
Belarus currently has the lowest preterm birthrate of all globally ranked countries.
BELARUS
Rate: 4.1% Rank: 184
Source: https://www.marchofdimes.org/mission/global-preterm.aspx#tabs-3
Belarus: officially the Republic of Belarus, formerly known by its Russian name Byelorussia or Belorussia is a landlocked country in Eastern Europe bordered by Russia to the northeast, Ukraine to the south, Poland to the west, and Lithuania and Latvia to the northwest. Its capital and most populous city is Minsk. Over 40% of its 207,600 square kilometres (80,200 sq mi) is forested. Its major economic sectors are service industries and manufacturing.
Source: https://en.wikipedia.org/wiki/Belarus
Healthcare- Belarus
Information available regarding healthcare in Belarus indicates that citizens have access to free medical aide and affordable medications. There may be many issues that contribute to preterm birth rates and infant mortality in any given country, or even section of a country. The US is indicated to be the wealthiest country, and yet our infant mortality and preterm birth rates are similar to or worse than many “developing” nations. It is a fact that access to healthcare in a major determinant of infant mortality and preterm birth rates, yet in my research I read articles in US publications that listed off many other potential factors related to infant mortality and preterm birth rates that did not mention access to healthcare. Interesting…..It makes sense to use our access to Global metrics and research to support and guide US research and solution-oriented efforts to reduce the high infant mortality and preterm birth rates in the USA. What can we learn from countries like Belarus to improve our efforts to prevent preterm birth?

The healthcare system in the Republic of Belarus is based on the principles of social justice and affordability. (Source: President of The Republic of Belarus)
 A kidney transplant surgery is performed at the Grodno Oblast Clinical Hospital
A kidney transplant surgery is performed at the Grodno Oblast Clinical Hospital
In line with the Belarusian legislation, all people are guaranteed:
- free medical aid in state-run healthcare institutions;
- affordability of medications;
- informed voluntary consent to medical intervention;
- the right to choose an attending doctor and a healthcare facility;
- participation in the choice of treatment methods;
- availability of information about their own health status, treatment methods, and qualifications of the attending doctor, other personnel directly involved in the treatment process;
- the right to choose people who can be informed about their health status;
- the right to deny medical treatment, including medical intervention, with the exception of the cases stipulated by the legislation;
- in-patient treatment in healthcare facilities meeting hygiene, sanitary, and anti-epidemic requirements; the right to security and protection of personal dignity;
- respectful and humane attitude of healthcare workers.
The entire healthcare system has been recently modernized in Belarus, from first-aid and obstetric stations to regional hospitals and advanced healthcare facilities.
Sixteen specialized national research centers have been set up in Belarus. These include the Cardiology Center, the Mother and Child Center, the Center for Transplantation of Organs and Tissues, the Neurology and Neurosurgery Center, the Center for Transfusion and Medical Biotechnologies, the Traumatology and Orthopedics Center, etc. Their goal is to bring together research and practice to apply state-of-the-art technologies in treatment and diagnostics.
The government has an unwavering focus on the well-being of women and children. Belarusian prenatal centers nurse newborns whose weight is below 500g. In 2008 the program of mass screening of children and newborn babies was launched in Belarus in a bid to improve medical aid to pregnant women and newborns.
Recuperation facilities are part of the medical rehabilitation network. There are 475 recuperation centers in Belarus.
It is always better to prevent a disease than to treat it. That is why Belarusian healthcare professionals invest a lot of efforts in preventing health hazards, promoting a healthy lifestyle and creating appropriate conditions for it. Belarus runs a comprehensive educational and awareness-raising system aimed to promote a healthy lifestyle.
National programs Cardiology, Oncology, Tuberculosis, Innovative Technologies and many more are implemented in the country. The National AIDS Prevention Center was established in Belarus to curb the spread of HIV.
The national healthcare system aims to make the population healthier by raising the quality of medical services and ensuring equal healthcare opportunities for all people regardless of their residence.
The Belarusian healthcare system is working to apply more high-tech projects and innovation technologies. There are plans to raise more investments, promote public-private partnership, expand the range of paid medical services, while preserving the opportunity to get free medical treatment. Belarus is also determined to increase the export of medical services fivefold by 2015 in comparison with the year 2010.
Source: http://president.gov.by/en/medicine_en/
COMMUNITY
We are packing for the annual Zumba Instructor’s Convention in Orlando, Florida where 7-8000 Global instructors will gather to learn, share, teach, and collaborate globally to build community through dance, fitness, music and, of course, having FUN! Because the global average for preterm birth is more than one in ten babies, a large portion of our global Zumba buddies are also Neonatal Womb Warriors and/or Neonatal Womb community partners.

