusting teams adapt more readily to new initiatives and challenges as members communicate openly and support one another during transitions.
Conclusion:
Building trusting teams is not just a desirable outcome but essential for organizational success. Trust enhances communication, collaboration, and accountability while fostering a positive work environment. Organizations can cultivate a culture where teams thrive by implementing strategies that promote trust-building, such as leading by example, fostering open communication, and providing opportunities for development.
Leaders must recognize that trust is a pivotal part of team dynamics and should actively work to nurture it. The benefits of trusting teams extend beyond individual relationships; they affect organizational performance, employee satisfaction, and innovation. As organizations navigate complexities in the modern workplace, prioritizing trust will be paramount for achieving sustainable success.
By building trust within teams, organizations can strengthen their foundation and position themselves for future success. As shown throughout this paper, trusting teams are the cornerstone of an effective and resilient organizational culture.

HEALTHCARE PARTNERS

SOS Préma” empowers healthcare providers with parental insights at 15th annual training days
Posted on 13 November 2024

10-11 October saw 340 healthcare professionals gather in France for SOS Préma’s 15th annual training days, a pivotal event offering an empathetic view into the realities faced by families of preterm infants.
Each year, “SOS Préma”, our valued partner in France, hosts training sessions to deepen the understanding of healthcare providers around the unique challenges encountered by preterm infants and their families. Established in 2011, these events now bring together hundreds of healthcare professionals, all committed to improving neonatal care. The 15th edition, held on 10 and 11 October, attracted over 340 participants, all united in their commitment to advancing care for these vulnerable newborns.
The event revolved around four main themes, each addressing key aspects of neonatal care:
- Zero Separation: Couplet care from birth
Promoting uninterrupted contact between newborns and parents from birth through hospitalisation, ensuring that critical family bonds are supported from the earliest moments.
- Supporting late preterm babies
Exploring breastfeeding and Kangaroo Mother Care as essential practices to help these infants grow and thrive, reinforcing the importance of holistic approaches.
- Navigating difficult moments with Zero Separation
Addressing challenging periods during hospitalisation and equipping professionals with strategies to provide consistent infant- and family-centred support.
- Observing newborns with family involvement
Encouraging healthcare providers to incorporate parents as essential members of the caregiving team, fostering a collaborative environment for a more comprehensive understanding of each infant’s needs.
SOS Préma’s Charter for the Hospitalised Newborn, a cornerstone of these discussions, continues to influence practices by promoting humane and inclusive neonatal care. Parental testimonials were central to the event, with families sharing their firsthand experiences, followed by scientific insights, ensuring that every healthcare professional gains practical tools and empathetic perspectives.
Source:https://www.efcni.org/news/sos-prema-15th-annual-training-days/

Global Health Education for Medical Students and Residents
Before you complete your family medicine residency or even finish medical school, there are ways that you can begin to nurture your interest in global health and prepare for service you may want to provide in the future. Here’s how to get started.

