Yemen, officially the Republic of Yemen, is a country in West Asia. It is located in the southern end of the Arabian Peninsula, bordering Saudi Arabia to the north and Oman to the northeast. It shares maritime borders with Eritrea, Djibouti and Somalia. Covering 530,000 square kilometres (204,634 square miles) and having a coastline of approximately 2,000 kilometres (1,200 miles), Yemen is the second-largest Arab sovereign state on the Arabian Peninsula.Sanaa is its constitutionally stated capital and largest city. The country’s population is estimated to be 34.7 million as of 2023. Yemen is a member of the Arab League, the United Nations, the Non-Aligned Movement and the Organisation of Islamic Cooperation.
Since 2011, Yemen has been facing a political crisis, marked by street protests against poverty, unemployment, corruption, and President Saleh’s plan to amend Yemen’s constitution and eliminate the presidential term limit. Subsequently, the country has been engulfed in a civil war with multiple entities vying for governance, including the government of President Hadi (later the Presidential Leadership Council), the Houthi movement‘s Supreme Political Council, and the separatist Southern Movement’s Southern Transitional Council. This ongoing conflict has led to a severe humanitarian crisis and received widespread criticism for its devastating impact on Yemen’s people.
The ongoing humanitarian crisis and conflict has received widespread criticism for having a dramatic worsening effect on Yemen’s humanitarian situation, that some say has reached the level of a “humanitarian disaster”. Yemen is one of the least developed countries in the world, facing significant obstacles to sustainable development and is one of the poorest countries in the Middle East and North Africa region. The United Nations reported in 2019 that Yemen had the highest number of people in need of humanitarian aid, amounting to about 24 million individuals, which is nearly 75% of its population.
Source:https://en.wikipedia.org/wiki/Yemen
- GLOBAL PRETERM BIRTH RATES – YEMEN
- Estimated # of preterm births: UNKNOWN per 100 live births
- (Global Average: 10.6)
- Source- WHO Yemen – Healthy Newborn Network 6.8% preterm birth rate, 39% of infant mortality

COMMUNITY

Expanding capacity for publication in nursing: Experiences from a writing for publication group
Highlights
- Despite expert knowledge and expertise, nurses often do not write for publication.
- Barriers to writing for publication are commonly reported by nurses.
- A virtual, Writing for Publication Program was convened to overcome these barriers.
- The group of clinical and academic nurses successfully published a manuscript.
- Recommendations for overcoming writing for publication barriers provided.
Abstract
Nurses have valuable knowledge and expertise to share. Yet, for a variety of reasons, many nurses do not write for publication. Members in one Sigma Theta Tau International chapter requested information about publishing so a writing for publication program (WPP) was convened. Ten nurses from diverse clinical and academic backgrounds participated. The goal of the WPP was to support a small group of nurses to advance knowledge and develop practical skills through the development of a manuscript with mentorship from doctorally-prepared nurses with publishing experience. The anticipated effect was that participants would share what they learned with colleagues or mentor others to publish in the future. Beginning with informational sessions to lay the foundation for writing and publishing, the WPP included biweekly, two-hour online sessions over a seven-month period whereby individual and group writing with embedded peer and WPP leader feedback occurred. WPP participants gained proficiency in searching online databases, synthesizing published literature, and working as a member of a writing team. The group successfully published a manuscript based on a topic of interest. This current article describes the structured support and mentorship provided during the WPP with recommendations for overcoming publication barriers commonly described in the literature.
Background
Barriers to writing for publication are widely reported in nursing literature. Writing barriers are described as situational or personal (Tivis & Meyer, 2018) and internal or external (Oman et al., 2016). Situational and external barriers to writing for publication include a lack of time, family commitments, lack of resources, inadequate access to technology, insufficient organizational support, or a workplace culture that does not value writing and dissemination (Ansryan et al., 2019; Oman et
Forming the group
In August 2021, the annual general membership meeting for one chapter of Sigma Theta Tau International (Sigma) was held. Based on member requests, the educational focus of the general membership meeting, held online via the chapter’s discussion board, was writing for publication. Over the three-day meeting, those with publication experience were encouraged to share insights related to publishing. Members without publication experience reflected on publishing myths and barriers to writing for
Developing the manuscript
The goal of the WPP was to train a small cohort of nurses on how to write a single manuscript on a topic of interest and submit it to a peer-reviewed nursing journal. Wood (2018) and Bourgault (2023) note that some of the earliest decisions should be selecting the topic of the manuscript, identifying the intended audience, and selecting the journal the manuscript should be submitted. Oman et al. (2016) concur that successfully writing a manuscript is enhanced when the topic relates to lived
Reflections from group members
Two months after the second manuscript was accepted for publication, participants were asked to complete an anonymous survey to ascertain perspectives about the WPP. All ten members completed the survey. Resoundingly participants believed the WPP was a ‘well run,’ ‘helpful,’ and a ‘worthwhile’ experience. WPP leaders were ‘well prepared’ and ‘professional and skilled in guiding the process.’
The topics that members were already familiar with before participating in the WPP were writing
Lessoned learned with recommendations
Reflection by WPP leaders yielded several lessons learned with recommendations for overcoming known barriers to writing for publication. Insufficient time is frequently cited as a barrier to writing for publication (Ansryan et al., 2019). The structure of the WPP program was feasible to accomplish personal and collective goals. Two-hour, bimonthly meetings allowed sufficient time to complete the session agenda without burdening participants who may have competing work and family demands.
Conclusion
Writing for publication is an expectation of all nurses because it improves the quality of patient care to achieve optimal outcomes while also advancing the nursing profession. An innovative, virtual WPP successfully guided 10 academic and clinical nurses to publish a manuscript in a respected, peer-reviewed journal (Chargualaf et al., 2023). Participants largely reported feeling more confident in their own ability to publish in the future. Thus, the goal of the WPP was met.
Source:https://www.sciencedirect.com/science/article/abs/pii/S8755722324000267
Protecting Children and Condemning Hate During a Time of War
FROM THE AMERICAN ACADEMY OF PEDIATRICS| FEBRUARY 26 2024
American Academy of Pediatrics https://doi.org/10.1542/peds.2023-065582Board of Directors Pediatrics (2024) 153 (3): e2023065582.
The violence, suffering, and death from the terrorist attack on Israel and the Israel-Hamas War weigh on us all. Pediatricians—who are called to care for children and keep them safe and healthy—have been reaching out to the American Academy of Pediatrics expressing anguish, outrage, and a deep desire to help stop the killing, ease the suffering, and protect all children from harm.
We are shaken and pained by what is happening in Israel and Gaza, and we are also alarmed by the increasing acts of violence and intimidation we’ve been witnessing in this country toward Jews, Muslims, and those with ties to Israel or Palestine. Many pediatricians and the families they care for have experienced such incidents.
As antisemitic and anti-Palestinian hate speech have been surging on social media, acts of hate have also been increasing in the United States and around the world. There has been an unprecedented rise in incidents of antisemitism, Islamophobia, and anti-Palestinian racism in this country according to data from the Anti-Defamation League and the Council on American-Islamic Relations. And reports of violent hate crimes targeting Jews, Muslims, and Arabs have risen steeply across the United States.
As people at home and abroad confront these issues and as world leaders debate how to move forward, one thing is certain: all children affected deserve our unconditional support.
It will always be the mission of the American Academy of Pediatrics (AAP) to advocate for children’s protection, health, and safety, no matter what, no matter where—be it in the United States, Israel, Gaza, the West Bank, Ukraine, South Sudan, Armenia, Syria, Yemen, Myanmar, Ethiopia, Democratic Republic Congo, or other conflict-torn areas that receive less media attention.
As pediatricians, pediatric medical subspecialists, and pediatric surgical specialists, we understand that the profound cost of any war is measured in children’s lives—those lost to violence and those forever changed by it. We know that what happens to these children today and what we do for them will help determine what becomes of this generation tomorrow.
In 2018, the Academy published a policy statement and accompanying technical report, “The Effects of Armed Conflict on Children,” which began with the following statistic: 1 in 10 children are affected by armed conflict. By 2021, 1 in 6—or about 449 million children worldwide—were living in a conflict zone. Africa had the highest overall number of children impacted by conflict (180 million), followed by Asia (152 million), and the Americas (64 million). Today, that figure is tragically even higher.
Our policy details both the acute and long-term effects of armed conflict on child health and well-being and uses a children’s rights-based approach as a framework for the AAP, child health professionals, and national and international partners to respond in the domains of clinical care, systems development, and policy formulation.
Our policy calls on governments to safeguard children and for pediatricians and health organizations to be involved both in preventing and responding to armed conflict. It advocates for integrating core human rights principles set forth in the United Nations Convention on the Rights of the Child (UNCRC) treaty into US policy.
To fulfill these rights, the policy lays out a number of detailed recommendations for mitigating the harms of child conflict both in clinical practice and in social systems serving children. This includes ensuring child health professionals who care for children affected by armed conflict have access to training in trauma-informed care, which involves recognizing and mitigating the harmful effects of these experiences. And it highlights opportunities for public policy advocacy, which include:
- Ending the participation of children younger than 18 years of age in armed conflict and ensuring all children are protected from torture and deprivation of liberty, including extended or arbitrary detention;
- Upholding the Geneva Conventions with respect to maintaining the sanctity of safe places for children, ensuring medical and educational neutrality, and allowing children fleeing armed conflict to petition for asylum and be screened for evidence of human trafficking;
- Ensuring that children are not separated from their families during displacement and resettlement, and in the event of separation, prioritizing family reunification;
- Protecting children from landmines, unexploded ordnances, small arms, and light weapons through effective clearing efforts and strict control on their sale, ownership, and safe storage;
- Affording children a voice in creating policy and programs that prevent and mitigate harmful effects of armed conflict; and
- Providing children affected by armed conflict access to educational opportunities as part of an environment conducive to their reintegration into society.
| 2023 AAP Board of Directors | 2024 AAP Board of Directors |
| Sandy L. Chung, MD, FAAP | Benjamin D. Hoffman, MD, FAAP |
| Benjamin D. Hoffman, MD, FAAP | Susan J. Kressly, MD, FAAP |
| Moira A. Szilagyi, MD, FAAP | Sandy L. Chung, MD, FAAP |
| Dennis M. Cooley MD, FAAP | Margaret C. Fisher, MD, FAAP |
| Patricia Flanagan, MD, FAAP | Patricia Flanagan, MD, FAAP |
| Warren M. Seigel, MD, FAAP | Jeffrey Kaczorowski, MD, FAAP |
| Margaret C. Fisher, MD, FAAP | Patricia Purcell, MD, MBA, FAAP |
| Michelle D. Fiscus, MD, FAAP | Jeannette “Lia” Gaggino, MD, FAAP |
| Jeannette “Lia” Gaggino, MD, FAAP | Dennis M. Cooley, MD, FAAP |
| Gary W. Floyd, MD, FAAP | Susan Buttross, MD, FAAP |
| Martha C. Middlemist, MD, FAAP | Greg Blaschke, MD, MPH, FAAP |
| Yasuko Fukuda, MD, FAAP | Yasuko Fukuda, MD, FAAP |
| Madeline M. Joseph, MD, FAAP | Madeline M. Joseph, MD, FAAP |
| Charles G. Macias, MD, FAAP | Angela M. Ellison, MD, MSc, FAAP |
| Constance S. Houck, MD, FAAP | Kristina W. Rosbe, MD, FAAP |
| Joelle N. Simpson, MD, FAAP | Joelle N. Simpson, MD, FAAP |
In examining the entire policy in light of the Israel-Hamas War, we determined it was missing important elements to emphasize the protection of children during war and the Academy’s opposition to religious persecution of any kind. We voted unanimously to add the following to the policy statement:
- Children should never be harmed because of the religious, cultural, and other beliefs and values of the child and/or their family;
- Harm to children should never be used as a tool or tactic of war or conflict; and
- Children should be protected from the direct effects of armed conflicts and their food, housing, health, and other basic needs safeguarded.
With the magnitude of the suffering and so many children hurting at home and abroad, this is a distressing time to work in pediatrics. The pain of our members is palpable; both the urgent desire to do all we can to protect children in Israel and Gaza and the fear and concern we are experiencing as acts of hate proliferate in the United States. Yet our common mission and the outpouring of support and solidarity among our member pediatricians reminds us there is light in the darkness.
We use our platform as the world’s largest pediatric organization to speak out against violence, hate, antisemitism, Islamophobia, and enmity toward Jews, Muslims, Israelis, and Palestinians and to speak up on behalf of all children suffering in armed conflict. We stand with everyone in the pediatric profession in these times of tragedy as we continue our work of healing, protecting, and caring for the world’s children.