Love /ZIN 75/OFICIAL CHOREO / ZIN MINSK
Published on Jun 21, 2018

Our infant mortality rate is a national embarrassment–By Christopher Ingraham September 29, 2014

The United States has a higher infant mortality rate than any of the other 27 wealthy countries, according to a new report from the Centers for Disease Control. A baby born in the U.S. is nearly three times as likely to die during her first year of life as one born in Finland or Japan. That same American baby is about twice as likely to die in her first year as a Spanish or Korean one.
Despite healthcare spending levels that are significantly higher than any other country in the world, a baby born in the U.S. is less likely to see his first birthday than one born in Hungary, Poland or Slovakia. Or in Belarus. Or in Cuba, for that matter.
The U.S. rate of 6.1 infant deaths per 1,000 live births masks considerable state-level variation. If Alabama were a country, its rate of 8.7 infant deaths per 1,000 would place it slightly behind Lebanon in the world rankings. Mississippi, with its 9.6 deaths, would be somewhere between Botswana and Bahrain.
We’re the wealthiest nation in the world. How did we end up like this?
New research, in a draft paper from Alice Chen of the University of South California, Emily Oster of the University of Chicago, and Heidi Williams of MIT, offers up some clues. They note that the infant mortality gap between the U.S. and other wealthy nations has been persistent — and is poorly understood.
One factor, according to the paper: “Extremely preterm births recorded in some places may be considered a miscarriage or still birth in other countries. Since survival before 22 weeks or under 500 grams is very rare, categorizing these births as live births will inflate reported infant mortality rates (which are reported as a share of live births).”
Oster and her colleagues found that this reporting difference accounts for up to 40 percent of the U.S. infant mortality disadvantage relative to Austria and Finland. This is somewhat heartening.
But what about that other 60 percent?
“Most striking,” they write, “the US has similar neonatal mortality but a substantial disadvantage in postneonatal mortality” compared to Austria and Finland. In other words, mortality rates among infants in their first days and weeks of life are similar across all three countries. But as infants get older, a mortality gap opens between the U.S. and the other countries, and widens considerably. You can see this clearly in the chart below.

Digging deeper into these numbers, Oster and her colleagues found that the higher U.S. mortality rates are due “entirely, or almost entirely, to high mortality among less advantaged groups.” To put it bluntly, babies born to poor moms in the U.S. are significantly more likely to die in their first year than babies born to wealthier moms.