For Medical Students
Integrating Global Health into Your Medical Education
Seeking out as many global health-related opportunities as possible during your time in medical school can help you clarify your vision for working and serving globally, and cultivate relationships through which you may contribute and be mentored.
Opportunities you should consider include the following:
- Develop knowledge, skills, and understanding that will prepare you to work effectively in a global context.
- Participate in your medical school’s global health track (if available). Getting involved in a global health track during medical school is strongly recommended. A well-designed global health track provides necessary background information and skills. It can also facilitate networking, which is key to short-term international rotations, and help you find individual mentors who can help guide your decisions.
- Participate in activities that focus on local underserved populations and/or global health (e.g., journal clubs, courses, electives, service projects, service-oriented student groups, research)
- Volunteer for a not-for-credit experience serving an underserved population during your M1-M2 summer, or during a fall, spring, or holiday break
- Do a research project or a scholarly/capstone project focused on a population outside of the United States or an underserved population in the United States
- Advocate for the value and relevance of global health curriculum and experiences to your medical school. For example, you could provide the dean and the family medicine chair with information about the value of global health experiences and curriculum for your development as a physician and the school’s achievement of its mission.
- Get involved in your medical school’s global health-related student interest group (if available)
- Lead your Family Medicine Interest Group (FMIG) in serving a local underserved population; you might want to partner with other student groups to develop a sustainable program.
- Engage with your medical school’s office/center/institute for global health (if available)
- Build a foundation for long-term collaboration by developing relationships with people and organizations involved in global health; tap into your medical school’s existing partnerships and relationships, if available.
- Aim for a longitudinal experience throughout medical school
- Use the AAFP global health resources and network
- Cultivate relationships with mentors who can guide your development of abilities and attributes you will need to pursue your interest in global health
Finding a Family Medicine Mentor in Global Health
Finding a mentor can be a huge help in navigating the many questions you’ll have as you become more aware of global health needs and opportunities. Here are some suggestions on finding a mentor for yourself.
- Attend the American Academy of Family Physicians’ (AAFP’s) annual Global Health Summit. This conference is specifically designed to facilitate networking and is attended by experienced global health workers who have long-term involvement in specific cultures and countries.
- Try personal networking. Ask colleagues, friends, and family members whether they know anyone who works in global health, and contact potential leads with emails and phone calls. The more connections you make, the greater your chances of identifying one or more physicians who would be an appropriate mentor.
- Look for someone who is doing the type of global health work you would like to do or working in a region that interests you. Contact that person to share your background and aspirations.
- Reach out to presenters at meetings or to authors of articles/books of interest. Ask for advice or offer to help someone with a project. People working in global health often find it rewarding to advise and work with those who are exploring an interest in global health.
Preparing for Global Health During Family Medicine Residency
An accredited family medicine residency program provides ideal preparation for short- and long-term global health work. Family physicians are specifically trained to provide the care that is most needed in the developing world—care for patients of all ages that is comprehensive, continuous, integrated, community oriented, and team based. If you are seriously considering global health work, you should select a residency program that offers:
- Support and guidance for interest in global health
- A patient population that includes a variety of ethnicities, cultures, and languages so that you can become proficient in the use of translators and cultural interpreters
- A robust global health track that provides additional training in tropical and poverty-related diseases, advanced procedural skills, and cultural competence; the opportunity to participate in global rotations; and a network of international contacts. Getting involved in a global health track during residency is strongly recommended.
Once you have started your family medicine residency, the following steps can help you prepare for global health work:
- Develop competence in a team-based approach to medical care; attention to the whole family; preventive and community-oriented care; and provision of continuous care to a defined population
- Develop specific interventional skills (e.g., procedures that are commonly performed at the primary care level in developing countries, such as repair of complex lacerations and interpretation of diagnostic ultrasound examination)
- Find a faculty mentor or advisor who is involved in global health work and can help you prepare yourself and your family. A faculty mentor might also be able to help you use your global health experience to develop a scholarly presentation or paper.
- Complete additional (e.g., fellowship-based) training in advanced obstetrics and gynecology (including c-section) or disaster relief. Although a fellowship is not essential for an effective contribution to global health, it can be helpful.
Family Medicine Residency Programs with International Rotations
The AAFP Center for Global Health Initiatives has compiled a director of family medicine residency programs that include international rotations. Search our free database to explore these programs.
INTERNATIONAL ROTATIONS DIRECTORY
Ways to Integrate Global Health into Your Residency Experience
Find your passion within global health.
If you want to make a lasting impact in a global health setting, it is important to find your niche within the vast array of family medicine global health opportunities. It may take time and several different experiences to discover and develop your passion. You may find that you are drawn to a certain country, culture, language area, or area of need (e.g., maternal and child health, social determinants of health, disaster relief, policy, noncommunicable diseases). Be open to the many types of experiences that are available. If possible, explore them before you are committed to long-term employment.
There may be faculty mentors in your residency program who have experience in certain areas of global health. The AAFP offers a directory of global health opportunities.
Attending conferences such as the AAFP Global Health Summit also will expose you to many different areas of interest within global health.
Form partnerships.
Once you find your passion, partnering with individuals and organizations that share your enthusiasm will further your interest and help you have a lasting, sustainable impact. Cultivate relationships by staying connected with particular organizations or international communities. If you travel, try to return to the same area so you can deepen your commitment to that population. Partnerships and connections will help you integrate global health fully into your career, and expand your capabilities in sustainable global health efforts.
Connect with others.
There is significant interest in global health among family medicine residents in the United States and abroad. The World Organization of Family Doctors (Wonca) Young Doctors’ Movements (YDMs) around the world connect passionate residents and young physicians in conversations about family medicine in global health.
- The Polaris Movement for New and Future Family Physicians in North America is a YDM launced in 2014 that provides an international platform for medical students, residents, and new family physicians. Connect on their Facebook page.
- Another initiative of the Wonca YDMs is Family Medicine 360°, an exchange program for family medicine residents during their elective months. These four-week exchanges allow participants to travel to a country of interest and experience primary health care delivery in that setting.
Consider completing a Master of Public Health (MPH) degree.
Proficiency in public health is becoming increasingly important in the global health arena, especially if you want to make lasting impact on prevention and social determinants of health. Some residency programs and fellowship programs pay for pursuit of an MPH while in training. Find out if your residency program is among them.
Explore fellowships in global health.
It is becoming easier to find residency programs that offer a family medicine global health fellowship; however, there are currently more global health fellowships in emergency medicine (EM) and internal medicine (IM) than in family medicine. If this is the case at your residency program, talk with the fellowship program to find out whether these fellowships can be adapted to family medicine.
Explore electives in global health.
Many residencies already have global health electives or tracks in place. If your residency does not offer these, consider creating your own global health elective in your area of interest. Most residency programs will accept your ideas for an elective, especially if you already have a relationship with the organization with which you will be working.
If you are unable to travel due to time or financial constraints, pursue or create electives locally that encompass global health ideals. Working with underserved or marginalized populations in your own community can create lasting positive changes. Remember, global health is not just international health; it includes efforts in your own backyard as well!
Source: https://www.aafp.org/family-physician/patient-care/global-health/education.html

