Honduras, officially the Republic of Honduras, is a country in Central America. It is bordered to the west by Guatemala, to the southwest by El Salvador, to the southeast by Nicaragua, to the south by the Pacific Ocean at the Gulf of Fonseca, and to the north by the Gulf of Honduras, a large inlet of the Caribbean Sea. Its capital and largest city is Tegucigalpa.
The nation’s economy is primarily agricultural, making it especially vulnerable to natural disasters such as Hurricane Mitch in 1998. The lower class is primarily agriculturally based while wealth is concentrated in the country’s urban centers. Honduras has a Human Development Index of 0.625, classifying it as a nation with medium development. When adjusted for income inequality, its Inequality-adjusted Human Development Index is 0.443.
The health system consists of a public and a private sector. The former includes the Ministry of Health and the Honduras Social Security Institute . The Ministry serves the entire population in its own facilities staffed by its own physicians and nurses, but it is estimated that only 50%-60% of Hondurans regularly use these services. The Institute covers 40% of employed economically active individuals and their dependents, using its own and contracted facilities. The private sector serves some 10%-15% of the population: those who can afford to pay or are covered by private insurance. An estimated 17% of Hondurans do not have regular access to health services.
Source:https://en.wikipedia.org/wiki/Honduras
- GLOBAL PRETERM BIRTH RATES – HONDURAS
- Estimated # of preterm births: 12.5 per 100 live births/Global Average: 10.6
- Source- WHO Preterm Birth Rate (Per 100 Live Births)
- World Population Review

COMMUNITY

Health Care Needs and Costs for Children Exposed to Prenatal Substance Use to Adulthood
Evelyn Lee, PhD1,2; Deborah Schofield, PhD2; Mithilesh Dronavalli, MPhil3; Kate Lawler, BSc(Med)Hons4; Hannah Uebel, MD4,5; Lucinda Burns, PhD7; Barbara Bajuk, MPH8; Andrew Page, PhD3; Yuanyuan Gu, PhD6; John Eastwood, MBChB, PhD9,10,11,12,13,14; Michelle Dickson, PhD15; Charles Green, PhD16; Lauren Dicair, MSW17; Ju Lee Oei, MD4,18,19
JAMA Pediatr. Published online July 22, 2024. doi:10.1001/jamapediatrics.2024.2281
Key Points
Question Does the increase in health care needs among children exposed to substance use during pregnancy vary by engagement in out-of-home care?
Findings In this cohort study, children exposed to substance use during pregnancy with or without neonatal abstinence syndrome were at higher risk of adverse birth outcomes and long-term costs than children who were not exposed but a reduction in cost was associated with any out-of-home care contact.
Meaning Increased support and timely access to services could mitigate the higher readmission risk and cost associated with substance use during pregnancy.
Abstract
Importance
Children exposed to substance use during pregnancy have increased health needs but whether these are influenced by engagement in out-of-home care is uncertain.
Objective
To evaluate the association between substance use during pregnancy, out-of-home care and hospitalization utilization, and costs from birth up to age 20 years.
Design, Setting, and Participants
This was a retrospective cohort study using individual-linked population birth, hospital, and out-of-home care information of all liveborn infants from New South Wales, Australia, between 2001 and 2020 using longitudinal population-based linkage records from administrative databases. Substance use during pregnancy included newborns with neonatal abstinence syndrome (n = 5946) and intrauterine exposure to drugs of addiction (n = 1260) and other substances (eg, tobacco, alcohol, and illicit drugs or misused prescription drugs; n = 202 098). Children not exposed to substance use during pregnancy were those without known exposure to substance use during pregnancy (n = 1 611 351). Data were analyzed from July 2001 to December 2021.
Main Outcomes
Main outcomes were hospital readmission, length of stay, and cost burden associated with substance use during pregnancy from birth up to age 20 years. Outcomes were investigated using 2-part and Poisson regression models adjusted for sociodemographic characteristics. Mediation analysis was used to evaluate whether the association of substance use during pregnancy with risk of readmission was mediated through engagement with out-of-home care.
Results
Of the 1 820 655 live births, 935 807 (51.4%) were male. The mean (SD) age of mothers was 30.8 (5.5) years. Compared with children who were not exposed to substance use during pregnancy, those who were exposed incurred significantly higher birth hospital costs (adjusted mean difference, A$1585 per child [US$1 = A$1.51]; 95% CI, 1585-1586). If discharged alive, more children with exposure to substance use during pregnancy had at least 1 readmission (90 433/209 304 [43.4%] vs 616 425/1 611 351[38.3%]; adjusted relative risk [RR], 1.06; 95% CI, 1.06-1.07), most commonly for respiratory conditions (RR, 1.11; 95% CI, 1.09-1.12) and mental health/behavioral disorders (RR, 1.36; 95% CI, 1.33-1.41). Excess hospital costs associated with substance use during pregnancy were A$129.0 million in 2019 to 2020. Mediation analyses showed that any out-of-home care contact mediated the association between substance use during pregnancy and risk of inpatient readmission and lower health care cost (decreased by A$25.4 million). For children with neonatal abstinence syndrome, any out-of-home care contact mediated readmission risk by approximately 30%, from adjusted RR, 1.28; 95% CI, 1.19-1.35, to RR, 1.01; 95% CI, 0.98-1.02.
Conclusion and Relevance
Children who were exposed to substance use during pregnancy incurred more hospital costs than children who were not exposed up to 20 years of age, but this was reduced in association with any contact with out-of-home care. This provides insights into possible strategies for reducing health and financial burdens associated with exposure to substance use during pregnancy for children.
Source:https://jamanetwork.com/journals/jamapediatrics/fullarticle/2821473