In fact, infant mortality rates among wealthy Americans are similar to the mortality rates among wealthy Fins and Austrians. The difference is that in Finland and Austria, poor babies are nearly as likely to survive their first years as wealthy ones. In the U.S. – land of opportunity – that is starkly not the case: “there is tremendous inequality in the US, with lower education groups, unmarried and African-American women having much higher infant mortality rates,” the authors conclude.
One way of understanding these numbers is by noting that most American babies, regardless of socio-economic status, are born in hospitals. And while in the hospital, American infants receive exceedingly good care – our neo-natal intensive care units are among the best in the world. This may explain why mortality rates in the first few weeks of life are similar in the U.S., Finland and Austria.
But the differences arise after infants are sent home. Poor American families have considerably less access to quality healthcare as their wealthier counterparts.
One measure of the Affordable Care Act’s success, then, will be whether it leads to improvements in the infant mortality rate. Oster and her colleagues note that Obamacare contains provisions to expand post-natal home nurse visits, which are fairly common in Europe.
Research like this drives home the notion that economic debates in this country – about inequality, poverty, healthcare – aren’t just policy abstractions. There are real lives at stake.
*** Update – Mary Katherine Wildeman – Jan 8, 2018
New data released by the Centers for Disease Control and Prevention shows there was no change in the national rate of infant mortality between 2014 and 2015, the most recent years for which it has published numbers.
 Kat and I were pleased to read a copy of a recent letter sent by APHA to Washington DC encouraging support of federal research and promoting known interventions and community initiatives related to preterm birth.
Kat and I were pleased to read a copy of a recent letter sent by APHA to Washington DC encouraging support of federal research and promoting known interventions and community initiatives related to preterm birth.
About APHA:
“We all deserve access to a culture of health – living as long as you can, as well as you can and having a short but glorious ending. It also means having a system in place that ensures we can all achieve it.” – APHA Executive Director Georges Benjamin, MD
APHA champions the health of all people and all communities. We strengthen the public health profession. We speak out for public health issues and policies backed by science. We are the only organization that influences federal policy, has a nearly 150-year perspective and brings together members from all fields of public health.
Please see the letter below and note all who signed it!
June 25, 2018
The Honorable Lamar Alexander The Honorable Michael Bennet Chairman, Senate Committee on Health, 261 Russell Senate Office Building Education, Labor and Pensions Washington, DC 20510 428 Dirksen Senate Office Building Washington, DC 20510
Dear Chairman Alexander and Senator Bennet,
The undersigned organizations committed to the health and wellbeing of mothers, infants, children and families applaud introduction of S. 3029/H.R. 6085, the PREEMIE Reauthorization Act of 2018, and support its swift passage.
Every day, one in ten infants is born premature in our nation. Preterm delivery can happen to any pregnant woman, and often its cause is unknown. Preterm birth is the leading contributor to infant death, and those babies who survive are more likely to suffer from intellectual and physical disabilities. In addition to its human, emotional, and financial impact on families, preterm birth places a tremendous economic burden on our nation. A 2006 report by the National Academy of Medicine found the cost associated with preterm birth in the United States was $26.2 billion annually, or $51,600 per infant born preterm. Employers, private insurers and individuals bear approximately half of the costs of health care for these infants, and another 40 percent is paid by Medicaid.
The original PREEMIE Act (P.L. 109-450) brought the first-ever national focus to prematurity prevention. For several years after its passage, preterm birth rates dropped by small but significant increments. Unfortunately, for the past three years, preterm birth rates have once again risen. In particular, troubling racial disparities in preterm birth persist, with black women experiencing preterm birth rates more than 50% higher than white women. Clearly, our nation must redouble its efforts to ensuring that every pregnancy and baby is as healthy as possible.
The PREEMIE Reauthorization Act of 2018 demonstrates Congress’s continued commitment to our most vulnerable infants and their families by supporting federal research and promoting known interventions and community initiatives. We applaud your sponsorship of this critically important legislation, and we strongly support its passage. If our organizations may be of further assistance, please contact Cindy Pellegrini at March of Dimes at cpellegrini@marchofdimes.org or 202/659-1800.
1,000 Days American Academy of Pediatrics American College of Nurse-Midwives American College of Obstetricians and Gynecologists American Psychological Association American Public Health Association American Thoracic Society Association of Maternal & Child Health Programs Association of State and Territorial Health Officials Association of Women’s Health, Obstetric and Neonatal Nurses Birth Equity Collaborative California Breastfeeding Coalition Children’s Dental Health Project Children’s Hospital Association Children’s Hospital of Philadelphia Cribs for Kids Every Mother Counts Every Woman CT Family Voices Ferring Pharmaceuticals First Focus March of Dimes Moms Rising National Hispanic Medical Association National WIC Association Nurse-Family Partnership PCOS Challenge: The National Polycystic Ovary Syndrome Association Preeclampsia Foundation Preemie World, LLC Prevent Blindness Rhode Island Chapter American Academy of Pediatrics Society for Maternal-Fetal Medicine Society for Reproductive Investigation Stanford University
Source: https://www.apha.org/search-results?q=preterm birth
HEALTH CARE PARTNERS
Fetal Immune System May Trigger Premature Birth: Study
April 25, 2018, at 2:00 p.m. Gulf News UK By Dennis Thompson HealthDay