Woman Gives Birth To Premature Baby On Flight To Hawaii | NBC Nightly News

Social Determinants of Health and Redirection of Care for Infants Born Extremely Preterm
Jane E. Brumbaugh, MD1; Carla M. Bann, PhD2; Edward F. Bell, MD3; et alColm P. Travers, MD4; Betty R. Vohr, MD5; Elisabeth C. McGowan, MD5; Heidi M. Harmon, MD, MS3; Waldemar A. Carlo, MD4; Susan R. Hintz, MD, MS Epi6; Andrea F. Duncan, MD, MS7; for the Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network- 03/11/24
Key Points
Question How are maternal social determinants of health associated with discussions and decisions surrounding redirection of care for infants born extremely preterm?
Findings In this cohort study of 15 629 infants born extremely preterm, Black mother-infant dyads were significantly less likely to have redirection of care discussions than White mother-infant dyads, and Hispanic mother-infant dyads were significantly less likely to have redirection of care discussions than non-Hispanic mother-infant dyads.
Meaning Research is needed to understand the possible reasons and solutions for differences in redirection of care discussions for critically ill infants by race and ethnicity.
Abstract
Importance Redirection of care refers to withdrawal, withholding, or limiting escalation of treatment. Whether maternal social determinants of health are associated with redirection of care discussions merits understanding.
Objective To examine associations between maternal social determinants of health and redirection of care discussions for infants born extremely preterm.
Design, Setting, and Participants This is a retrospective analysis of a prospective cohort of infants born at less than 29 weeks’ gestation between April 2011 and December 2020 at 19 National Institute of Child Health and Human Development Neonatal Research Network centers in the US. Follow-up occurred between January 2013 and October 2023. Included infants received active treatment at birth and had mothers who identified as Black or White. Race was limited to Black and White based on service disparities between these groups and limited sample size for other races. Maternal social determinant of health exposures were education level (high school nongraduate or graduate), insurance type (public/none or private), race (Black or White), and ethnicity (Hispanic or non-Hispanic).
Main Outcomes and Measures The primary outcome was documented discussion about redirection of infant care. Secondary outcomes included subsequent redirection of care occurrence and, for those born at less than 27 weeks’ gestation, death and neurodevelopmental impairment at 22 to 26 months’ corrected age.
Results Of the 15 629 infants (mean [SD] gestational age, 26 [2] weeks; 7961 [51%] male) from 13 643 mothers, 2324 (15%) had documented redirection of care discussions. In unadjusted comparisons, there was no significant difference in the percentage of infants with redirection of care discussions by race (Black, 1004/6793 [15%]; White, 1320/8836 [15%]) or ethnicity (Hispanic, 291/2105 [14%]; non-Hispanic, 2020/13 408 [15%]). However, after controlling for maternal and neonatal factors, infants whose mothers identified as Black or as Hispanic were less likely to have documented redirection of care discussions than infants whose mothers identified as White (Black vs White adjusted odds ratio [aOR], 0.84; 95% CI, 0.75-0.96) or as non-Hispanic (Hispanic vs non-Hispanic aOR, 0.72; 95% CI, 0.60-0.87). Redirection of care discussion occurrence did not differ by maternal education level or insurance type.
Conclusions and Relevance For infants born extremely preterm, redirection of care discussions occurred less often for Black and Hispanic infants than for White and non-Hispanic infants. It is important to explore the possible reasons underlying these differences.
Fouad Abdulwahed – Habibi | Official Music Video 2023 | فؤاد عبدالواحد – حبيبي
Rotana 2,117,326 views Premiered Dec 6, 2023 #FouadAbdulwahed #Rotana2023 #Rotana
#FouadAbdulwahed #Rotana2023 #Rotana Fouad Abdulwahed – Habibi | Official Music Video 2023 | فؤاد عبدالواحد – حبيبي


Credit…Ruth Fremson/The New York Times
After Years of Decline, Premature Births Rose in the U.S.