Talento Catracho Key Key (Caramelo)


Enhancing NICU Care and Communication: Perspectives of Moderately Preterm Infant Parents
Ashley D. Osborne, MD; Diana Worsley, MPH; Catherine Cullen, MD; Ashley Martin, MPH; Lori Christ, MD
May 08 2024
BACKGROUND
Moderately preterm infants (MPTI) comprise a large proportion of NICU admissions and are an understudied population. The unique experience of families with MPTIs has yet to be examined in the literature. Describing MPTI parent needs and preferences may inform interventions to improve care and outcomes for this population.
METHODS
Semi-structured qualitative interviews were performed with English-speaking birth parents of infants born between 32 and 34 weeks gestation to describe their NICU experience and identify areas for improvement specifically surrounding care team inclusion, education, discharge, and communication. Interviews were recorded, transcribed, and analyzed using directed content analysis. Enrollment ceased when the data reached thematic saturation.
RESULTS
Sixteen birth parents participated. Four themes emerged around parent-medical team connectedness, parental confusion, discharge readiness, and the desire for a use of a mix of in-person and electronic communication methods (e-mail, texting, apps, etc.) for communication. MPTI parents valued a strong connection with the medical team; however, they described a lack of knowledge regarding the reasons for admission and ongoing management. Near discharge, parents desired more information regarding feeding, reflux, and breathing patterns. Parents preferred in-person discussions but described a role for electronic methods to improve their understanding of their infant and discharge readiness.
CONCLUSIONS
From the MPTI parent perspective, clinicians can focus improvement efforts on communication, specifically around reasons for admission, discharge planning, and anticipatory guidance. These results may serve as a foundation for initiatives to improve the MPTI parent experience and potentially parent and MPTI outcomes.

He was born dead” Derick Hall’s Miracle Journey to the NFL
Apr 28, 2023 #NFL #AmericanFootball #Football
Auburn’s Derick Hall survives the near-death experience of being born four months premature, rising to become one of the best defensive ends in the nation – and making a transformational impact on his Gulf Coast community.


HEALTHCARE PARTNERS

The Relationship between Pediatric Medical Training and Neonatal Care in the Delivery Room and Beyond
Nicolle Fernández Dyess, MD, MEd; Perspectives| September 01 2024
Shetal Shah, MD Neoreviews (2024) 25 (9): e531–e536.https://doi.org/10.1542/neo.25-9-e531
The modern neonate differs greatly from newborns cared for a half-century ago, when the neonatal-perinatal medicine certification examination was first offered by the American Board of Pediatrics. Delivery room resuscitation and neonatal care are constantly evolving, as is the neonatal workforce. Similarly, the Accreditation Council for Graduate Medical Education review committees revise the requirements for graduate medical education programs every 10 years, and the modern pediatric medical trainee is also constantly evolving. Delivery room resuscitation, neonatal care, and pediatric residency training are codependent; changes in one affect the other and subsequently influence neonatal outcomes. In this educational perspective, we explore this relationship and outline strategies to mitigate the impact of decreased residency training in neonatal-perinatal medicine.
Full Article


Peer Nurse to Nurse Mentoring – An Exceptional Act of Kindness
Dudding, Katherine M. PhD, RN, RNC-NIC, CNE; Assistant Professor
Advances in Neonatal Care 24(5):p 389-390, October 2024.