WEDNESDAY, April 25, 2018 (HealthDay News) — Most potential explanations of premature birth revolve around the mother, and what might cause her body to reject her developing fetus. But what if it’s the other way around?
A new study suggests some preterm births occur because the fetus rejects the mother, after its immune system is triggered too early and senses maternal cells as foreign invaders. Researchers found that umbilical cord blood drawn from preemies contained elevated levels of immune cells generated by the fetus. Subsequent lab tests revealed that this immune response had been activated specifically to attack the mother’s cells.
The flood of inflammatory chemicals released during this fetal immune response can induce contractions in the uterus, causing preterm labor, the study concludes.
“We’re showing that in the context of maternal infection or inflammation — the most common cause of preterm labor — the naive fetal immune system wakes up, gets activated too early, and can actually identify and reject the mother’s cells,” said lead researcher Dr. Tippi MacKenzie.
More than one in 10 pregnancies are affected by preterm labor, in which a baby is born earlier than 37 weeks of gestation, said MacKenzie. She is an associate professor with the University of California, San Francisco pediatric surgery and fetal treatment center.Preterm birth is the leading cause of infant mortality in the United States and the world. Children who survive may go on to face a lifetime of health problems. Despite this, the causes of preterm labor remain “one of the big mysteries in science,” MacKenzie said.
Some recent studies have hinted that one cause might be the mother’s immune system rejecting the fetus. Much like an organ transplant, pregnancy requires the immune system of the mother to tolerate the fetus so it is not rejected. Until now, no one has considered that the fetus might play a role, because the fetal immune system is still developing when preterm birth occurs, MacKenzie said.
In their study, the researchers tested umbilical cord blood and maternal blood taken from 89 women who had healthy pregnancies and 70 who went into early labor. There were no signs of immune response in the mother’s blood. However, researchers found that the cord blood of preterm infants had higher levels of two types of immune cells: T cells, which attack foreign agents and promote immune response; and antigen-presenting cells, which guide the T cells to the foreign bodies under attack.
“Both of those cell types were quite immature in the blood of normal healthy term babies we looked at, but both of those cells were quite activated in the preterm labor blood we looked at,” MacKenzie said.Further tests showed that the fetal immune cells were attacking cells from the mother, and releasing significantly higher levels of inflammatory chemicals as part of their attack. In a laboratory model, the researchers showed these chemicals induced contractions in the uterus.
The scientists suspect the fetal immune system becomes triggered as a result of an infection in the mother, and mistakenly identifies the mother as a threat.Dr. Scott Sullivan, head of maternal-fetal medicine at the Medical University of South Carolina in Charleston, welcomed the report. “I really applaud their work, because one of the glaring holes we have with preterm labor and preterm birth is we don’t have a good understanding of the basic mechanisms and underpinning of the symptoms we see,” said Sullivan. At the same time, Sullivan and MacKenzie agreed that this is probably just one of many different ways in which preterm labor occurs.
High blood pressure, diabetes, improper fetal development, early water breaking or a short cervix are other likely risk factors for premature birth, Sullivan said. “As we understand the basic mechanisms, it helps us think of and develop treatments and preventative strategies,” Sullivan said. “Ultimately, there’s not likely to be one treatment that’s going to work for everybody. Ideally, we’re going to end up with different treatments for different mechanisms.” That said, these results might eventually help doctors detect and head off preterm delivery caused specifically by a fetal immune response, MacKenzie noted.
“We can potentially develop some biomarkers that allow us to diagnose it earlier,” MacKenzie said. “And if we know exactly which cell types and which mechanisms are involved, we can potentially develop specific medicines to treat it.” The study was published April 25 in the journal Science Translational Medicine.

