Colombia, officially the Republic of Colombia, is a country primarily located in South America with insular regions in North America. The Colombian mainland is bordered by the Caribbean Sea to the north, Venezuela to the east and northeast, Brazil to the southeast, Ecuador and Peru to the south and southwest, the Pacific Ocean to the west, and Panama to the northwest. Colombia is divided into 32 departments. The Capital District of Bogotá is also the country’s largest city hosting the main financial and cultural hub. Other major urban areas include Medellín, Cali, Barranquilla, Cartagena, Santa Marta, Cúcuta, Ibagué, Villavicencio and Bucaramanga. It covers an area of 1,141,748 square kilometers (440,831 sq mi) and has a population of around 52 million. Its rich cultural heritage[15]—including language, religion, cuisine, and art—reflects its history as a colony, fusing cultural elements brought by immigration from Europe and the Middle East, with those brought by the African diaspora, as well as with those of the various Indigenous civilizations that predate colonization. Spanish is the official language, although Creole, English and 64 other languages are recognized regionally.
Health care in Colombia refers to the prevention, treatment, and management of illness and the preservation of mental and physical well-being through the services offered by the medical, nursing, and allied health professions in the Republic of Colombia.
The Human Rights Measurement Initiative[1] finds that Colombia is fulfilling 94.0% of what it should be fulfilling for the right to health based on its level of income.
The reform of the Colombian healthcare had three main goals:
- The achievement of an antitrust policy, to avoid the statal health monopoly.
- The incorporation of private health providers into the healthcare market
- The creation of a subsidiated healthcare sector covering the poorest population.
The general principles of the law determine that healthcare is a public service that must be granted under conditions of proficiency, universality, social solidarity and participation. Article 153 of the law mandates that health insurance be compulsory, that health providers must have administrative autonomy, and that health users must have free choice of health providers.
Source: https://en.wikipedia.org/wiki/Colombia
- GLOBAL PRETERM BIRTH RATES – COLOMBIA
- Estimated # of preterm births: 9.0 per 100 live births/Global Average: 10.6
- Source- WHO Preterm Birth Rate (Per 100 Live Births)
- World Population Review
COMMUNITY

How to provide neonatal care in low-resource environments | Thomas M. Berger | TEDxGVAGrad

Drawing on historical milestones in neonatology, Professor Thomas Berger highlights the groundbreaking discoveries that revolutionised the care of infants with respiratory distress, ultimately leading to significant reductions in mortality rates. Through his personal experiences in Namibia and the implementation of low-cost interventions in low to middle income countries, he showcases how he has taken matters into his own hands and emphasises the importance of prioritising the patient’s well-being above all else. In this inspiring speech, Professor Berger shows how grit and simple solutions can make a positive impact in saving neonatal babies. Thomas M. Berger is a Swiss paediatrician and neonatologist. His postgraduate training began in Switzerland and continued in the USA (residency in paediatrics at the Mayo Clinic, Rochester, MN; fellowship in neonatology at the Harvard Joint Program in Neonatology, Boston, MA; fellowship in paediatric critical care at the Children’s National Medical Center in Washington, DC). After returning to Switzerland, he led the Neonatal and Paediatric Intensive Care Unit at the Children’s Hospital in Lucerne for almost 20 years. In 2017, together with his wife Sabine (a paediatric nurse), he founded NEO FOR NAMIBIA – Helping Babies Survive. This Swiss NGO helps to improve neonatal care in Namibia by providing affordable and robust equipment, ensuring thorough training of local health care professionals, and measuring impact with appropriate statistics. This talk was given at a TEDx event using the TED conference format but independently organized by a local community. Learn more at https://www.ted.com/tedx