By Alisha Haridasani Gupta Published Feb. 8, 2024Updated Feb. 14, 2024
Premature births, after years of steady decline, rose sharply in the U.S. between 2014 and 2022, according to recently published data from the Centers for Disease Control and Prevention. Experts said the shift might be partly the result of a growing prevalence of health complications among mothers.
“I’m not too surprised that these are the changes we’re seeing,” said Dr. Nahida Chakhtoura, chief of the pregnancy and perinatology department at the Eunice Kennedy Shriver National Institute of Child Health and Human Development. “We know that maternal complications have been on the rise for the same time period.”
Births before 37 weeks of gestation increased by 12 percent, though there were fluctuations during the pandemic years, with slight decreases in 2020 and 2022. Deliveries at or after week 40 declined during the study period. Increases in premature birth rates were similar across races and age groups, but the largest jump was among mothers aged 30 and above.
It is a reversal of promising trends before 2014, when premature births had been steadily declining and full-term deliveries were on the rise. Though the latest report doesn’t delve into the causes, it is “concerning,” Dr. Chakhtoura said, particularly because premature babies generally face increased risks for health complications.
One of the reasons for the rise might be that women are having babies later in life, said Dr. Vanessa Torbenson, an obstetrician and gynecologist at the Mayo Clinic in Minnesota. Older maternal age, she added, presents an increased risk of health complications that may require an early induction. Overall rates of high blood pressure in particular have been on the rise in recent years. According to the C.D.C., almost 16 percent of women who delivered in hospitals had some kind of hypertensive disorder in 2019, and those issues were most common among women 35 and older. Rates of gestational diabetes have also grown, especially among older mothers.
Generally, “the further along you go in pregnancy, the higher the chance of survival” for the baby, said Dr. Dawnette Lewis, director of Northwell Health’s Center for Maternal Health and a maternal fetal medicine specialist. Studies have found that a baby delivered at 23 weeks, for example, has a roughly 55 percent chance of survival, with chances increasing each week after that, Dr. Lewis said. The American College of Obstetricians and Gynecologists recommends inducing labor at or before 37 weeks when medically necessary.
The latest C.D.C. data is “skimming the surface,” Dr. Lewis said. One of the many unanswered questions is why there were few differences in premature birthrates across races, given that research consistently shows that rates of pre-eclampsia and hypertension are disproportionately higher among Black women. Understanding who was induced and why might shed some light on that question, she added.
Despite the concerns around later maternal age, many of the health risks can be managed, Dr. Lewis said. “Anyone who’s considering a pregnancy, regardless of their age, should see a health care practitioner so that they can be evaluated and, in case that they do have any medical conditions, that they can get those under control before attempting a pregnancy.”
Source:https://www.nytimes.com/2024/02/08/well/family/premature-births-maternal-age.html

HEALTHCARE PARTNERS
3 Organizations Providing a Free Lifeline for Healthcare Workers
By Cathy Cassata Published on May 03, 2022 Medically reviewed by Steven Gans, MD

There’s no doubt early in the pandemic, healthcare workers were pushed to their limits. Crowded hospitals required doctors and nurses to work long hours caring for patients suffering from an unprecedented and unpredictable COVID-19 virus. The pressure and demands of the situation put a physical and mental strain on those seeing patients.
According to a 2021 survey published in the Journal of General Internal Medicine of more than 500 healthcare workers and first responders, a substantial majority of respondents reported experiencing clinically significant psychiatric symptoms, including:1
- anxiety (75%)
- depression (74%)
- post-traumatic stress disorder (38%)
- recent thoughts of suicide or self-harm (15%)
To support healthcare workers’ mental health during the pandemic, many people were inspired to establish organizations. Below are three that sprung up over the past few years and continue to make a difference in the lives of doctors, nurses, and other frontline workers bearing the brunt of caring for the public during the ebb and flow of the pandemic.
Dr. Lorna Breen Heroes Foundation
Lorna Breen, MD, was a seasoned emergency room physician at New York Presbyterian Hospital in Manhattan when the COVID-19 crisis hit. In a period of three weeks, Breen treated COVID patients, contracted COVID herself, and returned to an overwhelming number of critically sick patients. At the peak of COVID, she worked 15 to 18-hour shifts with limited PPE, insufficient supplies, and not enough equipment to care for patients; some of who were dying in the hallways.
When Breen called her sister Jennifer to share that she was overwhelmed and exhausted to the point that she couldn’t get out of her chair, Jennifer and her husband Corey Feist went to Manhattan and took Breen to a mental health hospital, where she stayed for 10 days, receiving the first mental health treatment of her lifetime. A few days into her stay, Breen called her sister to express concern that her career as a physician was ruined because she was receiving mental health treatment.
When Breen returned to work on April 1, 2020, her fear continued, as she worried her colleagues would notice she couldn’t keep up. Breen died by suicide on April 26, 2020.
What Lorna was feeling is felt by doctors and nurses across the country today. The average person can ask for help, but not healthcare workers; in [several] states, they can lose their license for seeking [treatment for mental health]. That’s unacceptable.
According to a 2022 Medscape report, when physicians were asked why they have not sought help for burnout or depression, their top reasons were:2
- I can deal with this without help from a professional (49%)
- Don’t want to risk disclosure to medical board (43%)
- Concerned about it being on my insurance record (32%)
- Concerned about my colleagues finding out (22%)
After Breen’s death, the Feists went on the “Today” show to spread awareness about the mental health strain healthcare workers faced during the pandemic. After the show, they received an outpouring of support from the healthcare workforce, thanking them for sharing Breen’s story. One sentiment they heard often was the need for change when it comes to questions on licensure applications and hospital credentialing applications that ask about a person’s prior mental health
history.
The responses moved them to establish the Dr. Lorna Breen Heroes Foundation, which aims to reduce burnout of healthcare professionals and safeguard their well-being and job satisfaction by:
- Advising the health care industry to implement well-being initiatives
- Building awareness of these issues to reduce the stigma; and
- Funding research and programs that will reduce health care professional burnout and improve provider well-being.
“While Lorna is our beacon and inspiration, we started the organization because we heard from the
healthcare force (hundreds) after she died that something needed to change,” said Feist. “Now, what we have is a huge subsection of our healthcare workforce who has experienced repetitive trauma for two years. For some of them, this has been 9/11 every day for two years, and because of their fear of repercussions to continue working, they are going to suffer in silence.”
On March 18, 2022, the foundation’s work helped pass the Dr. Lorna Breen Health Care Provider Protection Act, which establishes grants and requires other activities to improve mental and behavioral health among healthcare providers.
The more we talk about mental health, the more we normalize it and give others permission to speak. Lorna was the toughest person I knew in the world and she was a seasoned physician in New York. She worked through Ebola in New York and other crises. This wasn’t about being tough.
He added that many solutions to the problem are complex, but that small actions can help.
“[Like] someone being vulnerable and recognizing the need for self-care, and peer support (recognizing a colleague who needs support) that don’t cost money. We need to make it clear that you care for yourself and colleagues just as you would your patients,” he said.
The foundation’s next mission is to raise awareness among medical licensing boards, nursing boards, and hospital systems about the impact of including mental health questions on applications. They hope licensing boards will change questions to reflect current mental health impairment and exclude past ones.
“We are asking all hospitals in this country to simply publish to their workforce that they can
get mental health support without repercussions, which can be a life-saving opportunity for all of the healthcare community,” said Feist.
The Emotional PPE Project
In March 2020, Ariel Brown, PhD, neuroscientist, was talking to her neighbor and friend Daniel Saddawi-Konefka, MD, critical care physician and anesthesiologist at Massachusetts General Hospital, when she was moved to help with the COVID crisis.
“Dr. Dan…is responsible for directing [about] 100 anesthesiology residents and was struggling with the best way to support them during the onslaught of COVID,” said Brown. “I wanted to help and so I put out a call on social media to see if any of the therapists in my network wanted to volunteer some of their time to help these folks who were fighting on the frontline of the pandemic.”
The therapists raised their hands in droves to offer free therapy to healthcare workers. When
Brown passed on their contact information to the residents, many reached out to therapists for help
at a no-cost, no-insurance, streamlined option for healthcare workers to seek mental health care.
Because of the goodwill of the mental health provider community and because of the great need in the healthcare worker community, things grew very quickly. I put together a team, which I led to set up to be able to scale. Two years later, we are a national nonprofit organization that has over 700 volunteer therapists and has served over 2,000 healthcare workers across the nation.
Over the course of the pandemic, she has learned that healthcare workers face significant barriers to getting support for their mental health. The Emotional PPE Project is designed to streamline mental health service by lifting barriers, including:
- Financial: Facilitating services at no cost and with no insurance.
- Access: A streamlined process to connect with therapists
- Stigma: Remaining 100 percent confidential and unaffiliated with any organization that employs healthcare workers
“Overall, we seek to take away every barrier that we can so that the folks experiencing unprecedented stress and trauma can have a streamlined connection with someone that can help,” said Brown.
The Emotional PPE Project is also involved in research and advocacy work similar to that of the Dr. Lorna Breen Heroes Foundation, including working to reform licensing practices to protect the mental health of physicians.
- Healthcare workers, find a therapist in The Emotional PPE Project directory
- Licensed therapists, sign up to volunteer your time
- Anyone, support the organization by making a tax-deductible donation
Therapy Aid Coalition
As the world started to shut down due to COVID-19 in March of 2020, Jennifer Silacci, LCSW, psychotherapist, felt grateful she could work from home and shelter in place although anxious about the virus.
I wondered, if those of us at home felt so overwhelmed, how were those on the frontlines coping? How were they processing the anxiety around constant exposure to a potentially deadly virus? And what could I do to help them?
She decided to offer free and low-cost therapy sessions to healthcare workers and asked her colleagues if they would join her. Word spread, and before she knew it, thousands of volunteer therapists from across the country joined Silacci.
“Quite honestly, I had no idea how to manage this new, growing network of volunteers, or the thousands of emails pouring into my inbox, so I asked everyone I could think of for help. Childhood friends and even some kids I babysat (now adults) stepped up. A friend connected us with her law firm, and soon we were a fully formed 501(c)(3) public charity,” she said.
Within months of putting out the initial call, Silacci established the Therapy Aid Coalition,
now made up of over 3,000 licensed therapists, who offered free and low-cost online therapy to essential workers in the United States.
Because confidentiality is a concern for many healthcare professionals, and many do not want to utilize employee assistance programs (EAPs), health insurance, or support and resources from their hospitals and clinics, Silacci said her service offers them the opportunity to connect with a therapist anonymously. Over the past two years, the program has served thousands of essential workers throughout the country.
“I think the pandemic and the amazing work of so many nonprofits…have shed light on the need for mental health support, destigmatization, and advocacy for mental wellness within the healthcare professions,” she said.
Because the Therapy Aid Coalition continues to receive hundreds of requests monthly, Silacci said, normalizing the fact that healthcare professionals “while perhaps heroic in their actions—are still painfully and beautifully human” needs to become more understood.
“We all have a breaking point. It is my belief that individuals that have been on the frontlines may not even fully realize the impact of their experience just yet. Some are still running on adrenaline. Some are still numb and just trying to make it through another shift,” she said. “I believe we will see a greater need for mental health support among frontline workers in the next year or two, as they finally come up for air, and have the time and space to unthaw, and digest all that has unfolded.”
Those affected also include mental health professionals, Silacci added, and taking care of therapists is also one of her objectives. While the Therapy Aid Coalition currently offers free and low-cost services, it plans to pay therapists via stipends as it accumulates grants.
Those affected also include mental health professionals, Silacci added, and taking care of therapists is also one of her objectives. While the Therapy Aid Coalition currently offers free and low-cost services, it plans to pay therapists via stipends as it accumulates grants.
“We want services to be free to essential workers, but we also believe it is absolutely not fair to ask therapists to continue to offer pro-bono sessions two years into the pandemic,” she said. “[Therapists] are essential workers, and also qualify for free short-term sessions with us!”