Could Early Birth Hinder Adult Success?
By Alan Mozes HealthDay Reporter (HealthDay)
WEDNESDAY, June 6, 2018 (HealthDay News) — Babies born prematurely or very small may not fare as well in life as those born full-term, a new research review suggests.
Adults who were born tiny or early may be more likely to lag behind educationally and professionally. They’re also more likely to use social services, according to the review of 23 prior studies from eight countries.
Preterm birth occurs before the 37th week of pregnancy. The difficulties reported in the new study were greater for those born very prematurely — before 32 weeks.
Despite the findings, study lead author Dieter Wolke stressed that people born early or at a low birth weight are not destined to struggle in adulthood.
“Most preterm-born adults are in employment and live independently. Most do well according to these markers,” said Wolke, a professor of psychology at the University of Warwick in Coventry, England.
The studies involved more than 5.9 million adults in all. They were conducted across the United States, the United Kingdom, Canada, Denmark, Finland, Germany, Norway and Sweden.
Nearly 272,000 participants had been born before 37 weeks or weighed less than 5.5 pounds.
In adulthood, this group was less likely to have gone on to college, less likely to have a job, and more likely to receive social benefits, compared with their full-term peers, the study review found.
These odds tended to rise with the degree of prematurity, especially educationally.
The achievement markers were viewed as stand-ins for overall adult wealth. In other words, preemies were more likely to have financial problems as adults than babies carried to full-term.
Dr. Lisa Waddell, deputy medical officer of the March of Dimes, said these are “important” findings. “They point out a clear association between preterm birth and adverse consequences down the road,” she said. “While we know that there are clinical consequences, this points out the impacts of preterm birth may have a long-term impact on the child into adulthood,” added Waddell, who wasn’t involved with the research.
Globally, about 11 percent of children are born prematurely. And nearly 9 percent of those are born in industrialized nations, according to background notes with the study.
Wolke said prior research suggests “super-sensitive” parenting is critical for helping these early, undersized arrivals to do as well as their average full-term peers.
But he cautioned that more research is needed to pinpoint the best way to foster and maximize resilience among preemies as they develop.
The news wasn’t all troubling: No difference was seen between preemies and full-term births in the ability to live independently as an adult, though Wolke cautioned that this latter finding “requires further investigation.”
What exactly might explain the findings? Wolke said that’s difficult to say, because of differences among the studies.
He noted, for example, that not all the studies analyzed neurological deficits among preemies. That’s one possible driver, among many, behind the findings, he said.
“Neurological deficits and disability will be part of the explanation,” Wolke said. He added such deficits tend to be minor among premature babies born relatively close to full-term.
Waddell said the findings “really reinforce the urgent need to reduce the numbers of preterm births and especially those born very preterm.”
Premature birth and its consequences are the leading contributor to deaths in the first year of life, she said.
“If we are going to give every baby the best possible start in life and the opportunity to grow, live, thrive and change the world, we must support the health of women before, during and after her pregnancy,” said Waddell.
The findings appear in the June 6 online edition of Pediatrics.
Copyright © 2018 HealthDay. All rights reserved.
 REIKI IN THE NICU FOR OPIOID WITHDRAW?
REIKI IN THE NICU FOR OPIOID WITHDRAW?
Noteworthy Professional News
Smith, Heather, E., PhD, RN, NNP-BC, CNS Section Editor(s): Newnam, Katherine M. PhD, RN, CPNP, NNP-BC, IBCLE; ; Smith, Heather E. PhD, RN, NNP-BC, CNS; doi: 10.1097/ANC.0000000000000512
As more Americans are succumbing to opioid abuse, neonates are innocently being affected from those pregnant opioid users. Although this is not a new phenomenan1 in history, it is estimated that today there are over 2 million people with an opioid addiction in the United States.2 Regardless of gestational age beyond viability, many of these neonates end up being cared for in the neonatal intensive care unit (NICU) due to the withdrawal period postdelivery from regular fetal opioid exposure called neonatal abstinence syndrome (NAS).3 , 4 Assessments of neonates with NAS have been measured using several different NAS tools over time, with the Finnegan Neonatal Abstinence Scoring System getting most use.3 , 5 NAS symptoms include, but are not limited to, uncoordinated feeding patterns, vomiting, diarrhea, high-pitched crying, and irritability.3 In premature infants born to opioid-addicted mothers, the risk for more frequent intermittent hypoxemia is present compared with the baseline intermittent hypoxemia common among most premature infants.6 NAS admissions have increased significantly over the last decade, which has increased length of stay and medical interventions.7 Neonatal nurses will need to continue expanding their thoughts and tools to assist in caring for this growing patient population.
One nonpharmacologic option recently researched in this patient population is the use of Reiki therapy.8 Reiki therapy is considered complementary or an alternative medicine that uses the person’s own healing energy guided by a Reiki practitioner to restore the body and/or restore balance within the person.9 Thirty opioid-exposed infants underwent a 30-minute Reiki therapy session with vital signs monitored to ensure the neonate was not overstimulated. Analyses showed performing Reiki in a NAS group of neonates did not pose any adverse events and, in fact, may have caused relaxation as noted by a slight decrease in heart rate during the session.8 Although the sample size was small and much more research is needed to determine further benefit, Reiki may be a viable nonpharmacologic intervention to opioid-exposed neonates with NAS.
Source:https://journals.lww.com/advancesinneonatalcare/Fulltext/2018/06000/NoteworthyProfessional_News.2.aspx
PREEMIE FAMILY PARTNERS
Kat and I witness many spectacular men in our World! This article points out a special way men may excel!