Australian program Every Week Counts says it has helped to prevent about 4,000 preterm and early births each year since 2021
By Charlotte Gore – Mon 18 Mar 24
In short: A program that aims to lower the national rates of preterm and early births says it’s helped 4,000 Australian babies avoid an early birth each year since 2021.
The Every Week Counts program helps maternity hospitals redesign services to identify and treat women at risk of delivering early.
What’s next? Experts involved in the program said they hoped to challenge the belief that full term was 37 weeks gestation.
Sheree Walsh’s twins Heidi and Connor weighed a combined 1250 grams when she delivered her babies at just 25 weeks gestation. The mother only realised she was at risk of a premature birth after she had concerns over a lack of movement and went to the hospital for a check-up. In an ultrasound she could see both babies moving and was temporarily relieved, until the doctor told her to immediately pack her bags to be admitted to the hospital for bed rest.
“I could still feel the babies, but my cervix had shortened so much that it was a risk for me to remain off bed rest,” Ms. Walsh said.
It was not long before the twins arrived.
“We had Heidi and Connor christened the day after they were born because we didn’t think Heidi would make it. She was so sick,” Ms Walsh recalled.
Every Week Counts
A world-first Australian program, led by the Australian Preterm Birth Prevention Alliance (APBPA), has said it has managed to significantly lower the number of preterm and early births across the country.
A preterm birth is one that occurs before 37 weeks gestation, while an early term birth is one that occurs between 37 and 39 weeks — and the Every Week Counts program has aimed to reduce the rates of both.
According to the APBPA, preterm births are the single greatest cause of death and disability in Australians under five years old, and 8 per cent of Australians are born preterm.
Australian Institute for Health and Welfare data has shown that preterm birth rates have fallen by 6 per cent since the APBPA began its work in 2018.
First Nations women are twice as likely as non-Indigenous mothers to experience a preterm or early birth.
APBPA deputy chair Professor Jonathan Morris said recent data from the federally-funded program suggested early term birth rates had declined by at least 10 per cent.
“Over the course of the program, that means 4,000 babies that would’ve been born early have been born at an appropriate time,” he said.
“Meaning they’re more likely to be with their mothers, more likely to be healthy in the first year of life, and more likely to perform well in later life.”
‘She’s a total miracle’
Ms. Walsh said before delivering her twins she had not heard of a Neonatal Intensive Care Unit (NICU) and was yet to attend birth classes.
“A premature birth is something that you’re not prepared for,” she said.
“With many parents of preemies, their relationship doesn’t survive, but we were really lucky because we were there for each other and we had strong support from our family.”
Now almost seven years old, Heidi is vibrant and energetic, and to her parents she’s “a total miracle”.
Most parents don’t have to leave their baby behind when they go home from the hospital.
“Heidi has very limited core strength, however it doesn’t stop her. She is the most resilient child I’ve ever come across,” Ms. Walsh said.
The mother has had a subsequent pregnancy and was able to deliver Heidi and Connor’s younger brother at full term. She said she believed that was due to the extra monitoring and treatments she received under the Every Week Counts program.
‘Misconception’ of 37 weeks as full term
Women’s Healthcare Australasia chief executive Barb Vernon said the Every Week Counts program has helped healthcare workers across multiple hospitals reshape some services with the aim of seeing fewer preterm and early term births. Strategies included prescribing vaginal progesterone to people with a shortened cervix or who have a history of spontaneous preterm birth — a treatment that assisted Ms. Walsh in her subsequent pregnancy.
The program has also promoted the continuity of care model which sees expectant mothers meeting with the same staff. Smoking while pregnant is also strongly discouraged.
“What we’ve been doing in this program is working with the hospitals to help them redesign their own local hospital system, to help them do their best care for every woman every time,” she said. “Whether it’s their electronic medical record, their booking process for an induction, the way they communicate with women during pregnancy and the information they might give women to make informed decisions. “All of those elements of care then have an impact on supporting more women to continue their pregnancy to 39 weeks.”
Dr. Vernon said a common misconception they hoped to address with the program was the idea that a baby had reached full term at 37 weeks gestation.
“That’s an idea that has been around for more than 100 years, but what we now know is that the baby’s brain develops much more powerfully if they’re born two weeks later at 39 weeks of pregnancy,” she said.
Dr Vernon said the program was an important opportunity to help pregnant women understand they would be doing “the best possible thing for their baby” if their pregnancy could safely continue to 39 weeks gestation.
“The advice that is being given to women as part of this work is that they should be seeking to have a cervix length measurement taken when they have their mid-pregnancy scan,” she said.
Dr. Vernon said so far the program’s work had been “really inspiring” in terms of the outcomes for women and their families.
“There are hospitals across Australia, from very large services to very small rural centres, that are seeing a drop in the number of babies being born earlier than they should be born,” she said.
Trust, meaningful conversations key to improving Indigenous outcomes
While the program has seen broad improvements across the country, the positive outcomes have not extended to First Nations women, according to Indigenous obstetrician and gynaecologist Kiarna Brown who lives and works on Larrakia country in the Northern Territory.
“I have the amazing privilege of now working as an obstetrician in the town that I grew up in, and so what that also means is that throughout pregnancies, I’m looking after my cousins and my nieces,” Dr Brown said.
The experience has shown her that First Nations women have better birth outcomes when they feel safe and can trust their maternity care providers.
Dr. Brown was part of a study that examined ten years of births at the Royal Darwin Hospital, finding the prevalence of many risk factors for preterm and early births were the same among Indigenous women compared to other expectant mothers. Those risk factors included preterm membrane ruptures, diabetes in pregnancy, blood pressure issues and whether a woman was carrying more than one baby.
But it did find Indigenous women were more likely to have shorter cervical lengths — an area Dr. Brown said needed more study. She said given preterm birth risk factors were not too dissimilar in Indigenous women, it was likely social determinants of health were responsible for First Nations women being twice as likely to experience preterm births.
“I think it boils down to people’s access to healthcare services … levels of education and employment,” Dr Brown said.
“We also need to find ways to engage and educate women — and I’m not saying we should tell women what to do — but actually getting their perspectives on how [health services] can do better.” “So, that’s what we’ve started in the Top End. We’re doing lots of yarning groups in remote communities, asking:
‘Hey, how can we do better? What do you know about this issue preterm birth? What experience have you had with maternity care?'”
She said the predominantly non-Indigenous workforce urgently needed culturally-informed training, as Western medicine has long ignored how First Nations mothers have traditionally experienced pregnancy.
Dr Brown said one example was that many mothers did not track their pregnancies in weeks or trimesters.
She said instead they might say, “‘My baby’s due in the wet season … or my baby’s as big as a mango'”.
“When they feel safe and trusted, they’re going to come [to maternity services] more often and they’re going to have more meaningful relationships with their healthcare professionals,” Dr Brown said.