A couple of months ago, I had a conversation with a Director of Nursing Professional Development from a potential hospital site which to conduct my research. I was asked if I would consider having a couple of nurses help with my study. Without hesitation, I replied “yes, I would be happy to mentor a couple of nurses to assist me with my study.” Initially, I thought this was an odd request because I feel like that is one of my professional responsibilities as a nurse. Upon further thinking, I realized maybe others do not share the same opinion and how unfortunate this would be for our future neonatal nurses, practitioners, educators, and researchers.
According to the American Nurses Association (ANA), 18% of nurses are leaving the profession after 1 year though other sources reported even higher rates of attrition. The nursing workforce dilemma continues to be problematic with nurse turnovers and an alarming rate of nurses leaving the profession after 1 year. While other sourcesreported rates as high as 30%, education and the healthcare systems are establishing strategic interventions to retain nurses. One of these interventions is mentoring. Specifically, peer nurse to nurse mentoring is beneficial when matched into a positive mentored relationship.
MENTORING
Nurses experiencing positive mentorships are associated with intent to remain at their current positions. There is nothing like the support of a mentor when you begin your nursing career. It was the kindness of mentors that taught us and encouraged us to become the best possible nurses and achieve our dreams. The knowledge we gained from our mentors are incorporated into our everyday professional lives. There is not one of us who was not impacted by a mentor and their influence (see Supplemental Figure 1, available at https://links.lww.com/ANC/A292). Many of us will have several distinct types of mentors throughout our nursing careers.
Each mentor serves a purpose and may be time limited. There may be mentors that are experts in clinical practice, education, research, or leadership. You might even have a mentor, whose sole purpose, is your sounding board for difficult decisions. However, there will be a handful of phenomenal nurses who will become lifetime mentors. Those are the special ones that we strive to emulate.
NURSING
When nurses feel supported by administration and mentors, they remain in their jobs. Being mentored gives us the opportunity to grow our skill sets or learn new processes under the guidance of our mentor. The mentor provides the safety net when learning and a resource to ask our never-ending questions without judgment.
We all can remember the hesitation we felt the first time we attempted our first IV. Moreover, we remember the happiness we felt when we successfully started our first IV. This was, in part, due to our mentor’s willingness to mentor us and invest their time and talent into our success. Our mentors believed in us.
It does not take long before these skills in essence become second nature. Our confidence level begins to increase with more successes than failures. We are becoming competent and independent nurses. These achievements cannot help but to spill over into our own interactions with patients, our students with teaching, and our participants in research. Good mentorship also benefits those we serve whether it be our patients, our students we teach or participants in research. Why would we not pay this forward when mentoring results in the best possible outcomes for all?
As our skills are honed, this cultivates our confidence, not only as a competent nurse, but as a valuable team member. Lyu et al states that competence and being integrated into a team is correlated with retention. As a supported team member, we are unstoppable to what we can accomplish in nursing. Eventually, this often leads the nurse mentee to now becoming the mentor.
GROWING THROUGH MENTORSHIP
Being a mentor is frequently the catalyst for endless opportunities for growth and the development of a leader. This may be a leadership opportunity within your respective work environment such as a charge nurse, manager, and director. Your sphere of influence, as a leader, has the ability change practice within the nursing. Moreover, this may motivate a broader impact by earning an advanced degree to become nurse practitioners, educators, and researchers.
What a privilege it is to mentor nurses and leave a lasting impact on the nursing profession. Today’s nursing graduates are tomorrow’s nursing leaders. We have a responsibility to present and future nurses to mentor them. I, personally, will forever be grateful to all my mentors. I am truly standing on the shoulders of giants by kindness that has and continues to be given to me. This act of kindness and giving of oneself through mentoring is invaluable.
In conclusion, there is only one question that remains, “will you step up to mentor the next generation of nurses?”
—Katherine M. Dudding, PhD, RN, RNC-NIC, CNE Assistant Professor The University of Alabama kmdudding@ua.edu