At last, something men are better at than women!
Posted on 28 May 2018 by keithbarrington – Neonatal Research
Following important research in neonatology / newborn medicine from around the world
That is, giving blood for babies, at least maybe.
The introduction to this new publication notes something that I was not aware of, that plasma donated by women is associated with a substantially greater frequency of transfusion related complications than man-plasma. It is thought to be due, perhaps to the leukocyte antibodies in higher concentration in female derived plasma, and the increase in risk is particularly in TRALI (transfusion related lung injury), and was first identified by the UK surveillance program, Serious Hazards of Transfusion, which I guess has the acronym SHAT.
The new article (Murphy T, et al. Impact of Blood Donor Sex on Transfusion-Related Outcomes in Preterm Infants. The Journal of pediatrics. 2018) examined the donor sex of blood given to preterm babies. We use a lot of blood in our tiniest babies, but not that much plasma; platelet transfusions are not uncommon and they contain a lot of plasma. In this study they only included babies who had received blood, and excluded those who had also had high plasma products. They ended up with a cohort of 170 babies under 32 weeks who had received blood, and divided them into groups of female only donors, male only donors and both. Initial comparisons were between the male only and the others, and that showed that babies who were received some female donor blood had more BPD, more composite morbidity and longer hospital stay than those who received exclusively man-blood.
If you think about it, getting out of the NICU having received blood from only male donors, compared to mixed male/female donors is more likely if you only have one or two transfusion donors. So the authors found that the mixed male/female donor group were more likely to have had more transfusions than the male-donor-only group. Perhaps they were therefore were sicker and had more complications. When they corrected for numbers of transfusions there was still a difference, with male-donor-only babies having better outcomes, but with smaller Odds Ratios and confidence intervals that now included no difference.
They then also compared those that had only female donors to the male-donor-only group, to compare recipients who had the same numbers of transfusions; the numbers are now getting smaller, about 60 per group. The odds ratios for BPD and any major morbidity (1.12 and 1.75) remain in the direction of worse outcomes with female-donor blood, but the confidence intervals are now quite wide and include no effect (or even a protective impact).
The data suggest then that it is possible that there is an impact, with man-blood recipients having better outcomes. Certainly a big enough impact to be worth investigating further. Donating blood also increases your life expectancy maybe if more men donated blood we could catch up to women, and provide safer blood to babies also!
Source: https://neonatalresearch.org/2018/05/28/at-last-something-men-are-better-at-than-women/
Books for Preemie Siblings and a Guide for Grandparents

Information is Power, and we know that the preterm birth experience is a walk in the DARK for most. Here are a few resources that may help light the journeys of preterm birth siblings and Grandparents traveling the Neonatal Womb path….
Books for Siblings
Heaven’s Brightest Star- by Kara M. Glad

Evan Early by Rebecca- by Hogue Wojahn

My Baby Sister Is a Preemie (Helping Kids Heal)- by Diana M. Amadeo
(Author), Cheri Bladholm (Illustrator) 
The Ultimate Guide for New Preemie Grandparents
What to do, say, and understand when your grandchild is a preemie-By Trish Ringley, RN Updated August 15, 2017

When Your Grandbaby Is Premature
By Kimberly Tchang

When I was pregnant with my twin boys, I had visions of giving birth to two healthy, full-term babies. But things didn’t turn out that way. Instead, my sons were born prematurely, at 28 weeks, and spent two months in the Neonatal Intensive Care Unit, or NICU. During that all-consuming time, when I was at the NICU every day, and my husband joined me there after work, my mother and my in-laws rose to the occasion. They visited regularly, brought us food, and were thrilled when the nurses eventually gave them the okay to hold their tiny grandsons. Premature babies (defined as being born before the 37th week of pregnancy), make up nearly 13 percent of all U.S. births, according to the March of Dimes, so it’s likely you or someone you know could become the grandparent of a preemie. Following are some suggestions on how best to help your family if your grandchild arrives early, based on my firsthand experience, and that of others who’ve been there.
Prepare for a Bumpy Ride People describe the NICU experience as an emotional roller-coaster ride, and with good reason. Preemies undergo frequent testing and blood transfusions, and typically experience setbacks. Their condition can change on a daily basis.
It can be a traumatic experience, and some grandparents handle the stress better than others. But while you’ll obviously be very worried about your grandchild, falling apart in the NICU is not helpful to anyone. Rebecca Herranen of San Diego knows the stress firsthand. She spent almost three months with her daughter in the NICU after her granddaughter, Ava, was born in 2003. Considered a “micro-preemie,” Ava, now 7, weighed just 1 pound, 15 ounces, when she was born at 26-and-a-half weeks. “When we realized how small Ava was, our greatest fear was that she would not survive,” says Herranen, who now runs a website, AvaBabys.com, specializing in preemie and micro-preemie clothing. “But as grandparents, you have to dig down deep and find the courage to be strong for your kids, because they’re terrified. This is their child.”
Dr. Jennifer Gunter, an OB/GYN from Mill Valley, Calif., found that her parents’ constant questioning only added to her anxiety when she gave birth to premature triplets in 2003; two of her sons survived. “My parents just kept asking me all these questions: When are you coming home? When are they going to get better?” recalls Gunter, author of The Preemie Primer (Da Capo, 2010). “There are so many unknowns — you don’t know if your baby’s coming home soon, or how long he’s going to be on a respirator. And having someone constantly ask you those questions is like reopening a wound.” Gunter recommends that grandparents acknowledge what their children are going through — and then respond proactively. She advises, “Say, This must be so hard for you. How can I help? or, That sounds very stressful. What can I do?”
Stay Behind the Scenes Sometimes, the best thing grandparents can do is not to visit the NICU each day, but to keep things running smoothly at home. While parents juggle work responsibilities and NICU visits, there might be an older sibling to take care of, groceries to buy, or laundry to do — and that’s where you come in. Long-distance grandparents can also help out by sending gift cards to local restaurants, arranging for meal deliveries, or hiring a cleaning service for the family. “Whatever the mom and dad want, Herranen says, “if it’s in your power to help them do it or get it, then do that.”
Spread the News Family and friends are often eager for updates on how a preemie is doing. But it can be exhausting, if not impossible, Gunter says, for parents to recount each day’s events by e-mail, much less to return endless, if solicitous, phone messages — Yes, he’s still on a G-tube; Yes, he’s still on a ventilator. Grandparents can help by keeping everyone updated on the baby’s progress. That might mean making calls or sending e-mails, starting a blog, or creating a page about your grandchild on a website like CaringBridge.com, which offers free, easy-to-use templates. Whatever you decide to report, be sure to get the parents’ okay first.
And then look forward to the day when your precious grandbaby arrives home at last!
Source: https://www.grandparents.com/family-and-relationships/family-matters/premature-grandbabies
INNOVATIONS
Embrace Neonatal MRI System – MRI for Neonates In The NICU