Digital health program cuts pre-term births by 20%

May 2, 2024 By Andis Robeznieks, Senior News Writer
Not all telehealth programs began during the COVID-19 pandemic. Ochsner Health started connecting pregnant patients with its digital medicine obstetric program in 2016 and has since achieved success across six key performance metrics including improved clinical outcomes, access to care and health equity.
Ochsner Health’s Connected MOM (Maternity Online Monitoring) initiative uses digital health tools to offer expectant mothers a convenient way to safely manage their pregnancy in collaboration with their physicians at some 20 clinical sites in Louisiana and Mississippi.
In 2022, Ochsner Health enrolled about 205 pregnant patients per month in the program, with nearly 1,600 enrolled at any given time that year and more than 2,250 patients in total for the year, according to an AMA Future of Health case study (PDF).
Ochsner Health is a member of the AMA Health System Program, which provides enterprise solutions to equip leadership, physicians and care teams with resources to help drive the future of medicine.
Patients are given a blood-pressure cuff to enable them to submit BP readings remotely via their personal smartphone.
This enables ob-gyns and patients to track key health readings and receive alerts when a reading is outside normal thresholds. Once alerted, physicians work with patients on a care plan.
Ochsner Health’s program caught the attention of Sen. Bill Cassidy, MD (R-La.), who then used it as the foundation of his Connected MOM Act, a bipartisan bill supported by the AMA (PDF). The bill would provide state Medicaid programs with remote physiologic monitoring devices and related services through Medicaid.
The Connect MOM program is especially helpful in detecting the hypertensive disorders of pregnancy, like preeclampsia, which is responsible for up to 7% of pregnancy-related deaths in the U.S.
Measures indicate success
The case study notes that the program has achieved significant success across these six dimensions.
Clinical outcomes.
Connected MOM participants overall had 20% lower odds of pre-term. The program also helped identify patients with “masked hypertension,” which includes those who had hypertension at home but a normal BP measurement in the clinic and are nonetheless at an increased risk for adverse outcomes. Those patients were given early intervention and closer monitoring.
Access to care. Ochsner Health’s team of more than 120 ob-gyns and certified nurse midwives delivered more than 10,860 babies—of which, about 20% were enrolled in Connected MOM. The option of substituting some in-office visits with virtual visits also was a benefit to patients with transportation challenges, and was helpful to those who otherwise would have had to take time off from work and secure child care to see their physician.
Patient, family and caregiver experience. Ochsner Health data indicates that 10.7% of patients in Connected MOM are re-enrollees, “highlighting a high level of satisfaction with the program,” says the case study.
Clinician experience. Because it is so easy to use the program’s digital tools, staff can better manage their time and offer support to more new patients. For every 1,000 patients enrolled in Connected MOM, the capacity of an ob-gyn’s clinic increases by the equivalent of 0.6 of full-time employee.
Financial operational experience. Connected MOM is offered at no additional cost to patients.
Health equity. Connected MOM supports the recruitment of a diverse demographic of patients, with more than 60% of enrollees being between 26–35 from various racial backgrounds, including 29% Black and 5% Asian, with about 30% of enrollees covered by in-state Medicaid programs.
Grant funding has helped pay for much of the program, so the passage of Dr. Cassidy’s bill would go a long way toward making the program sustainable.
“We’re asking for CMS [the Centers for Medicare & Medicaid Services] to make sure that not just the moms who go to Ochsner, but all moms across the United States are able to benefit from the Bluetooth-enabled blood-pressure devices and remote patient-monitoring devices such as those used in Connected MOM,” Veronica Gillispie-Bell, MD, MAS, head of women’s services at Ochsner Medical Center-Kenner, said in a recent episode of “AMA Update.”
“If we’re really looking to bring resources to those individuals, to those patients who need it the most, we have to have federal support,” Dr. Gillispie-Bell added.
Support for patients and physicians
The case study also highlights how Ochsner Health leverages the foundational pillars for “addressing the digital health disconnect” described in the AMA-Manatt Health report Closing the Digital Health Disconnect: A Blueprint for Optimizing Digitally Enabled Care (PDF).
The blueprint’s foundational pillars to achieve digitally enabled care are:
- Build for patients, physicians and clinicians.
- Design with an equity lens.
- Recenter care around the patient-physician relationship.
- Improve and adopt payment models that incentivize high-value care.
- Create technologies and policies that reduce fragmentation.
- Scale evidence-based models quickly.
In describing how the program is built for patients, physicians and other health professionals, the case study notes that patients are sent reminders to take their BP reading. Patients also receive a weekly planner and checklist for tracking their vital signs.
“The program has been thoughtfully designed to support both patient and clinician needs,” the case study says.
Regarding the pillar on creating technology that reduces fragmentation, the case study notes that sharing data via the patient’s smartphone app means that patients don’t need to copy or transcribe the data to message their physician. “Connected MOM allows for a centralized location for both the care team and the patient to access information, track progress, [and] identify trends,” the case study says.
Juanes, Juan Luis Guerra – Cecilia (Official Video)
Juanes 3.07M subscribers
1.9M views 1 year ago
#JuanLuisGuerra #Juanes #VidaCotidiana

HEALTHCARE PARTNERS

Ethics and Wellness: The Art of Disagreement in Neonatology: Navigating Change with Grace
Mitchell Goldstein, MD, MBA, CML

Neonatology, a field dedicated to the care of newborns, is characterized by its rapid pace of evolution. New research findings, advanced technologies, and updated guidelines continuously reshape our understanding and practices. What was considered best practice a decade ago may be outdated as the field progresses. This constant flux can lead to disagreements among professionals, which, though potentially disruptive, play a critical role in advancing care standards and improving patient outcomes.
Navigating these disagreements with finesse ensures they contribute rather than hinder progress. Constructive disagreement is not just about airing differing opinions; it involves engaging in a thoughtful and respectful dialogue that fosters professional growth and enhances patient care. Here are several fundamental principles for managing disagreements effectively in neonatology.
1. Prioritize Respectful Dialogue
The foundation of productive disagreement is respectful. communication. Interrupting others disrupts the flow of conversation and can escalate tensions. It is crucial to allow each participant to complete their thoughts before responding. This practice ensures that every viewpoint is fully understood and considered. Active listening is a cornerstone of respectful dialogue; it demonstrates that you value the other person’s perspective and are open to their ideas.
2. Let Everyone Speak
Equally important is ensuring that every participant has the opportunity to voice their opinions. Dominating the conversation or dismissing others’ viewpoints can stifle valuable insights and create a skewed discussion. Encourage a balanced exchange where all voices are heard. This inclusive approach not only fosters a more democratic dialogue but also enriches the decision making process by incorporating diverse perspectives.
3. Silence is Golden
In the heat of a debate, silence can be a powerful tool. It provides a moment for reflection and allows participants to process the information being discussed. Rather than rushing to fill every
pause with words, embrace moments of silence as an opportunity to gather your thoughts and consider the points raised by others. Silence can also help de-escalate tensions and allow everyone to cool down before responding.
5. Choose the Appropriate Setting for Discussions
The context in which disagreements occur can significantly impact their resolution. Sensitive or contentious issues are often better addressed in a private rather than a public forum. A private discussion allows for more candid exchanges without the added pressure of an audience, which can lead to more effective problem-solving and reduce the risk of escalating the conflict.
6. Focus on the Issue, Not the Person
Effective disagreement involves focusing on the issue rather than allowing personal animosities to cloud the discussion. Avoid competitive “pissing contests” where the goal is to outshine or undermine the other person. Instead, concentrate on clearly articulating the opposing viewpoint and contrasting it with evidence based data. This approach ensures that the debate remains centered on the merits of the arguments rather than personal conflicts.
7. Use the Praise Sandwich Approach
One effective method for presenting a differing opinion is the “praise sandwich” approach. This technique involves beginning with a positive remark or acknowledgment of the other person’s perspective, presenting your disagreement, and concluding with another positive note. This approach helps soften the impact of dissent and maintains a positive and constructive tone throughout the discussion. It demonstrates respect for the other person’s contributions while making your point.
8. Know When to Step Back
Sometimes, despite our best efforts, discussions can become too heated to be productive. In such cases, stepping back and taking a break is wise. A pause lets participants cool down and reflect on the discussion with a clearer perspective. Revisiting the conversation later can lead to more thoughtful and constructive dialogue, fostering a better resolution.
9. Cultivate an Open Mind
Approaching disagreements with an open mind is essential for constructive dialogue. Suspend disbelief and be willing to consider new ideas, even if they challenge your current beliefs. This willingness to explore different viewpoints can lead to innovative solutions and improvements in practice. Agreeing to disagree is a natural part of professional discourse and can enhance collaboration and problem-solving.
10. Remember the Shared Goal
Regardless of the intensity of the disagreement, it is essential to remember that all participants share a common goal: improving patient care. Maintaining a sense of camaraderie and mutual respect helps to keep the bigger picture in focus. (4) Disagreements should be viewed as opportunities to refine and enhance practices rather than as personal battles.
By adhering to these principles, disagreements can be transformed from potential conflicts into valuable opportunities for professional development and innovation. Constructive disagreement enriches the practice environment and contributes to improved physician retention and a more dynamic approach to patient care. Fostering a respectful dialogue ensures that every voice is heard and that the field of neonatology continues to advance in its pursuit of excellence.
Source: https://neonatologytoday.net/newsletters/nt-sep24.pdf