How Generative AI Will Change The Jobs Of Doctors And Healthcare Professionals
Bernard Marr/Contributor

The roles of professionals in society are shifting thanks to the development of truly useful and powerful generative artificial intelligence. Every industry will be impacted, but we have already seen that healthcare, with its heavy use of data and technology, will be disrupted more than most.
Generative AI has the potential to revolutionize the way we treat disease, develop new medicines and personalize treatments to fit individual patients. It will also fundamentally change both the day-to-day working lives of doctors, nurses and other clinical health professionals and even the way they are seen by society. As a result, they will find they are more reliant than ever on the human qualities like compassion, communication and the instinct that many who fill these jobs have for providing care.
So here’s my overview of some of the most dramatic and meaningful transformations we can expect to see in the near future, as well as some of the practical and ethical challenges that will have to be overcome.
AI As A Diagnostic Assistant
Generative AI helps with diagnosing conditions by interpreting data and providing clear, in-depth insights into what is known about the patient. It can be used to examine hundreds of X-ray, MRI and CT scans and quickly give a statistical summary of its findings. This will lead to more accurate, data-driven diagnosis of many common or not-so-common conditions.
This communication can then be fine-tuned depending on the role of the healthcare professional who is using it, whether a doctor, nurse, consultant or specialist. Communicating only the insights relevant to them means there will be less noise between the professional and the specific information they need.
The World Economic Forum has also predicted that generative AI will lead to improved outcomes as it becomes able to efficiently extract data from the many disparate and siloed sources that have traditionally existed across healthcare.
It will also increasingly be used to create synthetic data, which is artificially generated to resemble real-world information. This is particularly useful for situations with limited training data, such as with rare conditions and diseases. It can also reduce the security and data protection measures that healthcare professionals must take when working with real patients’ personal data. Synthetic data can also be used to simulate healthcare scenarios like pandemics or the emergence of antibiotic-resistant organisms that could cause a global healthcare crisis.
Automating Routine And Administrative Tasks
It will become increasingly common for medical professionals to use generative AI to automate many of the repetitive and routine administrative tasks they carry out every day. This will free up their time to focus on directly providing care, as well as continuing their training and learning.
From managing and updating patient records to scheduling appointments, healthcare professionals engage in many time-consuming tasks that can be streamlined or even entirely taken over by AI. According to one study, doctors spend half of their working day on tasks involving maintaining electronic health records.
Generative AI can drive more efficient EHR management by intelligently organizing doctors’ notes, test results and medical imaging. It can then provide quick summaries of individual patients, highlighting aspects of their health that are a concern and generating reports for other professionals. Automating many of these tasks is likely to also have the effect of reducing errors that could impact quality of care and patient outcomes.
Generative AI In Drug Discovery
The same capabilities that allow generative AI to create text and writing can also be used to develop new candidate medicines and vaccines for clinical trials. This means that researchers can speed up the lengthy process of shortlisting potential candidates.
Last year, Oxford-based biotech firm Etcembly produced the first immunotherapy drug created with the help of generative AI.
The process promises to speed the transition of potentially lifesaving new treatments from lab to patient, ultimately leading to better patient outcomes. This indicates that just like doctors and nurses, healthcare researchers and scientists will also have powerful generative AI tools to enable them to work more quickly and efficiently.
Ethical Consideration: The Human Touch
Clearly, however, integrating generative AI into healthcare in this way creates a long list of ethical challenges that can’t be ignored. This is because most use cases revolve around the use of personal data. This means that safeguarding against data leaks, losses and breaches is of paramount importance.
It’s also essential that AI algorithms make decisions that are transparent and explainable—this will be crucial for building the public trust essential for these systems’ potential to be realized.
The damage that can be caused by bias in data is also more pronounced than in nearly any other field. Its been shown that generative AI models can amplify bias present in training data. We know that women and people from minority ethnic backgrounds are more frequently diagnosed due to their underrepresentation in medical studies, and this issue could scale as AI becomes more widely used.
Data, models and outcomes must all be continually monitored and updated in order to mitigate these biases, which could otherwise further perpetuate inequalities.
Like many other professionals, those in healthcare will find themselves required to learn the skillset of the AI ethicist. This means developing the capability to evaluate potential use cases in order to determine whether applying AI is likely to cause damage, risk or danger, and ensuring adequate guardrails are in place at all times.
The Future Of Doctors And Healthcare Workers
Doctors, nurses and other clinical healthcare professionals are probably more insulated than many from the risks of being replaced by AI. Their jobs require them to function at an advanced level across many human skills that machines will not replicate any time soon. Intuition and experience all play a role, and that isn’t going to change.
AI does, however, offer the opportunity for these professionals to redefine the way they work and even their role in wider society. Shifting to models of work that allow them to spend more time with patients will also mean more time to continue their ongoing education and develop their own medical expertise.
This is likely to lead to new specializations as the need grows for clinical staff focused on AI-enhanced diagnoses, data-driven medicine and ethical AI, as well as helping patients navigate the range of new AI-assisted treatment options that will become available.
With AI handling routine analysis, record keeping and interpretation of scans, imaging and other data, doctors and nurses will spend more time getting to the bottom of more complex and nuanced patient issues.
Ultimately, the essence of providing healthcare will continue to revolve around empathy, compassion and the human touch. Generative AI creates the opportunity to augment these qualities in ways that will make professionals in this field even more essential to society. Those who are able to embrace this paradigm shift will find they are able to use their skills and training to cure sickness and improve patient lives in ever more rewarding ways.