Guernsey’s hospital to launch maternity app to record special moments of premature babies
ITV Report 28 March 2018 at 5:50am
Here at ITV we’re proud to be the most watched, most loved and biggest commercial broadcaster in the UK.
An app which will allow nurses to record special moments missed by parents of premature babies is being launched at Guernsey’s hospital.
vCreate will help reassure parents of their child’s progress when they need to go home to get some much-needed rest, or spend time with older siblings. Nurses at the hospital will be able to record video updates from a hospital-owned tablet, and send them securely to the parent’s own smart device. The application will be free for parents to use and has been set up with the help of the Priaulx Premature Baby Foundation.
Jo Priaulx, co-founder of the PPBF, was keen to support the technology following the premature birth of both of her children. This new technology will give new parents such reassurance as well as an incredible record of how far their baby has come.
– Jo Priaulx, Co-Founder of the PPBD
Heather Renouf, Lead Nurse of the PEH Neonatal Unit has said the app will allow nurses to create video diaries for families to record their child’s development. Nursing staff will be able to record precious moments on camera, like when babies open their eyes for the first time, or comes off ventilation. These milestones are important to parents.
– Heather Renouf, Lead Nurse PEH Neonatal Unit Last updated Wed 28 Mar 2018
WARRIORS:

KAT CHAT
*** In our March 16, 2018 blog (South Korea) we began to write our Writing For Wellness stories. Kat’s story continues as she becomes a volunteer in the NICU…….
The next day I found myself speaking with the volunteer service managers to set up my schedule for volunteer orientation. Within the next two weeks I was signing the paperwork, getting my volunteer badge, and completing the week of volunteer orientation training. After meeting with the volunteer service manager I was given permission to waive the 6-month entry level program as patient escort and directly start my service in the NICU.
Next came a slew of shots required for the safety of the patients. Finalizing my immunization papers and obtaining my volunteer badge I found myself captured by the heart of the community that kept me alive. As I walked into the NICU for the first time what caught my eye was the private patient rooms adorned with name tags and décor personalizing the space for each family. In the center of the unit was the staff station lined with computers and headboards; its ceiling contained tiny star-like lights.
Touring the unit with the nurse manager I was mesmerized by the tiny humans contained in the glass incubators, metal beds, and wooden cribs. I had no idea what my mom must have gone through in the months I was hospitalized. A turning point in my healing journey came to light when I witnessed my first 24-weeker. Watching her tiny body hooked up to various IV’s, laying in the blue light and ventilation of the incubator, I watched as she reached out her hand touching the glass window next to me. In my heart I felt our connection; I was once where she lay. Struggling daily to survive and thrive this little being was barely “keeping her head above water” until an amazing family came into her life! The effects of the couple’s loving visits were quickly noticed in the improvement of the baby’s vitals, and overtime, in the steady advancement in the baby’s overall health. Eventually, the baby left the NICU in the arms of the loving adoptive father and mother. The baby continued to grow and I have no doubt that the adoptive parent’s touch, attention, and deep love for the baby played a crucial part in the survival and vitality of the precious child. This patient’s story of hope has impacted my life and heart in ways that allow me to embrace our global preterm birth community more fully.
During the first few weeks of volunteering I interacted with various staff members, some of whom cared for me as a patient. I was overwhelmed by the stories, questions, and newfound information presented to me by my past care-providers.
Within my second week at the NICU I was able to reconnect to the respiratory therapist that cared for me daily as a patient. Growing up I heard stories of my respiratory therapist, the man now stood before me. This man was very important in my mom’s and my NICU journey. He had taught my mom our nightly ritual of back-tapping and massage we practiced until I was 12. His smile seemed familiar and I immediate felt at home in his presence. My respiratory therapist himself was born premature. An Eritrean native, he is dedicated to providing loving care to each patient and their family. I admire his ability to connect so well with those he works alongside with each day. I believe we connect at a high capacity thru the heart, for my respiratory therapist has a very expansive and loving heart.
I am grateful for the providers like my respiratory therapist that make significant impacts on our NICU family members. I encourage us to all take a moment to reflect on who has impacted our NICU/preterm birth journey. Consider taking the time to thank them whether it be in your heart, through a note, an email or a social media message! We are powerful Neonatal Womb Community members, and as evolved human beings we know the power of gratitude!