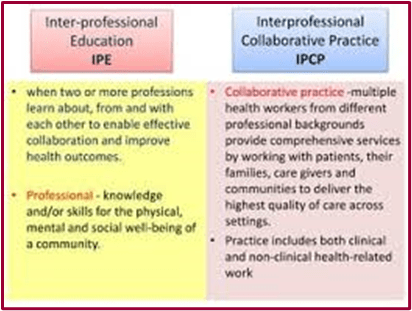
Celebrating the Distinct Contributions of Neonatal Therapists Within Interprofessional Neonatal Care
High-quality neonatal intensive care requires diverse specializations and interprofessional teamwork to include the unique contributions of neonatal therapists. Neonatal therapists include occupational therapists (OT), physical therapists (PT), and speech-language pathologists (SLP), who specialize in delivering age-specific evaluations and therapeutic interventions for premature and medically complex infants in the neonatal intensive care unit (NICU) A neonatal therapist begins with the end in mind to mitigate adverse sequelae, optimize neurodevelopment, and strengthen infant mental health by scaffolding the infant-parent dyad Although therapists are traditionally known for their rehabilitative roots, neonatal therapists utilize a preventative, habilitative approach, emphasizing neuroprotection and neuropromotion .
What is Neonatal Therapy?
Neonatal therapy is an advanced practice area for OTs, PTs, and SLPs as described by the Neonatal Therapy Core Scope of Practice©. All three professional groups share core fundamental knowledge yet recognize that each discipline adds unique and valuable contributions to the field. In part, neonatal therapy is “the art and science of integrating typical development of the infant and family into the environment of the NICU.”. As interdisciplinary care team members, neonatal OTs, PTs, and SLPs help drive the delivery of Family Centered, developmental care and are often instrumental in the discharge planning process. In level III and IV NICU settings, neonatal therapists are integral to neonatal follow-up clinics, providing neurodevelopmental testing and triage for early intervention services.
Why is neonatal therapy considered an advanced practice area?
Professional training programs for OT, PT, or SLP entail graduate-level or doctoral degrees. Despite this rigorous education, advanced training in the neonatal therapy subspecialty is required. An entry-level neonatal therapist requires NICU-specific continuing education and mentorship to ensure safe, well-timed, risk-adjusted neonatal care. Neonatal therapists must be familiar with the complexities of the NICU environment, recognize neonatal risk factors, precautions, and medical comorbidities, navigate NICU equipment, safely handle preterm and critically ill infants, apply trauma-informed principles when working with families, and have a solid understanding of typical preterm and newborn neurobehavior and developmental progression (1-3). This extensive education and training instills confidence in neonatal therapists’ expertise and their ability to provide evidence-based services in this highly vulnerable patient population.
What are the requirements to become a certified neonatal therapist (CNT)?
The CNT designation is internationally recognized and obtained throughthe Neonatal Therapy Certification Board (NTCB). The CNT certification requirements include: (a) credentialling as an OT, PT, or SLP for three or more years, (b) 3500 hours of experience in the NICU, (c) Forty hours of NICU-specific education in less than three years, (d) forty hours of NICU mentorship, and (e) successful completion of the Neonatal Therapy National Certification Exam.
What are the neonatal therapy practice domains?
Neonatal OT, PT, and SLP have a shared foundational knowledge, including six practice domains: (1) environment, (2) family/ psychosocial support, (3) sensory system, (4) neurobehavioral system, (5) neuromotor and musculoskeletal systems, and (6) oral feeding and swallowing, which are not fundamentally exclusive to any one discipline (1,2). Neonatal therapists use an integrative collaborative-care model when administering continual assessment and intervention cycles grounded in evidence-based decision-making (9). Ideally, therapeutic interventions begin at the earliest point of the lifespan when therapists collaborate with other disciplines and use their unique lenses to help advance infant competencies, promote parental confidence, and expedite the journey home.
What interventions do neonatal therapists provide?
From the first day of life, neonatal therapists promote healthy postures and movement patterns, reduce pain and stress, and nurture age-appropriate sensory experiences. In tandem with the bedside nurse, neonatal therapists partner with families to engage them in their baby’s activities of daily living, such as diapering, eating, dressing, bathing, etc.. Neonatal therapists can be instrumental in coaching parents with direct hand-overhand support and anticipatory guidance to help develop proficiency and confidence in their co-occupation as parents. The neonatal therapy team helps to advance individualized care plans to include environmental modifications, positive touch, therapeutic handling for posture and regulation, protection of the aerodigestive system, infant-driven feeding strategies, and parent education related to discharge needs (1, 3, 11). In many settings, neonatal therapists are considered feeding specialists with advanced training in pre-feeding strategies, breastfeeding support, and clinical feeding assessments (10, 13). Highly skilled neonatal therapy professionals will often have extensive training in any of the following areas: (a) evaluating an infant’s neurologic integrity using skilled observations and standardized testing, (b) therapeutic management of orthopedic conditions, (c) instrumental swallowing evaluations such as video fluoroscopic swallow studies (VFSS) or fiberoptic endoscopic evaluation of swallowing (FEES), and (d) lactation support as a Certified Lactation Counselor (CLC) or International Board Certified Lactation Consultant (IBCLC).
What is the best approach to successful neonatal therapy staffing?
With the rising complexity and volume of premature and medically fragile infants, there is a growing need for highly trained, multidisciplinary NICU teams . Finding and staffing NICUs with all three disciplines who also have NICU-specific expertise can be highly challenging, particularly in units with high fluctuations in their census and for smaller, more rural NICUs. Larger level III and IV NICUs have additional staffing challenges of higher acuity, heavy caseloads, and shortage of qualified therapists. The staffing models of neonatal therapy teams often vary in size and the way they delineate roles between neonatal therapists based on therapist availability, cross-discipline knowledge, therapy service requirements, budget constraints, and the individual therapist’s competence and confidence within the neonatal subspecialty. The American Academy of Pediatrics (AAP) NICU Verification Program includes neonatal therapy services for Level II, III, and IV NICUs, with certified neonatal therapists (CNTs) preferred.
Help celebrate neonatal therapists from around the world!
Every September, the National Association of Neonatal Therapists (NANT) hosts International Neonatal Therapy Week (INTW) to highlight this advanced practice area and unite neonatal OT, PT, and SLP clinicians around the globe. NANT is a professional organization that delivers NICU-specific continuing education, resources, standards, mentorship, and supportive connections to advance this specialty. During the week of September 15th-21st, 2024, NANT will celebrate the impact of this vibrant neonatal therapy community with its members, who span over thirty countries and five continents.
Want To Learn More?
• Celebrate International Neonatal Therapy Week between September 15th and 21st, 2024 and join
our vibrant neonatal community.
• Attend NANT 15, the annual neonatal therapy conference, in Indianapolis, IN, from March 27th to
29th, 2025. Attendees typically represent all fifty states and eight or more countries.
• Join NANT’s annual Virtual Summit in December — A FREE educational event— info coming soon! • Stay informed by subscribing to NANT NEWS and visiting www.neonataltherapists.com
• Therapists interested in becoming a CNT can apply online at https://www.ntncb.com/