Kristen Leeman, MD
Female leadership in neonatology: The value of mentorship
Posted on March 21, 2023 by Nancy Fliesler | Our Community, People
While the majority of neonatologists are women, women make up a far smaller proportion of neonatologists in leadership positions. A recent national survey led by Kristen Leeman, MD, in the Division of Newborn Medicine at Boston Children’s and Lindsay Johnston, MD, at Yale, finds that many female neonatologists face roadblocks to career development. They often miss out on speaking engagements, career guidance, additional training, networking opportunities, and above all, mentors.
To learn more about their needs, Leeman and her colleagues contacted nearly 4,000 female neonatologists from the AAP-affiliated Women in Neonatology group and a Facebook group for female neonatologists. They received 451 survey responses, revealing several additional challenges:
- gender-based salary discrepancies, reported by 49 percent of respondents
- delayed promotion (37 percent)
- harassment by colleagues (31 percent), trainees (8 percent), staff (24 percent), and patient families (32 percent)
- lack of an established mentor (61 percent).
Female neonatologists also tend to struggle more than their male counterparts with work/life balance issues, Leeman notes, making it hard to advance. “Women commented on child care stress and burnout,” she says. “The supports are not there at vulnerable times in their careers. It’s a leaky pipeline.”
Building a mentoring program for female neonatologists
Leeman and Johnston decided to address what they see as the key missing ingredient — mentors.
“Both of us have had the benefit of superb mentorship, which has been integral to our careers,” says Leeman. “We wanted to offer an opportunity for all women across the U.S. to have access to female role models to help mentor them through different elements of their careers.”
With colleagues across the country, they created the National Women in Neonatology Mentorship Program. Bringing together senior, mid-career, and junior neonatologists, the year-long pilot program, which concludes in August, has three goals:
- to provide resources to facilitate career advancement and professional and personal satisfaction
- to identify strategies to help female neonatologists gain appropriate compensation, promotions, and professional recognition
- to foster a feeling of community.
In virtual and in-person meetings, the program’s 250-plus participants read and discuss materials, hear speakers, share their thoughts and experiences, network, offer mutual encouragement, and consult with mentors. The program has various subgroups, including groups for women practicing in community NICUs, groups for specific interests like global health or lab research, and groups for women from backgrounds that tend to be underrepresented in medicine.
Neonatology mentorship at Boston Children’s: Balancing medicine, research, and family
Patricia Davenport, MD, and Martha Sola-Visner, MD, neonatologists at Boston Children’s, illustrate the value of mentorship. As a junior faculty member, Davenport found herself juggling her clinical, research, and family responsibilities. In addition to caring for patients in the NICU, she joined Sola-Visner’s lab to conduct research on neonatal platelet transfusions. Sola-Visner quickly became a mentor.
“Martha’s mentorship has been crucial to me,” Davenport says. “She values her patients, her research, and her family. Holding those three things equally in your hands is really important. I had never done basic science before and needed a lot of mentoring, not just at the bench but also writing and presenting.”
Whether it’s an unfortunate patient outcome, an experiment that didn’t work, or a family emergency, Sola-Visner has been a vital support and sounding board. And the benefits of mentorship flow in both directions.
“I’m established now, and at this stage in my career, seeing other people progress and move forward is the most rewarding part of what I do,” says Sola-Visner. “Making sure that the people who I’ve mentored are succeeding becomes more and more important over time. I get great joy to see that.”
Davenport is also an enthusiastic participant in the national pilot mentorship program, where she is part of a subgroup on basic science.
“We talk about funding difficulties, how to organize a lab, wellness, how to care for yourself,” she says. “There’s a real sense of community across the nation. You’re always asking, ‘am I good enough?’ and it’s nice to hear other women having the same thoughts and feelings of ‘imposter syndrome.’ But we’re all doing good work.”
Source: https://answers.childrenshospital.org/mentorship-neonatology/

PREEMIE FAMILY PARTNERS

Physical Activity During Pregnancy and Preterm Birth Among Women With Gestational Diabetes
Wanglong Gou, PhD1,2,3; Congmei Xiao, PhD1,2; Xinxiu Liang, PhD1,2; et alZelei Miao, PhD1,2,3; Meiqi Shi, MS4; Yingying Wu, MS4; Sha Lu, PhD4; Xuhong Wang, MS4; Yuanqing Fu, PhD1,2; Wensheng Hu, PhD5,6; Ju-Sheng Zheng, PhD1,2,3,7
Key Points Original Investigation Public Health December 19, 2024