Neonatal Neurocritical Care: Past, Present and Future – Fernando Gonzalez, MD (11/13/2023)

Dec 15, 2023
Title: Neonatal Neurocritical Care: Past, Present and Future Speaker: Fernando Gonzalez, MD Co-Director, UCSF Neuro-Intensive Care Nursery Director, Residency Molecular Medicine Track Co-Leader, SPR Pediatrician-Scientist Development Professor of Pediatrics, University of California, San Francisco Presented by leading researchers from UCSF Pediatrics, from other departments at UCSF and outside institutions, Frontiers in Child Health Research is an interactive series meant to facilitate scientific exchange and stimulate new ideas.


Skin-to-skin transfer from the delivery room to the neonatal unit for neonates of 1,500g or above: a feasibility and safety study

Front. Pediatr., 20 March 2024 Meline M’Rini* Loïc De Doncker Emilie Huet Céline Rochez Dorottya Kele Neonatal Department, Hôpital Universitaire de Bruxelles, Hôpital Erasme, Université Libre de Bruxelles, Brussels, Belgium
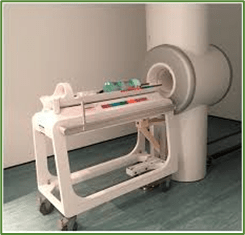
Objective: Immediate skin-to-skin contact (SSC) is already standard care for healthy term newborns, but its use for term or preterm newborns requiring admission to neonatal intensive care unit (NICU) with or without respiratory support is challenging. This study aimed to assess the safety and feasibility of SSC during the transfer of newborn infants, using a new purpose-built mobile shuttle care-station, called “Tandem”.
Material and methods: A monocentric prospective observational study was conducted at the tertiary referral center of the Université libre de Bruxelles in Brussels, Belgium after ethical approval by Hopital Erasme’s Ethics Committee (ClinicalTrials.gov ID: NCT06198478). Infants born with a birth weight above 1,500 g were included. Following initial stabilization, infants were placed in SSC with one of their parents and transferred to the NICU using the Tandem.
Results: Out of 65 infants initially included, 64 (98.5%) were successfully transported via SSC using the Tandem. One transfer was not successful due to last minute parental consent withdrawal. The median (range) duration of continuous skin-to-skin contact after birth was 120 min (10–360). SSC transfers were associated with gradually decreasing heart rate (HR) values, stable oxygen saturation levels (SpO2), and no increase in median fraction of inspired oxygen (FiO2). Heatloss was predominantly observed during initial setup of SSC. There was no significant difference in the occurrence of tachycardia, desaturation or hypothermia between preterm and term neonates. No equipment failures compromising the transfer were recorded.
Conclusion: Skin-to-skin transfer of infants with a birthweight of equal or above 1,500 g using the Tandem shuttle is feasible and associated with stable physiological parameters. This method facilitates early bonding and satisfies parents.
Clinical Trial Registration: ClinicalTrials.gov (NCT06198478).https://www.frontiersin.org/articles/10.3389/fped.2024.1379763/full

PREEMIE FAMILY PARTNERS
© Pexels/Hussein Altameemi
The fasting month of Ramadan: Does intermittent fasting of pregnant women influence the risk for preterm birth?

POSTED ON 18 MARCH 2024
Fasting during Ramadan is a valuable experience for Muslims all over the world. Even though it is not compulsory for pregnant women to participate in fasting, many choose to do so. However, the question arises as to whether abstaining from food and water throughout the day could have an impact on the well-being of the unborn child. To answer this question, fourteen studies from seven countries were reviewed, involving more than 2,800 expectant mothers. The results show that Ramadan fasting influences neonatal weight and other parameters of foetal health. However, most of the effects, including the risk for preterm birth, were found to be non-significant. This indicates that fasting during Ramadan is not harmful for the baby overall, and that the decision to participate in Ramadan fasting should therefore be left to the mother.
Ramadan is a month focusing on prayer, community, and reflection for all Muslims around the world. Central to this is the Ramadan fasting (RF), which is a form of intermittent fasting in which no food or water is consumed from sunrise to sunset. The abstinence from water during the fasting period makes RF more intense compared to other forms of intermittent fasting. While RF is obligatory for healthy Muslims, breastfeeding mothers and pregnant women are exempt from fasting and can decide for themselves whether they feel fit enough to participate or not. The Muslim population makes about ¼ of the world’s population, and accordingly many pregnant women face the question if they can participate in RF without harming the foetus. This concern arises from the fact that an adequate supply of nutrients is important to meet the needs of both mother and foetus, and neonatal weight is a direct indicator of the foetus’ wellbeing.
A total of 14 studies from seven countries examined the topic and the results were analysed in an overall review. The 2,889 participating mothers lived in Turkey, Iran, Lebanon, Pakistan, the UK, the Netherlands, and Saudi Arabia.
Ramadan fasting has a significant influence on birth weight
Several different measurements indicate foetal health and can be used to analyse the effects of RF on the unborn child. One indicator is neonatal weight. The findings varied in the different studies examined, but the overall effect showed a significantly lower birth weight in fasting mothers. The amniotic fluid index (AFI), a standardised indicator of foetal well-being, also showed a significant effect. The combination of dehydration during RF, longer daytimes, and temperatures above 36°C led to a reduction of the AFI in fasting mothers. Further significant correlations were found between RF and foetal femur length and RF and lower biparietal diameter assessing foetal size in fasting mothers.
The results on gestational age at delivery were contradictory but insignificant altogether. When analysing the impact on preterm birth (PTB), only one study showed a slightly increased incidence of PTB when the mother was fasting. The increase was not statistically significant and all other studies that examined PTB reported no association, leading to the redeeming conclusion that RF has no effect on the likelihood of PTB.
Various other measures showed no significant impact of RF on foetal health, including foetal body weight, length, head circumference, and abdominal circumference of the infant. The biophysical profile also did not change for fasting mothers, nor did the foetal movements, breathing movements, tone, amniotic fluid volume or the Apgar Score.
Fasting for expectant mothers is not harmful to neonatal health overall
Although RF affects foetal growth, it is not associated with poorer neonatal health. The negative associations between fasting and foetal well-being were stronger when the mother fasted during the second or third trimester of her pregnancy. Furthermore, all associations between RF and reduced health were predominantly found in lower quality studies, which supports the evidence that fasting is safe for pregnant women. Thereafter, current scientific evidence shows that fasting during Ramadan is not harmful to the foetus and can be practiced by pregnant women. The decision to fast should therefore be made by the pregnant woman herself, in consultation with her doctor, who will take her individual health status into account. The wellbeing of the foetus depends more on the type of food the mother eats during the fast-breaking period of Ramadan.
Source:https://www.efcni.org/news/does-ramadan-fasting-influence-risk-for-ptb/
Trauma in infancy can have a lingering effect throughout life