Effect of Routine Nurse Caregiving on the Stress Responses and Behavior State in Preterm Infants -A Systematic Review

Cistone, Nicole MSN, RN, RNC-NIC; Pickler, Rita H. PhD, RN, FAAN; Fortney, Christine A. PhD, RN, FPCN; Nist, Marliese D. PhD, RNC Editor(s): Gephart, Sheila PhD, RN, Section Editor; Newnam, Katherine PhD, RN, NNP-BC, CPNP, IBCLE, Advances in Neonatal Care 24(5):p 442-452, October 2024. | DOI: 10.1097/ANC.0000000000001177
Abstract
Background:
Although routine nurse caregiving is vital for the overall health of preterm infants, variations in approaches may exert distinct effects on preterm infants’ stress responses and behavior state.
Purpose:
The purpose of this systematic review was to examine routine nurse caregiving in the neonatal intensive care unit and its effect on stress responses and behavior state in preterm infants.
Data Sources:
A systematic search was conducted using PubMed, Embase, and CINAHL for studies published between 2013 and 2023.
Study Selection:
Included studies enrolled preterm infants born <37 weeks gestational age and investigated nurse caregiving practices and effects on stress responses and/or behavior state.
Data Extraction:
Following Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, data about study design, methods, findings, and limitations were extracted and summarized. Included studies were evaluated for bias using the National Health, Lung, and Blood Institute quality assessment tools.
Results:
All 13 studies included in the review received a fair quality rating. Nurse caregiving activities, including suctioning, diaper changes, bathing, and weighing, were associated with increases in heart and respiratory rates, blood pressure, energy expenditure, and motor responses, lower oxygen saturations, and fewer sleep states.
Implications for Practice and Research:
Adapting nurse caregiving frequency and duration, aligning caregiving with infant state, and integrating developmental care strategies may reduce infant stress responses and support behavioral rest. Further research is needed to understand how caregiving activities affect stress responses and behavior state in preterm infants, aiding in identifying modifiable caregiving stressors to promote optimal development.

PREEMIE FAMILY PARTNERS

How the NICU and Occupational Therapy Support a New Baby

Spotsylvania Regional Medical Center Jul 19, 2021
Meet Occupational Therapist Hayley Chrzastowski and learn how a baby in the Level III NICU at Spotsylvania Regional Medical Center would receive care from an occupational therapist. Dr. C Chrzastowski will also discuss how she works to both include and support baby’s care team to best prepare them to care for baby once transitioned home.

Common tests in the NICU

Key Points
Your baby may have tests in the NICU to find out about health conditions and treatments she needs to grow and be healthy.
Some tests, like blood tests, are really common, and lots of babies get them. Others are just for babies with certain health conditions.
Before providers can do certain tests on your baby, you have to give permission. This is called informed consent.
Talk to your baby’s provider about tests your baby needs. Make sure you understand the test and why your baby needs it before you give permission.
Why do babies have tests in the NICU?
Your baby’s health care providers in the newborn intensive care unit (also called NICU) staff give your baby medical tests to find out about your baby’s health conditions. Test results help providers know what treatment your baby needs. For example, providers may do a blood test to check your baby for anemia. Anemia is when your baby doesn’t have enough healthy red blood cells to carry oxygen to the rest of her body. Or providers may take an X-ray to check your baby for a lung infection. Your baby’s provider tells you what tests your baby needs and tells you the test results.
Before providers can do certain tests, they need your consent. This means they’ll ask you to read and sign a consent form. When you sign the form, you give them permission to do the test. Sign the form only when you understand what the test is and why your baby needs it. Ask your baby’s providers any questions you have about the test before you sign the form.
What tests may your baby have in the NICU?
blood test — Tests your baby’s blood for certain health conditions. Blood tests are the most common tests done in the NICU. Test results give providers important information about your baby’s health. They also help providers find possible problems before they become serious.
CAT scan or CT scan — Also called computed tomography scan. A test that takes pictures of the inside of the body. It’s like an X-ray, but it gives a clearer, three dimensional (also called 3D) view. Your baby goes to the radiology department for the test. She may need medicine to help keep her still during the test.
echocardiogram — A special kind of ultrasound that takes pictures of the heart. Ultrasound uses sound waves and a computer screen to make the pictures. Providers use this test to help find heart problems, including heart defects. A heart defect is a problem with the heart that’s present at birth.
EKG or ECG— Also called electrocardiogram. A test that records the heart’s electrical activity. An EKG can show how fast your baby’s heart is beating and if the rhythm of the heartbeat is regular.
hearing test — Also called brainstem auditory evoked response test or BAER. This test checks your baby’s hearing. A provider places a tiny earphone in your baby’s ear and puts small sensors on his head. The provider plays sounds through the earphones, and the sensors send information to a machine that measures your baby’s response to the sounds. All babies get this test as part of newborn screening.
MRI— Also called magnetic resonance imaging. This test uses strong magnets and radio waves to take detailed pictures of the inside of your baby’s body. An MRI gives a more detailed view than a CT scan, X-ray or ultrasound. Your baby may need medicine to help keep her still during the test.
newborn screening test — Checks for serious but rare and mostly treatable conditions at birth. It includes blood, hearing and heart screening.
ROP exam— Also called retinopathy of prematurity exam or eye exam. Providers use this test most often for babies born before 30 weeks of pregnancy or babies who weigh less than 3 1/3 pounds. An eye doctor (also called an ophthalmologist) checks to see if the blood vessels in your baby’s eyes are developing the right way. If the doctor sees signs of problems, he checks your baby’s eyes over time to see if the condition gets better or if it needs treatment.
ultrasound — A test that uses sound waves to make pictures of the inside of the body. A provider puts a special jelly on your baby’s skin over the area of the body she wants to check. Then she rolls a small device shaped like a microphone over the area. Providers often use ultrasound to check for bleeding in your baby’s brain.
urine test — Tests a baby’s urine for certain health conditions. Urine test results can tell providers a lot about your baby’s overall condition. For example, test results can tell provider if your baby’s getting enough fluid, how your baby’s kidneys are working and if your baby has an infection. Your baby’s provider inserts a thin tube called a urinary catheter in the opening where urine passes out of your baby’s body to collect the urine.
weight — Weighing your baby at birth and as he grows and develops. Providers weigh your baby soon after birth and at least once a day in the NICU. It’s a good sign when babies start to gain weight at a steady rate.
x-ray — A test that uses small amounts of radiation to take pictures of the inside of your baby’s body. X-rays show pictures of your baby’s lungs and other organs. If your baby has breathing problems, she may need several lung X-rays each day. X-rays expose your baby to radiation, but the amount is so low that it doesn’t affect her health now or in the future. Radiation is strong energy that can be harmful to your baby’s health if she’s exposed to too much.