Question Is physical activity during pregnancy associated with preterm birth among women with gestational diabetes (GD)?
Findings In this cohort study of 1427 pregnant women with GD, accelerometer-derived moderate-to-vigorous intensity physical activity (MVPA) demonstrated an inverse association with preterm birth. The dose-response curve for MVPA in relation to the risk of preterm birth exhibited an L-shaped pattern, with a steady decline in preterm birth rate up to approximately 74 minutes per day.
Meaning These findings provide key evidence for the health benefits of MVPA during pregnancy and lay the foundation for establishing physical activity guidelines for pregnant women with GD.
Abstract
Importance Physical activity, as a modifiable factor, emerges as a primary intervention strategy for the prevention and management of gestational diabetes (GD). Among women with GD, the association of physical activity during pregnancy with preterm birth remains unclear.
Objective To examine the association of accelerometer-derived physical activity metrics and patterns with preterm birth among women with GD.
Design, Setting, and Participants This prospective cohort study recruited pregnant women with GD in Hangzhou, China, from August 2019 to August 2023 as part of the Westlake Precision Birth Cohort study. Statistical analysis was performed between August and November 2023.
Exposures Wearable accelerometer–derived physical activity metrics and patterns. Measurements of physical activity via wearable accelerometer were performed at a median (IQR) of 25.4 (24.6-26.6) weeks’ gestation.
Main Outcomes and Measures Preterm birth was determined through the examination of delivery records. Incident preterm birth was defined as the delivery of infants before completing 37 weeks of gestation.
Results Among the 1427 women meeting the inclusion criteria, the mean (SD) age was 31.3 (3.8) years, and there were 80 cases of preterm birth. An increase in moderate-to-vigorous intensity physical activity (MVPA) and the fraction of physical activity energy expenditure derived from MVPA exhibited an inverse association with preterm birth, with an odds ratio per 30 minutes of 0.64 (95% CI, 0.42-0.98) and an odds ratio per SD of 0.69 (95% CI, 0.55-0.88). In the dose-response analysis, there was a progressive decrease in the odds of preterm birth with increasing duration of MVPA per day, reaching a plateau at approximately 74 minutes per day. Furthermore, the findings indicated that active MVPA (MVPA ≥30 minutes per day), whether it was concentrated into a few days or followed a more regular pattern, had similar beneficial association with preterm birth.
Conclusions and Relevance In this prospective cohort study, MVPA during pregnancy exhibited an inverse association with preterm birth among women with GD. Concentrated physical activity was associated with similar benefits in reducing preterm birth risk as regular physical activity.
Source: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2828262
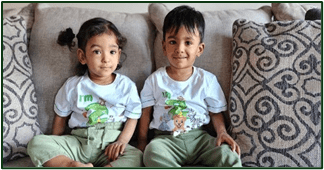
The world’s most premature twins turn two!
Mount Sinai Hospital Sinai Health March 21, 2024
Two years ago, Adiah and Adrial Nadarajah defied the odds when they were born at just 22 weeks at Mount Sinai Hospital.
The twins, who share the Guinness World Records for the youngest and lightest premature babies born, recently celebrated their second birthday, and we caught up with the family to find out how they’re doing.
Things certainly are much different in the Nadarajah household these days. “The first year of their lives was spent constantly tending to their medical needs,” reflects Shakina. And today, as the twins’ mother puts it, the family is now in the phase of “full throttle toddler parenting.”
“In the first year, the twins didn’t have much recognition of each other, so it’s beautiful to see how close they are becoming,” says Shakina. “Adrial is very affectionate and is always trying to hug his sister. He has started saying a few words too.” Some of which include: banana, potato, purple, car and of course – mama and papa.
Adiah is “the bossy one,” calling all of the shots when it comes to play time. She loves reading books, and given that both of her parents play the piano, Adiah has been naturally drawn to it.
“She is mesmerized by the piano and enjoys watching us play on it, or playing it herself,” says Shakina. “That is how she spends quality time with her dad, Kevin.”
The younger twin, Adrial was on oxygen for a period of time following a re-hospitalization after their discharge from the NICU, but went off it shortly after the twins’ first birthday. And while checking oxygen tanks and figuring out wiring across the house were not what they envisioned for their first year of parenthood, these add to their unique story of parenthood and to the twins’ story of resilience.
The twins continue to attend standard follow up appointments at Mount Sinai Hospital’s neonatal follow-up clinic, which provides families with developmental assessments for their infant(s) who received care in the NICU, and also counselling for early intervention, depending on the needs of children. The detailed assessment of a baby’s growth, feeding and development includes movement patterns, speech, play skills and problem-solving abilities, and guides families in supporting activities to enhance their development to the full potential.
“Infants who spend an extended period of time in the NICU can face long-term challenges, which is why it is important to continuously monitor these children to identify any challenges they may face as early as possible,” says Dr. Prakesh Shah, Paediatrician-in-Chief at Sinai Health. “This allows us to proactively provide optimal support, planning and timely therapy referrals for families.”
The twins were referred to different specialists, including a speech therapist, physiotherapist and an occupational therapist, and continue to get support on an ongoing basis.
“This family is a living example of what hope can do,” says Dr. Shah. “The family continuously advocated for their babies and persevered and now the twins are two years old, defying many odds.”
Although so much has changed for the Nadarajah family over the past two years, Shakina shares that “not a single day goes by” that they don’t think about the Mount Sinai Hospital NICU.
“It holds such a special place in our hearts, and was where we spent the first half year of our babies’ lives. It was our everything – our whole world. And it was amazing to have the support we received from the hospital, especially in the first year.”
Source:https://www.sinaihealth.ca/news/the-worlds-most-premature-twins-turn-two

Peek A Boo ICU Preemie
The first app of its kind to offer information SPECIFIC to the weekly growth and development of the premature baby.”
“A comprehensive guide for parents of premature babies that helps to reshape the NICU experience. Providing and educational and empowering platform to document, record, and celebrate their preemie’s story.”
“The Peekaboo ICU PREEMIE App is inspiring parents and making an impactful difference for NICU families.”