In adulthood, these children “are more vulnerable to stress-related health outcomes, like diabetes, and mental health issues, addiction and obesity,” one expert says
By Katie C. Reilly – March 20, 2022
Are infants too young to experience and remember painful emotions or traumatic events? A growing body of research suggests no, and researchers believe that if left untreated, trauma experienced in infancy can sometimes result in lifelong health consequences.
Beyond such obvious triggers as war and terrorism, exposure to domestic violence, natural disasters such as a house fire, physical abuse and community violence are examples of experienced events that can be traumatic for infants, experts say.
Experts in infant mental health, which goes from the prenatal period up to age 3, say that babies and very young children who experience such things have higher incidences of anxiety disorders or depression that can persist into adulthood if left untreated.
“It is easy to assume that babies don’t remember trauma because they express their experiences differently,” Tessa Chesher, an clinical assistant professor of psychiatry and behavioral sciences at Oklahoma State University who specializes in infant and early childhood mental health, says in an email. “At [8 to 12] weeks of age, babies have stored enough memories that [the babies] start to anticipate their caregiver’s behavior based on previous behaviors. They start to respond based on the experiences they have had.”
‘Vulnerable to stress-related illnesses’
Evelyn Wotherspoon, a social worker specializing in infant mental health, said that as they reach adulthood “infants and very young children who have had early exposure to trauma and chronic stress … are more vulnerable to stress-related health outcomes, like diabetes, and mental health issues, addiction and obesity. These children are much more vulnerable to all of these stress-related illnesses, and their brain may not develop the way it should.”
Although infants and young children are just developing, experts in infant mental health say they can experience a wide range of feelings that includes negative emotions, sadness or anxiety. A report by the American Academy of Pediatrics found that, by age 16, more than 2 in 3 children had said they had experienced a traumatic event.
According to a Report of the Task Force of the World Association for Infant Mental Health, rates of mental health disorders in infancy (which generally includes birth to age 3) are comparable to that of older children and adolescents. And one small study of 1-year-olds found that 44 percent of those who had witnessed severe violence against their mother by an intimate partner showed symptoms of trauma afterward, such as increased arousal, increased aggression or an interference with normal infant development. Infants and young children (under age 4) can develop post-traumatic stress disorders after events, according to a study in the Journal of the American Academy of Child & Adolescent Psychiatry.
Kathleen Mulrooney, a counselor who is also program director for the Infant and Early Childhood Mental Health Program for Zero to Three, a nonprofit organization dedicated to improving the lives of babies and toddlers, said it’s important to note that not every infant who experiences a trauma will be traumatized. As with adults, it depends on the infant, “because what is traumatic for one person is not for someone else,” Mulrooney says.
“To be traumatized, one must be severely frightened,” says Charles Zeanah, a psychiatrist and the executive director of the Institute of Infant and Early Childhood Mental Health at Tulane University School of Medicine. Infants under 12 months may not always be aware that a particular situation is actually dangerous, which can potentially protect them from trauma, he says.
Caregivers can be key
In this context, caregivers can be key in buffering small children from the effects of trauma by how they react. “The ability of parents or key caregivers to provide protection, to have a co-regulating role when it comes to the stress response is critical,” Mulrooney said in an email.
If a child has a significant trauma before age 2 but following the trauma “the baby has the powerful protective factors of consistent safety, love and security; there is a decreased likelihood of having mental health problems,” Chesher says in an email. “That doesn’t mean the baby didn’t suffer or that their body doesn’t remember that trauma, it means that there were protective factors around to mitigate the effects of the trauma.”
Regina Sullivan, a developmental behavioral neuroscientist and professor of psychiatry at NYU Grossman School of Medicine, says that while a primary caregiver cannot “buffer a small child from trauma in the environment — it’s called social buffering because the child’s fear response and stress hormone response is reduced — more recently, we have shown that the caregiver is actually blocking neural activity in the amygdala, the brain area responsible for fear.”
Trauma in infancy can physically alter the developing architecture of the brain, according to the American Academy of Pediatrics. Toxic stress — strong, frequent or prolonged adversity — has been shown in various studies to harm learning capabilities, memory and executive functioning.
“Many brain areas in infants and small children are physically altered and the ability of those brain areas to talk to one another is also modified by trauma,” said Sullivan.
Trauma can be difficult to recognize
Yet trauma in infancy can be difficult to recognize given that infants are not yet verbal and rely on their caregivers to respond to their needs, which means a caregiver would have to be attuned to symptoms and seek help.
“A baby can’t just go up to you and say, ‘Hey this happened yesterday, I’m scared,’ Chesher says. “And so really learning the language of the babies is important and then educating people on how to read that language. And so, if we don’t know the red flags, then we are not identifying trauma and we can have longer term effects on the brain.”
Experts say some red flags of trauma for babies younger than 12 months are: feeding or sleep problems and not being able to be comforted by their caregiver. A toddler (between ages 1 and 3) can express themselves more verbally and physically than a baby. Some red flags of trauma in that age group can involve repeating traumatic events in their play or becoming aggressive, Chesher says.
“One of the issues is how that child expresses trauma might be through disruptive sleep or being a bit fussier,” Sullivan says, “things that occur in normal children for a host of many reasons, which makes it difficult to identify which child is going to respond to the trauma in a way that will be long lasting and damaging.”
If a parent or other caregiver is concerned, based on a child’s behavior and experiences, they should “ask to be referred to an infant and early childhood mental health specialist,” Chesher says.
Experts will look at a variety of factors, with the most critical being the relationship between the baby and their primary caregiver. In addition to observing that interaction, mental health experts may also look at “pregnancy history, birth history, medical history, development history, safety screeners, perinatal depression screener [for both parents], how the infant eats and how the infant sleeps,” Chesher says.
Different interventions
Depending on a child’s age, different interventions are available, including child-parent psychotherapy.
“It is essential that the parents or … their caregivers … are involved in a major way in the treatment because it is really through relationships with caregiving adults that infants thrive and do well,” Zeanah says.
To recover, an infant needs a caregiver in their life who can accurately read their cues and respond in a nurturing, patient manner, Wotherspoon says. “One of the most powerful therapeutic tools that we have is the relationship a child has with a nurturing caregiver and they only need one and it doesn’t have to be perfect. … An infant who gets that fairly early on can recover beautifully from trauma,” Wotherspoon says.
Increasing awareness about infant and early childhood mental health among both parents and medical practitioners is critical, experts say. But it’s also important for parents to understand what trauma is — and is not. A child “getting distressed is different than being traumatized,” Zeanah says.
“It’s important to distinguish from everyday events that might scare the child and are important in the child learning how to regulate their emotions and physiology versus trauma from horrible events such as a tornado or a parent who is repeatedly traumatizing the child unnecessarily through verbal or physical assaults,” Sullivan says.
“We want parents to enjoy this time in their life and not be fearful that they are going to traumatize their child by making them eat vegetables or get vaccinated,” she adds. “Those are normal experiences in life that the child needs to experience as part of [the] current world.”
Source:https://www.washingtonpost.com/health/2022/03/20/infant-trauma-stress-mental-health/