Why medical residency should be reformed: It ‘can unmoor even the best of us’

July 19, 2023 Sathvik Namburar
In a May 6, 2016 photo, medical residents Dr. Wes Penn, right, and Dr. Cameron Collier, center, walk with medical students down a hallway during their daily rounding at Our Lady of the Lake Regional Medical Center in Baton Rouge, Louisiana. (Gerald Herbert/AP)This article is more than 1 year old.
July marks a time of change in hospitals across the country. It marks the beginning of the academic year for medical residents and fellows, with new physicians starting their training. As I begin the second year of my medical residency this month, I have been thinking about Libby Zion and Nakita Mortimer.
The former was briefly a household name in the 1980s. Libby Zion was a college student who sought care at New York Hospital (now New York-Presbyterian) with a fever in March 1984, only to pass away after her doctors missed a crucial medication interaction. Her distraught parents believed that overworked resident physicians were to blame and drove efforts to institute work-hour caps for residents.
The latter is tragically less known. Dr. Nakita Mortimer was a resident physician at Montefiore Medical Center, and she died by suicide in May 2023. My colleagues and I became aware of her untimely passing almost immediately, as this news spread rapidly through the medical world. (As with all suicides, it will remain unclear specifically why Dr. Mortimer took her own life.)
My colleagues and I reacted to Dr. Mortimer’s death with shock but not surprise. As one of the senior resident physicians in my program put it, “Residency can unmoor even the best of us.”
All of us in the medical profession know classmates or colleagues who were unable to complete their training, overburdened by the demands of the profession. Studies show that upwards of 50% of physicians report feeling burnout.
Residency is a key contributor to these issues. Usually lasting between three and seven years depending on subspecialty, resident physicians have completed medical school but are still undergoing training and cannot independently practice medicine.
Being a resident means working long hours for little pay (the average first-year resident makes about $60,000 a year). Many residency programs continue to require residents to work 28-hour shifts out of a belief that these long hours enhance continuity of care and resident learning.
But by the end of 28-hour shifts, residents are so sleep-deprived that they have the equivalent of blood alcohol contents of 0.1%, above the threshold for being legally drunk. The resident physicians who were taking care of Libby Zion were in the midst of a 28-hour-plus shift and were also responsible for 40 other patients on the night she died.
Often forgotten in the Libby Zion case is that her death led her parents to push not only for reforms in the medical residency system, but also the consideration of legal charges against the resident physicians and the threat of revocation of their licenses to practice medicine. Therefore, to my co-residents and me, her passing is both a clarion call and a warning, that even if we are tired, we must be perfect or else lose our livelihoods. Of course, with the desire for perfection comes incredible mental stress.
With the desire for perfection comes incredible mental stress.
We resident physicians recognize that our profession has societal responsibilities. It is our duty to learn and take care of patients, and we do not and should not expect to work regular 9 a.m. to 5 p.m. hours during our training. My goal is to maximize my learning opportunities so that when I complete residency, I can practice medicine independently and competently.
Physicians take an oath to “Do no harm” and try to live up to this credo. But no one can always be perfect.
Some residency programs have been implementing further reforms to protect resident physicians and patients. Over the past year, I have only had to complete one 28-hour shift, compared to my friends in other residency programs who have had to do dozens of such shifts. My residency also has a dedicated wellness curriculum, peer listening programs and access to mental health professionals.
Still, there is more to do. Residents in programs around the country are forming unions and demanding better working conditions and more pay. After 26 years of stagnation, in 2022, Congress finally approved an increase in the number of residency spots, which would decrease the work burden on residents. Our patients should support these efforts and push for further changes because well-rested, better-paid residents are more likely to provide adequate health care.
Few other jobs place physical and mental demands on employees like residency does, and few other jobs come with the awesome responsibility that being a physician has. Continuing reforms will help prevent deaths like those of Libby Zion and Dr. Mortimer. We owe it to all resident physicians and our patients to ensure that such reforms are enacted.
Editor’s note: You can reach the National Suicide Prevention Lifeline at 1-800-273-TALK (8255) and the Samaritans Statewide Hotline (call or text) at 1-877-870-HOPE (4673). Call2Talk can be accessed by calling Massachusetts 211 or 508-532-2255 (or text c2t to 741741).