WARRIORS! Come Journal With Me !!!!!!
TOP 3 JOURNAL APPS OF 2018
Surfing on an artificial wave Flowboarding
Published on Nov 23, 2017
Flowboarding – Surfing simulator, surfing on artificial flow or wave. May 27, young Belarusian Ruslan Sugako brought Belarus a gold medal!












 Premature birth test being trialed
Premature birth test being trialed







 BRASIL
BRASIL







 By Robert Preidt, HealthDay Reporter
By Robert Preidt, HealthDay Reporter


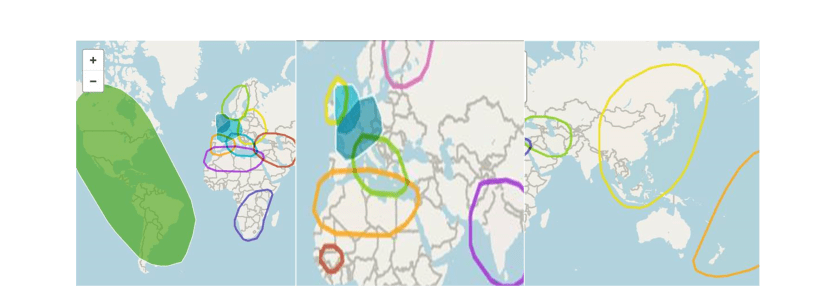 Genealogy of my maternal and paternal strands is pictured above. My brother Seth, sister Ciara and I took our DNA tests and found out our genetic make up is as shown in the photos above. Ethnically we are Western and Eastern European, Scandinavian, North African Berber, Senegalese/Central African, South African, Middle Eastern, South and East Asian, Latin, Indigenous to the Americas, and Polynesian.
Genealogy of my maternal and paternal strands is pictured above. My brother Seth, sister Ciara and I took our DNA tests and found out our genetic make up is as shown in the photos above. Ethnically we are Western and Eastern European, Scandinavian, North African Berber, Senegalese/Central African, South African, Middle Eastern, South and East Asian, Latin, Indigenous to the Americas, and Polynesian.






























 : the 2018
: the 2018 










































 struggles to discover, create, and provide our Neonatal Womb and National Communities with effective healthcare resources, each Country has wisdom and expertise to help us achieve our collective and individual wellness goals. The New England Journal explores Chile’s Health Care changes in the interesting article below:
struggles to discover, create, and provide our Neonatal Womb and National Communities with effective healthcare resources, each Country has wisdom and expertise to help us achieve our collective and individual wellness goals. The New England Journal explores Chile’s Health Care changes in the interesting article below:
 Cuddling my first micro-preemie (also born at 24 weeks gestation) was a sweet/sad emotional moment in time. In my hands lay another human being traveling a familiar path. Holding the preemie was an eye and
Cuddling my first micro-preemie (also born at 24 weeks gestation) was a sweet/sad emotional moment in time. In my hands lay another human being traveling a familiar path. Holding the preemie was an eye and 





 Preterm birth survivors and young children experience trauma differently than people experiencing trauma later in life. Trauma expert Bessel van der Kolk offers empowering tools that may enhance our parenting abilities and family relationships. Van der Kolk also provides a free webinar that may catch your interest!
Preterm birth survivors and young children experience trauma differently than people experiencing trauma later in life. Trauma expert Bessel van der Kolk offers empowering tools that may enhance our parenting abilities and family relationships. Van der Kolk also provides a free webinar that may catch your interest!