INNOVATIONS

NIU researcher’s innovation helps lead to device to prevent hearing loss in NICU infants
August 28, 2023
DeKalb, IL – Technology developed by NIU Electrical Engineering Professor Lichuan Liu and designed to prevent hearing loss in the most vulnerable of newborns could soon find its way into hospital neonatal intensive care units, or NICUs
NICUs can be noisy. The care units are louder than most home or office environments and have sound levels that often exceed the maximum levels recommended by the American Academy of Pediatrics. Hearing impairment is diagnosed in 2% to 10% of preterm infants, versus 0.1% of the general pediatric population.
Aiming to put her electrical engineering expertise to use to benefit others, Professor Liu invented an apparatus, system and method to significantly reduce harmful noises while maintaining communication between the newborns and their parents or caregivers.
In 2014, NIU began a partnership with Invictus Medical, a Texas-based medical device company, to commercialize the technology. NIU licensed its related patents to Invictus, while the company has continued to refine the incubator-based active noise control (ANC) device, now known as the Neoasis®.
In July, Invictus announced that the company had received a U.S. Food and Drug Administration (FDA) clearance-for-use declaration for the device.
The control unit front face and home screen on the Invictus Medical Neoasis® incubator-based active noise control (ANC) device. Photo courtesy of Invictus Medical
“With this clearance for use, Invictus has made a huge step towards deploying the Neoasis® ANC device in neonatal intensive care units,” said George Hutchinson, Ph.D., Invictus Medical’s chief executive officer. “It is well documented that a quieter environment has a positive impact, including improved sleep hygiene and weight gain in infants where both are critical for development.
“The NIU team has been a pleasure to work with,” Dr. Hutchinson added. “The Office of Innovation has been a great teammate throughout the entire process.”
The Neoasis® ANC device utilizes a proprietary, innovative active noise control (ANC) system to attenuate noise with canceling sound wave technology. At the same time, it allows a parent’s voice to be directed to the infant, which can also be beneficial for cognitive development. Invictus is currently exploring relationships with strategic partners to get the Neoasis® ANC device into NICUs—now possible with the FDA clearance.
While universities and researchers can realize typically modest financial benefits from technology transfer, the primary intent is to broaden the potential impact of research through the creation of innovative products and services for public benefit, said Karinne Bredberg, director of NIU’s Office of Innovation. The office has guided Liu through the partnership, patent processes and licensing.
“This is a big deal for Dr. Liu and for NIU,” Bredberg said.
“NIU research has produced other patents and licenses, but we believe this is the first NIU-licensed technology to be incorporated into a device that has an FDA clearance-for-use declaration,” Bredberg said.
Mark Hankins, NIU’s assistant director for technology transfer, credited the ingenuity of Professor Liu, as well as a great working relationship with Invictus Medical.
“Dr. Hutchinson in particular was very diligent in trying to move this technology forward and persevered through a number of roadblocks,” Hankins said.
Professor Liu said it was about a decade ago when President Lisa C. Freeman, then serving as NIU’s vice president for Research and Innovation Partnerships, brought Liu together with Invictus Medical. While Liu developed an initial prototype, the company refined the device, making the it more commercially accommodating for NICU environments.
“It’s a little different working with industry, as opposed to academia,” Professor Liu said. “It was a learning curve for me, but Invictus Medial has been very professional and easy to work with.”
NIU Professor Lichuan Liu is now conducting research on an artificial-intelligence algorithm that can detect the meaning behind babies’ cries.
Over the years, the commercialization process received funding support from the NIU Foundation and a National Science Foundation’s (NSF) Small Business Technology Transfer grant. Liu, herself a mother of two, is excited at the prospect of hospitals using the Neoasis® ANC device.
“I think this is fantastic,” Liu said. “I kept working on this project and thought someday there would be payback.
“I have a passion or motivation to work to benefit others,” Liu added. “As a mom, I think this device is really something important. As an engineer, I’m happy to make an impact.”
Liu said her current research includes other ways to use noise cancellation. She is working on a pillow that would cancel out the racket of snoring, and she and NIU Nursing Professor Jie Chen are working on a system for adult intensive care units.
Additionally, Liu is working on an artificial intelligence algorithm that can listen to infant cries and determine whether they are normal or abnormal to potentially indicate a severe or chronic illness. Invictus might incorporate the technology into future versions of its Neoasis® ANC device.

Multisensory stimulation and its effect on breast milk volume production in mothers of premature infants

Carla Madeleine Cuya1* Carlos Barriga2 Maria del Carmen Graf3 Mirta Cardeña1 María del Pilar Borja1 Richard Condori4 Moises Azocar5 Carlos Cuya4
Introduction: In a significant number of NICUs, mothers are unable to provide enough maternal milk to feed their premature babies, so healthcare workers rely on human milk banks. Unfortunately, this service is not available in many countries, such as Peru, where premature infants receive formula. The aim of this study was to determine the effectiveness of multisensory stimulation on mother’s own milk production.
Methods: Participants in this study were postpartum mothers of preterm infants 27–37 weeks gestational age. The participants were assigned to three groups: (1) audiovisual stimulation (SAV) (n = 17), (2) audiovisual and olfactory stimulation (SAVO) (n = 17), and (3) control (n = 16). A questionnaire was used to collect demographic and obstetric data, including a record of mother’s own milk volume.
Results: There was no significant difference between the SAV, SAVO and control groups regarding age, marital status, education level, occupation, number of children, mode of delivery, Apgar and birth weight. On the other hand, a significant difference was observed between the SAV and SAVO groups regarding the amount of milk produced, with higher production between the fourth and seventh day (Tukey p < 0.05). Similarly, milk volume was significantly greater in the SAVO group compared to the SAV and control groups (OR = 1.032, 95% CI = 1.0036–1.062, p < 0.027).
Conclusion: Multisensory stimulation in postpartum mothers of preterm infants caused an increase in the volume of mother’s own milk production. However, more research is needed to explain the findings presented in this study.
Front. Pediatr., 14 March 2024
Volume 12 – 2024 | https://doi.org/10.3389/fped.2024.1331310

Advanced imaging and modeling in neonatal simulation
Jennifer Arnold, Niranjan Vijayakumar, Philip Levy
Abstract
Advances in modeling and imaging have resulted in realistic tools that can be applied to education and training, and even direct patient care. These include point-of-care ultrasound (POCUS), 3-dimensional and digital anatomic modeling, and extended reality. These technologies have been used for the preparation of complex patient care through simulation-based clinical rehearsals, direct patient care such as the creation of patient devices and implants, and for simulation-based education and training for health professionals, patients and families. In this section, we discuss these emerging technologies and describe how they can be utilized to improve patient care.
Introduction
Simulation is a powerful tool for improving education, patient safety, and innovation in any field of medicine.1 In neonatology, the opportunity to create realistic simulations to help prepare clinicians for high risk care of vulnerable patients is paramount.2 As the field of healthcare simulation advances, technologies for simulation are diversifying. With advances in modeling and imaging, broader and more realistic tools for education and training, and even opportunities to improve direct patient care are emerging. These include realistic models for preprocedural planning and clinical rehearsals, and innovative, bespoke patient specific devices and healthcare tools to use in clinical care. Current advances in specific technologies have allowed for this expansion, including point-of-care-ultrasound (POCUS), three dimensional (3D) and digital anatomic modeling, and extended reality technologies that are immersive digital recreations of reality, such as virtual reality (VR), augmented reality (AR), and mixed reality (beyond the scope of this article). In this article we review the types of imaging and modeling technologies available and how they can be applied to improve neonatal patient care and outcomes through healthcare simulation-based education (SbE), clinical rehearsals(SbCR), and more.
Section snippets:
Point-of-care ultrasound (POCUS)
POCUS, which is ultrasound performed and interpreted in real time by bedside clinicians, has been used by adult and pediatric specialties for many decades, with recognition that this technology may enhance quality of care and improve patient outcomes.3 Pediatric anesthesiology and adult emergency medicine were early adopters of POCUS, and pediatric critical care has increasingly utilized POCUS for central line placement and diagnostic imaging.4 POCUS has more recently been utilized in
Applications of imaging and modeling
The types of imaging and modeling described above are emerging tools now available in healthcare that can be applied in three specific ways: preparation for complex patient care through SbCRs, direct application for patient care, and simulation-based education and training.
Patient specific simulation-based clinical rehearsal (SbCR)
Simulation-based Clinical Rehearsal (SbCR) refers to the practice and rehearsal by clinicians to prepare for a patient-specific procedure or complex care process before providing direct patient care. These are typically rehearsed using physical 3DP or virtual models. SbCRs can be patient-specific (utilizing the patient’s exact anatomical data to create a model for rehearsal, such as practicing a specific congenital heart disease [CHD] repair on a 3DAM before operating on the patient) or
Imaging and modeling in direct patient care
While using immersive technologies as a part of the preparation for patient care is exceedingly valuable, there are additional applications as part of healthcare services provided directly to patients. In the next section we describe how 3DP, POCUS, and virtual modeling improve care delivery in neonatology and other fields of medicine.
Imaging and modeling in simulation-based education and training
Imaging, modeling and other emerging technologies are used in the education of healthcare professionals and patients, families, and other home caregivers. 3DAMs have been shown to improve performance and promote competency-based education. The benefits of 3DP in education include on demand reproducibility, the possibility to model different physiologic and pathologic anatomy from an endless dataset of images, and the possibility to share 3D models among different institutions.56 3DP has
Conclusion
In conclusion, imaging and modeling technologies have significantly advanced healthcare, including neonatal care. These technologies have enhanced education and training for all levels and types of learners, enabled better preparation and rehearsal for complex care, augmented diagnosis and applications of personalized treatment plans, and improved patient outcomes. From ultrasound to physical models to sophisticated virtual models, these tools provide invaluable insights into the delicate care.
Source:https://www.sciencedirect.com/science/article/abs/pii/S0146000523001283?via%3Dihub
Point-of-care MRI heads to the NICU for imaging infants