Post-Pandemic Reentry for Teens With Social Anxiety
Recognize the warning signs of social anxiety and get help for your teen.
Posted December 20, 2022 | Reviewed by Gary Drevitch
THE BASICS
Key points
- Post-pandemic life is harder for teens with social anxiety, as restrictions that curtailed their social activities are no longer present.
- Parents can watch for a variety of signals that indicate whether their teen is struggling with social anxiety.
- Cognitive behavioral therapy is the gold standard of effective treatment and management for social anxiety.
Parents continue to grapple with the impact of pandemic restrictions on the mental health of their children. For teens, reentry into “normal” life brings a new set of challenges, especially for those prone to social anxiety. Most teens with social anxiety experienced profound relief during the pandemic because restrictions curtailed their social and performance situations. They didn’t have to face the many situations that commonly trigger their social anxiety, such as raising a hand in class, making idle chitchat with peers, attending a social event, and playing sports. However, their prolonged lack of exposure to these situations also set them back because they didn’t have the opportunity to learn and grow and discover that they can in fact handle being in uncomfortable social situations.
Teens’ anxiety about social and performance situations came roaring back with a vengeance when those situations returned to their daily lives. A national survey of U.S. teens aged 15 to 19 found that nearly half (48%) were concerned about experiencing social anxiety while transitioning back to “normal” life (Steinberg, 2021). Compared with pre-pandemic statistics, which indicated that approximately 10% of teens suffered from social anxiety (NIH, n.d.), this is a remarkable increase that deserves our attention.
In simple terms, social anxiety involves feeling extreme worry and fear related to social and performance situations. Individuals suffering from social anxiety can also fear being observed doing basic everyday activities, such as using a phone, texting, writing, using a computer, eating, or using a public restroom. Their worry and fear focus on concerns about feeling judged, negatively evaluated, and ultimately being rejected by others. Social anxiety doesn’t present the same way in all individuals, but it always exacts a big toll on the well-being of the sufferer.
How do I know if my teenager is struggling with social anxiety?
Observe your teen’s behaviors and listen to what they are saying. If you notice any of the following, your teen is likely experiencing social anxiety:
- Inordinate focus on and preoccupation with concerns about how others perceive them.
- Avoidance of social or performance situations that most peers tolerate.
- Extreme physiological reactions (e.g., sweating, shaking, nausea, hyperventilation) in performance or social situations.
- Excessive reassurance seeking and/or declarations that others perceive them as weird, odd, etc.
- Requests for special accommodations from teachers, counselors, etc. to reduce or avoid being in situations that trigger worry and fear (e.g., requests to be excused from oral presentations, public speaking, competitions, or classes or activities that others tolerate easily).
- Recess and break times spent in the library or other locations less likely to result in social interactions
- Refusal to attend parties or other events you expect your teen would enjoy, or insistence that they simply dislike these events.
- Spending time only with kids they know well.
If you observe any of the above, your teen is missing out and may need your help.
Why it’s important to get help for your teen
Untreated social anxiety is associated with depression, substance abuse, and other serious psychological problems. It can make your teen’s life miserable and limited.
Studies show that untreated social anxiety has a strong negative impact on various measures of quality of life, including academic achievement, and can interfere with people’s career paths (Vilaplana-Pérez et al., 2021). Without effective intervention, teens often come to define themselves as lacking in basic self-confidence, insecure, self-doubting, and inadequate.
These unfortunate outcomes and suffering are avoidable and repairable if the right steps are taken. Social anxiety or any other type of anxiety disorder should never define a person. These are common, highly treatable problems, just like asthma, diabetes, or allergies.
Finding treatment for social anxiety
Cognitive behavioral therapy (CBT) is the gold standard of effective treatment and management for most anxiety and related problems, including social anxiety. The basic process of CBT for anxiety disorders involves identifying distorted thinking, correcting those thinking errors, and adjusting specific behaviors. Exposures are the single most important element of successful CBT. The basic technique of exposure is to gradually face a situation that triggers anxiety, while at the same time not engaging in any safety, avoidance, or accommodation behaviors or rituals (Walker, 2021).
Finding a qualified CBT clinician, however, can be a huge challenge, and locating one who is truly experienced in CBT is not easy. You may have tried traditional talk therapy for your teen but found it ineffective. Unfortunately, after ineffective treatment, many people feel worse about themselves; like they can’t be helped. This is especially damaging to a young person developing their sense of self.
To find a therapist, visit the Psychology Today Therapy Directory.https://www.psychologytoday.com/us/blog/anxiety-relief-for-kids-and-teens/202212/post-pandemic-reentry-for-teens-with-social-anxiety

INNOVATIONS
Pioneering care for preemies – from artificial placentas to brain-healing stem cells