INNOVATIONS

Advancements in Neonatal Technology: What’s New in 2024?
Jun 29, 2024
The realm of neonatal care has always been a critical aspect of medical science. The delicate nature of newborns, especially preterm infants, necessitates constant innovation and improvement in technology.
As we advance through 2024, several groundbreaking developments are revolutionizing neonatal care, ensuring better survival rates and improved health outcomes for infants. In this blog, we will delve deeper into the significant advancements in neonatal technology that are shaping the landscape this year.
- Neonatal Intensive Care Units (NICUs): Modern NICUs are increasingly integrating smart technology and artificial intelligence (AI) to enhance care delivery. In 2024, many hospitals have adopted AI-driven monitoring systems that continuously analyze vital signs and predict potential complications before they become critical.
The modern NICUs use machine learning algorithms to identify patterns that may be missed by human observation, providing early warnings for serious medical conditions. In fact, more seizures are recorded in real-time when the AI algorithms are applied.
Additionally, NICUs are now equipped with advanced incubators that offer more than just a controlled environment. These incubators come with integrated sensors that monitor temperature, humidity, oxygen levels, and even the infant’s movements. Real-time data from these sensors helps healthcare providers make immediate adjustments to optimize the infant’s environment, significantly reducing the risk of complications.
- Telemedicine and Remote Monitoring: Telemedicine has become a crucial tool in neonatal care, particularly in remote or underserved areas. In 2024, advancements in telehealth technology allow for real-time video consultations between neonatologists and local healthcare providers.
Remote monitoring technology has also made significant strides. Wearable devices designed for neonates can now continuously track vital signs and other health metrics, transmitting data to healthcare providers instantly. These devices are minimally invasive, ensuring that they do not interfere with the infant’s comfort while providing critical health information.
- Respiratory Support: Respiratory support is a cornerstone of neonatal care, especially for preterm infants whose lungs are not fully developed. In 2024, advancements in this area are particularly noteworthy.
The high-frequency ventilation and non-invasive procedures are two examples of innovations in the respiratory support systems that have been able to improve the prognosis for neonates suffering from respiratory distress syndrome. These developments also lower the likelihood of long-term problems by offering mild and efficient breathing assistance.
Furthermore, innovations in surfactant therapy, which helps to reduce the surface tension in the lungs and keep the airways open, are enhancing the survival rates and respiratory outcomes for preterm infants.
- Personalized Medicine and Genomics: Personalized medicine is transforming neonatal care by customising treatments to the individual needs of each infant. Advances in genomic sequencing allow for the early identification of genetic disorders enabling targeted interventions.
In 2024, whole-genome sequencing is becoming more accessible and faster, allowing for timely diagnosis and treatment of congenital conditions. Pharmacogenomics, which studies how genes affect a person’s response to drugs, is also making its way into neonatal care.
- Advanced Imaging Techniques: Imaging technology has seen remarkable improvements, providing clearer and more detailed views of neonatal anatomy and physiology. High-resolution screening devices such as CFM Olympic Brain Monitor specifically designed for neonates are now available, offering non-invasive ways to screen brain conditions.
In addition, there are other advanced imaging techniques help in early detection of issues such as brain injuries, congenital heart defects, and other critical conditions, allowing for prompt and appropriate interventions.
- Parental Involvement and Support Technologies: A number of technologies have been introduced in 2024 to encourage parental involvement in neonatal care, in recognition of the vital role that parents play in this process.
Throughout their child’s time in the NICU, parents are offered resources to remain informed, involved, and supported. Furthermore, specially made wraps and clothes are making skin-to-skin contact—also referred to as Kangaroo care. These items enable parents to comfortably hold their infants while providing the essential medical supervision and assistance.
Summing It Up:
The advancements in neonatal technology in 2024 are profoundly transforming the care and outcomes for newborns, especially those born prematurely or with critical conditions.
As technology continues to evolve, the hope is that these advancements will become accessible to all, ensuring that every newborn receives the highest standard of care, regardless of their circumstances.
Source: https://www.genworkshealth.com/blog/advancements-in-neonatal-technology-whats-new-in 2024#:~:text=In%202024%2C%20whole%2Dgenome%20sequencing,its%20way%20into%20neonatal%20care.

Effect of neonatal nurse mentorship in improving neonatal care competencies among neonatal nurses in Rwandan hospitals
Marie Louise Manirakiza, Aphrodis Gustave Tuyishime, Amedee Fidele Ndibaza, Francoise Musabeyezu, Benjamin Kulaaza, Francois Biziyaremye, Dieudonne Ndatimana, Richard Kalisa … See all authors
First published: 21 December 2023 https://doi.org/10.1002/puh2.141