PREEMIE FAMILY PARTNERS

Empowering NICU Parents: How to Advocate for Your Preemie

A Million Little Miracles Premiered May 22, 2024
Feeling lost on how to advocate for your preemie in the hospital? NICU grad mom Alexis shares practical tips to help you become your baby’s champion!


‘Once a preemie, always a preemie:’ Mother reflects on her son’s remarkable journey from the NICU–Patient Stories

When Shalece Kimble watches her 4-year-old son, Shea, barrel through the house at top speed or navigate his bike outside, she can hardly believe he is the same child who was just a fragile 2 lbs., 3 oz. when he was born prematurely on March 28, 2016.
Shalece was 30 weeks pregnant when she went to UPMC Magee-Womens Hospital for a follow-up sonogram. At a routine prenatal appointment the week before, doctors felt the baby was smaller than he should be, so they asked her to come back for a second look.
She told her husband, Dion, not to bother calling off work; convinced that there was no danger, she brought her aunt instead, and the two women made plans to go for lunch after the appointment.
“When I got down there, they did the first sonogram. I could tell by their reaction that something was wrong, but they didn’t want to alarm me,” she recalled. “They said, ‘We’re going to send you upstairs for a uterine sonogram and a monitor.’”
Her older son, Dion 2nd, was born at full term 11 years earlier with no complications. So while her aunt panicked, Shalece — a former nursing assistant — remained calm: “I’m not a person who panics a whole lot,” she said, adding that throughout the process, she was thinking, “It’s only 30 weeks. I’m not having this baby today.”
And then the doctor on duty came in and said that, in fact, she was. The blood in the umbilical cord was flowing backward, preventing the baby from getting vital nutrients. She would have to undergo an emergency Cesarian section.
According to Dr. Yoel Sadovsky, MD, executive director of Magee-Womens Research Institute, the reversal of blood flow in the umbilical cord is usually caused by a dysfunction in the placenta — a complication Dr. Sadovsky and other researchers at the institute study.
In such cases, delivery is induced in an effort to save the baby’s life, he noted: “If you don’t deliver someone who has these kinds of findings, some babies don’t even make it.”
But at that moment, Shalece was in denial, even though the staff advised her to call her husband and get him to the hospital.
“I was absolutely not going for it,” she recalled. “In my mind, it wasn’t happening to me; it was happening around me.”
Finally, her aunt called her husband, who arrived in time for the emergency delivery. Their son was born at 1:33 p.m., but Shalece’s blood pressure skyrocketed, so she only glimpsed him before he went to the neonatal intensive care unit (NICU).
Once she stabilized, the staff wheeled her, still in her hospital bed, to meet her tiny son.
“There were more cords and plugs than baby,” she said. “I was able to see him, really see him. From there, it was me and him.”
Little Shea spent two months and three days in the NICU. After seeing her older son on the school bus in the morning, Shalece traveled back to the hospital, where she would sing to Shea, read to him from the Game of Thrones series, and talk.
“I told him, ‘You’re a squatter in this NICU. You’re coming home,’” she said. “I willed this baby into coming home.”
Of the 380,000 babies born prematurely in the United States each year, rates are up to 50 percent higher among women of color, according to the March of Dimes. Black children face an infant mortality rate that is more than twice as high as other infants, according to the U.S. Centers for Disease Control, making prematurity the largest contributor to infant mortality disparities.
Shea spent the first few hours of his life on oxygen and was treated with bilirubin lights for jaundice. He went through several blood transfusions and experienced a brain bleed, but no surgery was required. He also had retinopathy of prematurity, an eye disorder caused by abnormal blood vessel growth in the retina of premature infants, and wears glasses now. He also undergoes physical therapy for mild cerebral palsy.
About a quarter to a third of preterm births are medically induced, Dr. Sadovsky said. Less than 5 percent of all babies need to have a medically-induced preterm delivery for growth restriction, and in the majority of these cases, the placenta is the cause.
“This is a typical case of what we’re studying in our lab,” Dr. Sadovsky said. “One of the major goals of our research is better diagnosis, and importantly, prevention of these kinds of stories.”
Despite the long odds, Shea is now in preschool, and most people don’t realize he has had difficulty walking or climbing steps in the past. He adores sports and superheroes, and he looks up to his big brother.
“He’s your average 4-year-old boy. He is loud. He is fast,” said Shalece.
She knows his premature birth will always influence other parts of his life; she’ll have to be careful about his participation in sports because of his early brain bleeds, and she pays attention to how he learns things, or even how he holds a pencil.
“Once a preemie, always a preemie. You are always on high alert,” she said. She belongs to a support group for mothers of premature infants, where she both draws and offers encouragement.
Asked what advice she would offer to a new mother of a preemie, Shalece said: “Take it one day at a time. Don’t hesitate to cry; crying is good. Don’t feel bad, and reach out for help.”
She remembers how worried she was, and looks at her 4-year-old son riding a bike and realizes how far he has come.
“You have to try a little harder as a parent,” she said, but added, “Being born premature doesn’t mean they aren’t going to be the kid you thought they were going to be.”