New treatments being developed by EU-funded researchers will improve both survival rates and the long-term health of babies born early. 11/July/24
Dr Niels Rochow is a researcher and neonatologist at Klinikum Nürnberg, in Nürnberg, Germany, one of the largest municipal hospitals in Europe.
His work, looking after newborns born early or with medical problems, keeps him very close to the topic of his research. He recalls a tense battle over the weekend to save a premature baby’s life.
‘She was born early and was in a bad state. We fought for two and a half days to keep her alive.’ The baby’s survival depended on invasive artificial ventilation technology and external lung and kidney support.
Although sometimes lifesaving, these devices were originally developed for adults and scaled down for neonatal care. They are not well adapted to a baby’s tiny body, are highly invasive and can damage immature lung tissue.
Currently, premature babies frequently need to be heavily medicated and connected to a mechanical ventilator pumping air into their lungs.
‘These babies are full of tubes and essentially paralysed,’ said Rochow. This treatment often leads to side effects and can cause chronic lung disease, impacting the child’s whole life.’
Short- and long-term impact
Every year, about 15 million babies are born preterm – classified as before the 37th week of pregnancy. A full-term pregnancy is 40 weeks, but a lot happens in those last three weeks. Currently, around 7% of births in the EU are classified as preterm.
Despite advancements in neonatal intensive care, progress in improving long-term health outcomes for these infants has been slow. Two million preterm babies lose their lives – before they even start – every year.
In fact, the Global Burden of Disease study in 2010 estimated that preterm births were the leading cause of death and disability in children under the age of five – greater than either malaria or pneumonia.
Having missed the crucial developmental milestones that normally occur in the last part of the pregnancy, survivors also have increased risks of long-term health consequences. They are more likely to suffer respiratory issues like bronchitis and asthma, and be affected by a range of neurodevelopmental disorders due to brain injury.
Like mother’s womb
Dr Rochow is one of a team of European and international researchers that received a grant through the European Innovation Council (EIC) Pathfinder programme to work on a better alternative – a system they call an artificial placenta, or ArtPlac.
The goal is to simulate the conditions of the mother’s womb, potentially reducing complications and improving outcomes for the most vulnerable newborns.
‘In the womb, the baby is connected to the natural placenta which serves as a lung, a kidney and a feeder,’ said Professor Jutta Arens, one of the lead engineering scientists working on the four-year ArtPlac project, which kicked off in 2023.
‘This placenta cannot be reconnected after birth, which is why we are developing a device that replaces its functions in the most natural way possible.’ By connecting to the baby’s belly button, the artificial placenta allows the infant to develop and heal naturally, offering a less invasive alternative to current methods.
ArtPlac will also make it easier for parents to have physical contact with their child from the start. Artificial ventilators are not only very invasive, they are also awful for parents, according to Rochow.
‘If you hear your baby cry, you want to hold it. Yet, you can’t. With ArtPlac, parents could be close to the baby and interact with it more easily.’
ArtPlac will undergo initial in-vitro testing in the last quarter of 2024. This will be followed by proof of principle in-vivo testing which will be carried out on a premature lamb. The aim is to be able to perform initial clinical trials on babies within the next few years.
Early injury, lifetime consequences
Although advances in healthcare mean that more than half of all babies born before 28 weeks survive, a large proportion of these will have a lifelong disability. Even babies born late preterm – between 32 and 37 weeks – are at increased risk.
The brain damage caused by premature birth, known as encephalopathy of prematurity (EOP), can result in long-term disorders like cerebral palsy, severely impaired cognitive functions, attention deficit and hyperactivity disorder (ADHD) and autism spectrum disorder (ASD). Brain injury can also be caused by a lack of oxygen during birth (asphyxia) or a stroke around the time of birth.
For example, it is estimated that a quarter of all cerebral palsy cases are associated with preterm birth. Diagnosing a brain injury in a preterm baby, however, is complicated and can take days to weeks. Even then, there are few options for treatment.
Dr Bobbi Fleiss is a researcher and senior lecturer at the Royal Melbourne Institute of Technology (RMIT) in Melbourne, Australia. She leads the RMIT Perinatal Brain Injury lab and is passionate about understanding injury to the brain in newborn babies and how to make outcomes for these infants better.
‘The standard procedure is applying cooling therapy, which has to happen within six hours after birth,’ explains Fleiss. ‘It is very stressful.’
Fleiss is part of a global team of researchers that received funding from the EU to develop an effective alternative treatment for preterm brain injury. Led by the French National Institute of Health and Medical Research (INSERM), the PREMSTEM project runs from 2020 to the end of 2024.
It brings together world-leading clinicians, researchers, stakeholder advocacy groups and an industrial partner specialising in neonatology and drug development from eight countries: Australia, France, Germany, Italy, the Netherlands, Spain, Sweden and Switzerland.
Brain-healing stem cells
Like ArtPlac, PREMSTEM takes its inspiration from nature’s own design. Blood that remains in the umbilical cord after birth contains a special kind of cell called a stem cell.
These cells have the ability to grow into many different kinds of cells, such as bone marrow cells, blood cells or brain cells. This makes them very valuable for treating a wide range of diseases.
PREMSTEM is using stem cells from donated umbilical cords to create a groundbreaking and easy-to-administer new treatment that could help heal neonatal brain injuries.
‘Think of stem cells as little factories that produce helpful chemicals and support the brain in helping itself,’ said Fleiss. ‘Our goal is to provide an intranasal treatment using a fine mist containing the stem cells.’
Specifically, a simple nasal spray containing stem cells is sprayed into the baby’s nose. From there, the stem cells travel to the brain, find the damaged areas and assist the brain in repairing itself.
PREMSTEM researchers have successfully tested different delivery systems, several of which have proven to be effective in reducing brain injury in animals. They expect that clinical trials testing the new treatment in human babies should begin in 2026.
The success of these projects could be life-changing for millions of babies and their families. ‘Even if we help one percent of them, it’d be wonderful,’ said Fleiss.
‘My dream is to see every baby leaving the hospital with smiling families. I hope every parent’s biggest stress will be how to strap their baby into a car seat. Nothing more.’
Research in this article was funded by the EU’s Horizon Programme including, in the case of ArtPlac, via the European Innovation Council (EIC). The views of the interviewees don’t necessarily reflect those of the European Commission.