Abstract
Background
Despite healthcare improvements in Rwanda, newborn mortality remains high. This study assesses the impact of neonatal mentorship on enhancing nurses’ competencies within neonatal units, aiming to address this mortality concern and strengthen healthcare providers’ abilities.
Methods
The prospective cohort study included 25 health facilities supported by Ingobyi Activity in Rwanda, which were beneficiaries of a monthly mentorship program focusing on five critical neonatal competencies. These included adopt manipulation of neonatal equipment, effective management of small and sick newborns, stringent infection prevention and control (IPC), kangaroo mother care (KMC) implementation, and family-centered care provision. We employed an observation checklist to measure neonatal practice competencies, comparing practices at the time point of the baseline, at the 6th mentorship session, and finally at the 12th mentorship session.
Results
The program engaged 188 neonatal nurse mentees. Data analysis highlighted a substantial increase in overall neonatal practice competencies from a baseline of 42.7%–75.4% after 12 mentorship sessions. Specific competency enhancements included family-centered care (40.3%–70.3%), IPC (43.2%–84.2%), KMC (56.9%–73.3%), management of small and sick newborns (38.5%–77.6%), and manipulation of neonatal equipment (42.7%–75.4%).
Conclusions
This neonatal mentorship program was effective in enhancing nursing competencies, leading to significant improvements in neonatal care practices. Future work should evaluate the program’s cost-effectiveness and explore its potential to positively impact neonatal health outcomes, thus ensuring sustainable healthcare advancements.


We are delighted to present an editorial for the Special Issue ‘Advances in Healthcare for Neonates’. This Special Issue is a testament to the excellent quality of the eleven articles submitted in the short span of just one year, far exceeding our expectations. We are humbled by the commitment of the scientific community to pursue neonatal research across the globe, which bodes well for improvements in quality of life as newborns grow into children and adults.
The survival of extremely preterm infants in the past few decades is closely linked to the discovery of surfactants in the early 1990s. Advances in neonatal care, including parenteral nutrition, gentle ventilation, and infection control practices, have further contributed to the increasing survival of extremely low birth weight (ELBW) infants. The extensive use of continuous positive airway pressure (CPAP) and non-invasive ventilation (NIV) techniques is essential for the close monitoring of infants on NIV to ensure appropriate clinical decision-making. One such method is standardizing the weaning process when using non-invasive ventilatory support. Nussbaum et al. attempted to standardize the weaning of NIV using the Silverman–Andersen score (SAS). The study did not find any differences among the groups, highlighting the fact that various factors, including interrater reliability, influence weaning from NIV, thereby limiting the predictive value of the SAS. However, the study addresses an important knowledge gap in weaning infants on NIV off respiratory support.
Neonatal units have traditionally used chest X-ray for the diagnosis of respiratory disorders in neonates. However, more recently, lung ultrasound has emerged as a useful clinical tool at the bedside. Ismail et al. have demonstrated that imaging using lung ultrasound can not only be used as an alternative to chest X-ray, but also as a high-precision tool for diagnosing various respiratory diseases in neonates, such as respiratory distress syndrome, pneumonia, transient tachypnea of the newborn, meconium aspiration syndrome, pneumothorax, and atelectasis. Incorporating point-of care-ultrasound scanning in scientific studies and training programs would certainly enhance the existing clinical applications of ultrasound, thus helping to advance the care of neonates.
Despite advances in neonatal care leading to the increased survival of ELBW infants, premature infants are at an increased risk of adverse long-term neurodevelopmental outcomes, including cerebral palsy. Assessment of motor movements based on heart rate is a novel way of detecting abnormal pathologies that could help in earlier detection of cerebral palsy. In this Special Issue, Maeda et al., from Japan, present an algorithm to extract the movement patterns of premature neonates, as assessed through a combination of heart rate and video recordings of general movements. The authors demonstrated that it is possible to use an algorithm-based approach to assess general movements using instantaneous heart rate monitoring; however, they caution that it is essential to distinguish artifacts, such as a care intervention, using a supplemental video recording . Nevertheless, as fetal movements indicate fetal wellbeing, movement pattern assessment using algorithmic tools could be valuable for assessing motor and cognitive functions in premature infants after birth.
Early diagnosis and appropriate intervention can minimize the risk of developmental delays sometimes seen in premature neonates. A randomized controlled study comparing standardized early physical therapy versus no intervention in preterm infants from 32 weeks of gestation to 2 months corrected age demonstrated no differences between the group. However, factors such as the dose, intensity of intervention, parental compliance, and the shorter duration of intervention might have contributed to an absence of difference between the groups. The authors also highlight that engaging with and educating parents demonstrating poor compliance with therapy techniques for prolonged periods is essential to derive benefits .
Implementation of neuroprotective care in the neonatal intensive care unit is essential for optimal neurodevelopmental outcomes in premature neonates. Therefore, reducing pain is critical for neuroprotective care in premature infants. Dusek et al. studied the possibilities of influencing the procedural pain associated with retinopathy of prematurity (ROP) screening using oral clonidine. The authors assessed the pain and vegetative scores of using oral clonidine versus standard care during routine ROP exams. Although they did not demonstrate any difference between the groups, the absence of severe complications with clonidine may make it a potential candidate in future studies addressing neonatal pain.
The clinical care of neonates is the focus of this Special Issue. Traumatic lumbar puncture (LP) has been a problem confounding the diagnostic evaluation of neonates, especially in extremely low birth weight infants. In addition to ensuring the proceduralist′s technique, skills, and experience, it is also essential to use the correct size of needle when performing a procedure. In a study in this Special Issue, a smaller gauge (25G) lumbar puncture needle not only resulted in a decreased incidence of traumatic LP, but also a reduction in desaturation episodes during the procedure. This study is a step in the right direction for providing neuroprotective care to these fragile infants. Future studies should address optimal positioning, non-invasive imaging techniques to facilitate easier insertion, and needle size stratification based on gestational age or birth weight in order to optimize the success of vital neonatal procedures.
Improving the outcomes of neonates is best accomplished by preventing hospital-acquired infections and ensuring the optimal screening of newborns in the intensive care unit. The World Health Organization has described antimicrobial resistance as a serious threat to public health; hence, screening fragile infants for multidrug-resistant microbes is essential. Out born infants admitted to neonatal units in Turkey were meticulously screened using perirectal swab cultures and were found to have a 27.2% and 4.8% positive screening rate for carbapenem-resistant Enterobacterales (CRE) and vancomycin-resistant Enterococci (VRE), among the 125 referrals from the outside hospitals. This result reinforces the need for antibiotic stewardship to prevent multidrug resistance, and high vigilance and attention to screening when these vulnerable neonatal patients are referred from centers in which antibiotic policies are unclear.
Next-generation sequencing (NGS) and exome and genome sequencing using targeted panel molecular genetic analysis have contributed significantly to advances in newborn care. In this issue of Advances in Newborn Care, Zaza et al. describe a neonate with a cleft palate and an aortic root aneurysm, with a pathogenic mutation of exon 8 of TGFBR2 confirming a diagnosis of Loeys–Dietz syndrome. Advances in molecular genetics will help better diagnose rare conditions using genetic mutations, thus contributing to earlier detection of conditions and better management of these infants. Neonates with special conditions and genetic syndromes require a higher level of care and treatment strategies, and standardized tools to enhance their recovery. Vogt et al. propose an enhanced recovery protocol for patients undergoing the Kasai procedure for biliary atresia. The checklist includes, among other elements, parental education, preoperative dextrose-containing fluids, maintaining normothermia, adequate analgesia, and initiation of early feeds. The checklists almost always provide a framework for clinicians to optimize outcomes in complex patients such as those requiring the Kasai procedure.
With the increasing survival of premature infants, many patients go home with an accompanying increase in respiratory morbidities post-discharge. The widespread use of palivizumab helps to reduce re-admission rates and complications from infection with respiratory syncytial virus. The feasibility of home immunization with palivizumab without any serious adverse events is reported in this Special Issue . The advantages of home immunizations include higher parental satisfaction and well-being for the whole family. This study is a step towards personalized medicine within a unique population, which may help them to avoid visiting the hospital or clinic and potentially being exposed to children with other droplet infections. On the note of personalized medicine, there is an increase in the growing adult population who were born prematurely and are thus at extremely high risk of developing various comorbidities such as systemic hypertension, metabolic syndrome, reduced exercise tolerance, pulmonary hypertension, chronic obstructive pulmonary disease, and cardiac failure. Holistically addressing the problems of adults born preterm will help promote cardiovascular health, wellness, and quality of life over their lifetime. Despite the large number of resources invested in the survival and care of extremely premature infants, it is surprising that minimal resources are available regarding commitment to wellness as infants grow into children and adults. Vital screening programs, effective communication, targeted counseling and therapeutic interventions, and a seamless transition of care from a pediatric clinician to an adult health care provider would improve the quality and longevity of life of those born extremely preterm.