Casey Insights
Mar 7, 2023 VIENNA
MRI can be a powerful tool for diagnosing problems in newborns, but transferring infants to the radiology department for scanning creates a number of issues. Aspect Imaging has developed Embrace, a 1-telsa MRI scanner that can be installed in the neonatal intensive care unit (NICU) to enable MRI to be used at the bedside. Aspect Imaging demonstrated the Embrace scanner at the 2023 European Congress of Radiology (ECR) meeting.



Innovation and Comfort in the NICU: Enhancing the Neonatal Experience:
In the fast-paced world of neonatal care, where infants face immense challenges from their earliest moments, a wave of innovation is transforming the NICU into a place of both healing and joy. Amidst the beeping monitors and hushed whispers, new technologies and thoughtful touches are bringing smiles to the faces of families and healthcare professionals alike.
Imagine, for a moment, the introduction of point-of-care MRI machines, compact enough to fit beside a newborn’s crib yet powerful enough to provide detailed images without the need for transport. Picture tiny headphones delicately placed on the ears of our smallest patients, playing gentle melodies to soothe and comfort them during procedures. In these small yet significant advancements, the NICU transcends its clinical setting, becoming a sanctuary of warmth and reassurance.
But the innovation doesn’t end there. Enter virtual reality (VR), once reserved for gaming enthusiasts, now offering parents a momentary escape to tranquil beaches or serene forests, providing a much-needed respite from the sterile surroundings. Meanwhile, specialized mobile apps empower parents to track their baby’s progress, celebrate milestones, and inject a touch of whimsy into their daily routines with photo filters that adorn their infants with superhero capes or astronaut helmets.
This harmonious blend of technology and compassionate care paints a future where laughter and joy are as integral to the NICU experience as medical treatment. It’s a future where parents find solace and moments of levity amidst the uncertainty, and where our smallest patients are given every opportunity not just to survive, but to thrive.
As we embrace these innovations, we usher in a new era of neonatal care—one filled with hope, imagination, and the promise of brighter beginnings for our tiniest heroes and their families.

Mom inspired to become a nurse after son’s diagnosis with heart defects

By Yi-Jin Yu – February 19, 2024
An Indiana mother was inspired to change careers after her second child was diagnosed with congenital heart defects and spent nearly two months in a neonatal intensive care unit.
With February being Heart Month, Calley Burnett is sharing her personal story to raise awareness about congenital heart defects, something she had no idea her son Spencer would have when he was born on July 26, 2016.
Burnett, who previously worked for a family business, is now a NICU nurse at Riley Hospital for Children in Indianapolis, the same hospital where Spencer was sent for further care days after his birth.
Calley Burnett was inspired to become a nurse after her second son, Spencer, was born with congenital heart defects.
Burnett’s positive experience with the Riley nurses and doctors who cared for Spencer left an indelible mark on her and in 2019, the mom of two decided to go back to nursing school and become a registered nurse.
“Spencer was born with congenital heart defects and that led my way into the nursing program after just being bedside for several weeks with Spencer at Riley,” the 39-year-old told “Good Morning America.”
Recent Stories from GMA
Burnett said even though it was a “very scary” time for her while Spencer was in the NICU, she and her family had a team of caring health providers who were dedicated to helping Spencer through his many treatments and hurdles.
Spencer had to spend nearly two months in the neonatal intensive care unit at Riley Hospital for Children in Indiananpolis, Indiana.
Spencer had to be treated for multiple heart defects, including coarctation of the aorta, ventricular septal defect, and patent ductus arteriosus. This meant a part of Spencer’s aorta was narrower than usual, he had an unclosed hole in his aorta and he also had a hole in the wall separating the two ventricles of his heart.
According to Burnett, Spencer needed to have a closed-heart surgery in August 2016 before he was discharged. Nearly a year later, the boy also had an open-heart surgery in July 2017, all to treat the various heart issues he was born with.
“We had just phenomenal nurses there that I still talk to today … Their bedside manner and how they made me feel and the trust that I had and the bond that we had, it just opened my eyes to say, ‘You know what, I think that this is something that I would love to do,'” Burnett explained.
It took Burnett, who had to take prerequisite classes, about two years to complete nursing school. The working mom said although it was “tough,” the sacrifices and the hard work were “very well worth it.”
After graduating, Burnett first took a job at another hospital but she knew she wanted to return to Riley, where the staff meant so much to her and Spencer.
“I knew immediately that I wanted to be with the babies. There’s just something about being at Riley and being with kids and tiny little infants that I just knew that’s where my heart was going to be as soon as I hit nursing school,” Burnett said.
Today, Spencer is an active second grader who plays basketball and soccer.
“He is a very spunky 7-year-old. He’s very athletic. He’s always on the go, always making me laugh. He is just loving life,” his mother told “GMA.”
Burnett says she’s staying on her toes as a NICU nurse at Riley, which she said “feels like home.”
“It’s a phenomenal feeling to be able to help the parents because I feel like I’ve been there. I can tell these moms and dads, ‘Hey, I’ve been where you are and I understand.’ And I just love it,” she said.
For others inspired to take a turn in their own careers or to go into nursing themselves, Burnett said she encourages them to take the leap.
“If that is your passion. I would 100% follow [it]. It’s worth it,” she said. ‘The journey is worth it. It’s tough. But what you get back from it is a hundred times better.”


Mama Sing My Song 715 views Jan 19, 2024
“My Little Fighter – NICU Baby Song” by @mamasingmysong AS SEEN ON SHARK TANK! https://www.mamasingmysong.com

🦸♂️💜Children’s Book Read Aloud: SUPREEMIE: KYLO’S JOURNEY THROUGH THE NICU by Nico Avery + Shanel

On this episode of Nighty Nights with Miss Neli, we join our friend Kylo on his journey to grow big and strong so that he can go home with his family from the NICU. Book Description: This book takes readers on a journey with a micro premature baby named Kylo. Born weighing just 1 pound 3 ounces, Kylo may be small but that doesn’t stop him from being super. He’ll have to stay in the NICU (Neonatal Intensive Care Unit), which is way different from mommy’s belly until he’s big and strong enough to go home. But adventure and growth await him during his hospital stay. This story follows Kylo on his journey to grow stronger and bigger. SUPREEMIE KYLO’S JOURNEY THROUGH THE NICU


Forgotten Island – Paragliding on the island of Socotra (in English)

NOVA | Performance Paragliders Oct 28, 2014 #FLYnova #parapente #paragliding
A group of professional test pilots explore the remote and rarely visited Island of Socotra off the coast of Yemen in the heart of the Middle East. Join them as they thermal up to 1000m over the Indian Ocean, battle 40 km/h winds, and fly from the longest caves in the orient. A 37 minute documentary including spectacular aerial footage from one of the few remaining flying secrets left on earth. #NOVAparagliders #NOVAwings #FLYnova #Gleitschirm #paragliding #parapente #parapendio #paragleiter #ForgottenIsland





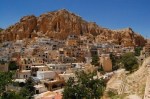







 Published on Jan 31, 2019 Physician Mental Health & Suicide
Published on Jan 31, 2019 Physician Mental Health & Suicide