Telehealth and high-risk pregnancy
Last updated: August 21, 2024

High-risk pregnancies can be treated and managed through telehealth as long as the patient and provider have an emergency plan in place. US Dept. Health and Human Services
What are considerations for using telehealth for high-risk pregnancies?
Telehealth can provide life-saving health care for pregnant patients. Some rural patients live far from high-risk specialists. Others can’t afford to take time off work or find childcare to go to their provider’s office. There are several ways to ensure access to high quality care for high-risk patients through telehealth.
Use remote patient monitoring
There are several devices that can monitor a patient’s health without the patient having to come into the office for multiple check ups. Remote patient monitoring can also be used to gauge whether a patient has breached the high-risk threshold, meaning it’s time to seek immediate medical care.
Pregnancy-related remote monitoring devices may include:
- Blood pressure monitors
- Blood glucose testing
- At home fetal monitors
Patients should be sent to in-person care when:
- There is decreased fetal movement
- There are known fetal abnormalities that require multiple check ups
- The patient is experiencing pre-eclampsia symptoms
- The patient is experiencing signs of early labor
Know when to seek in-person care
Part of your telehealth workflow should include a protocol for when to send a high-risk patient to the office or hospital. Some high-risk conditions, including pregnancies with multiple babies and certain chronic conditions, need more in-person oversight than telehealth can provide.
Partner with local resources for rural and underserved patients
Telehealth can be a life-saving resource and also the first line of defense for potential pregnancy complications. This is especially true for rural and underserved patients who may delay, or entirely forgo, prenatal care.
High-risk care tends to be more hands on than complication-free maternal health care. But there are many ways telehealth providers can make sure rural and underserved patients get the care they need, when they need it. Some examples include:
- Identify and partner with the patient’s local clinic or hospital. Local facilities can often provide routine testing that will help you determine the best course of care, and keep an eye on potentially serious complications. This could include baseline 24 urine collection and labs for pre-eclampsia, STI panels, blood sugar monitoring, and ultrasound.
- Work with local OB-GYNs for in-person appointments. Underserved patients may often feel more comfortable with providers that are not local to their area.
- Research local resources and online help post-childbirth. Rural and underserved parents don’t stop needing maternal telehealth care once the baby is born. Telehealth providers can help in those first few days and weeks with telehealth lactation consulting and mental health counseling. Other potential resources following high-risk pregnancies could include maternal or pediatric specialists, local and online behavioral health support, substance use counseling, smoking cessation, and parenting classes.
More information
Telehealth for chronic conditions — Health Resources and Services Administration
Statewide Telehealth Program Enhances Access to Care, Improves Outcomes for High-Risk Pregnancies in Rural Area — Agency for Health Care Research and Quality
Spotlight
Maternal Hypertension Remote Patient Monitoring Project
Using remote patient monitoring (RPM) technology, the University of Mississippi Medical Center, a HRSA-funded Telehealth Center of Excellence, is monitoring women who are at high risk for hypertension during their pregnancy. A nurse coordinator will assist the mothers in coordinating care including connecting them to community and health resources to support a healthy pregnancy. The program also provides maternal child and chronic disease management support and virtual consultations with an obstetrician in the home.
Learn more about the University of Mississippi Medical Center’s Maternal Hypertension RPM project .

Relaxation Skills for Middle School Students: How to Cope with Stress and Anxiety
YouTube Child Mind Institute Apr 27, 2023

Building Resilience: Taking Charge of Your Well-Being
Navigating life as a young person today can feel like an obstacle course of challenges, from school pressures to social expectations and the quest for personal goals. But each of these experiences is also a chance to build something powerful: resilience. Resilience is the ability to bounce back from setbacks and keep going even when the going gets tough. And the good news? It’s a skill anyone can develop with a little practice.
Set Your Own Pace
Life is not a race, despite how it sometimes feels. Take a moment to step back, breathe, and check in with yourself. How do you feel? Are you pushing too hard or not hard enough? Finding your balance is key. Try setting small, achievable goals each week that help you get closer to your bigger dreams. Remember, it’s the consistent, small steps that lead to big changes.
The Power of Positive Self-Talk
Your mind can be a powerful cheerleader—or a tough critic. What you say to yourself impacts how you feel and act, so practice kindness in your self-talk. When a mistake happens, instead of thinking, “I can’t believe I messed up,” try, “I learned something valuable here. I’ll do better next time.” Resilience isn’t about never feeling down; it’s about how you lift yourself back up.
Find Your Outlet
Everyone needs an outlet to decompress and recharge. For some, that’s going for a jog or hitting the gym. For others, it’s creating art, cooking, or simply enjoying a quiet walk. Whatever brings you joy, make time for it. Life can be demanding, but even a few minutes a day spent doing what you love will help you keep your energy up and your stress down.
Celebrate Your Wins
Often, we’re so focused on what we haven’t done that we forget to celebrate what we have achieved. Did you ace that exam, complete a project, or make a new friend? Each accomplishment is worth recognizing. Celebrating even the small victories gives you the confidence to tackle the next big thing with resilience and courage.
Building resilience takes time, patience, and practice. But with each step forward, you’re creating a stronger foundation to support you through whatever life brings your way. Keep going, believe in yourself, and know that every challenge you overcome makes you that much stronger.

Stress Management Tips for Kids and Teens!
Sep 3, 2020
Today, we will be learning all about stress! You’ll learn the definition of stress, how it affects you, and FIVE helpful ways of coping!



Mental Health Center Kids
Coping Skills For Kids – Managing Feelings & Emotions For Elementary-Middle School | Self-Regulation
Nov 6, 2022
Help children and teens learn how to manage big emotions. Emotional regulation for anger management, stress management, anxiety, depression, and coping strategies for many more mental health struggles. Provide a good foundation of coping skills for elementary and middle school students, and the same concepts can be applied to teenagers or high school students. Three Steps To Manage Emotions: 1) Notice And Identify Your Feelings 2) Think About Coping Skills You Can Use To Feel Better 3) Take Action By Practicing One Or More Coping Skill




De Colombia para el mundo. Los mejores exponentes del surf local se unieron a tres surfistas explosivos: la campeona mundial de stand up paddle Izzi Gómez, su hermano Giorgio y el panameño Oli Camarena. Dirección y Producción: Germán Bertasio. Edición: Fede Maicas. Comercial: Martín Méndez Pasquali. Productora: Mundo Zero Producciones.
































































































































 Published on Jan 31, 2019 Physician Mental Health & Suicide
Published on Jan 31, 2019 Physician Mental Health & Suicide