Infants Exposed to Substances Prenatally Also Have Increased Exposure to Unsafe Sleep Practices

Unsafe sleep practices may be a more common cause of sudden unexpected infant death cases where children are born exposed to drugs, according to a new study. The article, “Sleep-Related Sudden Unexpected Infant Death Among Infants Prenatally Substance Exposed,” published in the December edition of Pediatrics, looked at data from the Centers for Disease Control and Prevention SUID and Sudden Death in the Young Case Registry. Data showed that of 2,010 infants with sleep related deaths, 14% had been born drug exposed with nearly a third of all infants dying from suffocation. Among the sleep-related deaths, about half happened in an adult bed with infants sharing the space with a sleeping adult. Overall, 1 in 4 deaths of prenatally exposed infants involved supervisors who were both impaired and bedsharing. Non-Hispanic white infants were disproportionately impacted, making up nearly half of those prenatally exposed who died in their sleep. These infants were also more likely to be exposed to social drivers of poor health and family vulnerability such as poverty and barrier to prenatal care. Study authors advocated for expanded prevention efforts such as safe sleep messaging while arguing more needs to be done to address the social needs of these families.
The American Academy of Pediatrics is an organization of 67,000 primary care pediatricians, pediatric medical subspecialists and pediatric surgical specialists dedicated to the health, safety and well-being of infants, children, adolescents and young adults.

A genetic signature in newborns can predict neonatal sepsis before symptoms even start to show, according to a new study

The study, led by UBC and SFU researchers in collaboration with the Medical Research Council (MRC) Unit The Gambia, has the potential to help healthcare workers diagnose babies earlier, including in lower- and middle-income countries (LMICs) where neonatal sepsis is of particular concern. The research, published today in eBiomedicine, is funded by the National Institutes of Health and the Canadian Institutes of Health Research.
“Neonatal sepsis is caused by the body’s irregular response to a severe infection that occurs within the first 28 days of life. Globally, it affects around 1.3 million babies annually, and unfortunately, in LMICs, those rates are higher,” said first author Andy An, a UBC MD/PhD student who completed the research as a doctoral student in the department of microbiology and immunology. “Even when treatment is successful, sepsis can have lifelong effects because it can lead to developmental delay in children, imposing cognitive deficits and long-term health issues. By recognizing it as early as possible, we can treat infants promptly and ideally, head off these harms.”
Neonatal sepsis causes an estimated 200,000 deaths worldwide each year, with the highest rates in LMICs. In Canada, the risk is lower at about one in 200 live births, but higher in prematurely born babies.
Rolling the dice on health
Diagnosing sepsis is challenging for doctors and families. The symptoms can look like many other illnesses, and tests to check if sepsis is present can take several days, aren’t always accurate, and are largely only available in hospitals. The uncertainty can delay urgent treatment with antibiotics.
“Knowing that sepsis is impending would also allow physicians more time to determine the appropriate treatment to use,” said co-senior author Dr. Bob Hancock, professor in the UBC department of microbiology and immunology. “The consequences of neonatal sepsis are so severe in the most vulnerable individuals that providing an early diagnosis to assist and guide physicians could save lives.”
Equitable access to healthcare
The researchers participated in a large study in The Gambia where blood samples were taken from 720 infants at birth. Out of this cohort, 15 babies developed early-onset sepsis.
The researchers used machine learning to map the expression of genes active at birth, in search of biological markers that could predict sepsis.
“We found four genes that, when combined in a ‘signature’, could accurately predict sepsis in newborns nine times out of 10,” said co-senior author Dr. Amy Lee, assistant professor in the SFU department of molecular biology and biochemistry. “This was a unique opportunity where samples were available from all babies in this cohort on the day of birth, meaning we could study the genes expressed in the sepsis babies before they got sick. Most other studies have only published markers that were present when the babies were already ill, and this would therefore not be a predictive signature.”
“The early recognition of sepsis is vital for infants’ survival, and identifying markers that might allow us to ‘predict’ babies at particular risk would be an enormous advantage, since we could then target specific surveillance and treatment of such infants,” said Dr. Beate Kampmann, who led the clinical component of the study at the MRC Unit in The Gambia.
The researchers hope the signature will one day be incorporated not only into PCR tests in hospitals, but also in portable, point-of-care devices.
“There are point-of-care devices available that can test for gene expression, for instance, COVID-19 and influenza, with a single drop of blood. They can operate anywhere with a power source including batteries and can be used by anyone, not just trained healthcare providers,” Dr. Hancock. “These portable devices could be retooled to recognize this ‘signature’ relatively easily and inexpensively.”
The next step for the research would involve a large prospective study to show the signature is successful at predicting sepsis in other populations and prove its methodology, and then the development of point-of-care tools for approval by relevant government bodies.
Source:https://www.sciencedaily.com/releases/2024/10/241028211504.htm



Ready to kick off the new year with fresh goals and BIG dreams? This fun and interactive video is perfect for kids, parents, and educators! We’ll share simple and achievable New Year’s resolution ideas for kids to help them learn goal-setting in a positive and exciting way.

Welcoming the New Year with Hope and Resilience
As preemie warriors, we step into 2025 with gratitude and pride, not just for how far we’ve come but for the people who made our journey possible. This new year is a moment to reflect on the strength and resilience that define us—and to honor the families, parents, caregivers, and healthcare providers who stood by us every step of the way.
Our journey has been shaped by many. For some, families and communities stood as steadfast advocates, offering love and support through difficult decisions and uncertain times. For others, healthcare providers brought their expertise and compassion to the forefront, working tirelessly to help achieve the best possible outcomes. Together, these connections have been a source of strength, ensuring care and hope in moments that mattered most.
2025 is a celebration of this community of support. Together, we’ve proven that resilience is a collective effort. Every milestone we’ve reached—every breath, every step, every moment of growth—is a shared triumph, a testament to the power of unity and the impact of care.
This year, let’s continue to inspire and uplift one another. Our stories remind the world that we as preemie warriors have so much to offer, and that progress in neonatal care depends on the passion and dedication of our neonatal womb community, preemie warriors, families, and professionals alike. By sharing our journeys, we create a ripple effect—sparking change, advancing care, and building a future where every preemie has the best chance to thrive.
Here’s to 2025: a year to honor the bonds that sustain us, the progress we’ve made, and the hope we carry forward. Together, we rise, stronger and more united than ever.


CGI Animated Short Film: “Miles to Fly” by Stream Star Studio | CGMeetup
Follow your Dreams – Miles to Fly is a graduation short made by 4 students from Multimedia University, Malaysia released in 2020. The story is about an ambitious boy who dreams of becoming a pilot but is torn between helping his mother’s bakery to survive, or pursuing his dream.


Surfing at Cherating Point – Pahang, Malaysia

Mar 12, 2018 Kembara Xscapes