Supporting Your Premature Baby’s Development: Essential Tips and Activities

Jul 9, 2024 #swaddling #babytips #preemiebaby
Was your baby born more than 3 weeks early? Premature development differs from full-term, but there’s no need to worry! Let’s explore effective ways to understand and support your baby’s growth and milestones. Premature babies are often born with more extended (straight) positions, while full-term babies get a curled up (flexed) feeling from being in the womb longer. Babies need both flexion and extension to help their motor skill development. Try these activities to aid your preemie’s physical growth and work on their flexion. Always consult your healthcare provider for personalized advice.


Your Preemie’s Growth and Development: 2 and Up

Medically Reviewed by Amita Shroff, MD on July 30, 2023 Written by R. Morgan Griffin
By the time they’re 2, your preemie has come a long way. It may be hard to believe that your child — maybe a noisy, strong-willed toddler already — is the same person as that tiny, fragile baby you anxiously watched over in the hospital.
What comes next? As they grow, most preemies become healthy children. But some continue to have health issues. And even kids that do well generally may have lasting health effects years and even decades later.
There’s no way to know exactly how your child will grow and develop. In general, the earlier your child was born, the more likely they are to have lasting health issues. Watch out for signs of problems so you can get your child the care and treatment they need.
Your Preemie’s Long-Term Health
If your child was born prematurely, they have a higher chance of some of these health concerns:
Growth problem: Kids who were born at less than 32 weeks of pregnancy — what doctors call “very premature” — are likely to be shorter and weigh less than other kids.
Learning disabilities.Some preemies have lasting problems with how they think and learn. About 1 in 3 kids born prematurely need special school services at some point.
Behavior problems: As they grow up, preemies may be more likely to have attention deficit hyperactivity disorder (ADHD) than full-term babies. They’re also more likely to be shy or anxious.
Breathing problems and asthma:.Lots of preemies need help breathing when they’re born, since their lungs aren’t ready yet. While these issues often go away, some babies born prematurely have lasting asthma or similar problems.
Other health conditions:Some preemies have more serious long-term complications. One example is cerebral palsy, which causes problems with movement and balance. There’s no cure, but it can be managed with treatment. Other kids may have lasting problems with their vision, hearing, and digestive system.
Remember, your child may not develop any of these problems or may outgrow them. But being aware that they have a higher chance of having them is important. If you notice signs, you can get help from your child’s doctor. The faster your child gets treatment for any problems, the better.
Your Preemie in Early Childhood
While your child might have been treated for lots of health problems in the hospital when they were born — like apnea, reflux, and jaundice — most if not all of those should be gone by now. Experts say that in terms of growth, most preemies are more or less caught up to full-term babies by age 3.
When your child is still young you can:
Keep track of your baby’s developmental milestones. Milestones are skills your child will learn, like riding a tricycle or walking up the stairs on their own. They’re often linked with the average age kids are able to do them. When preemies are young, doctors use their “corrected age” — based on their original due date — instead of their birthdate when checking milestones. But by age 2, most preemies have caught up enough that you can start using their actual age.
Remember that milestones are just rough averages. All kids develop differently, whether they’re full-term or premature. It’s not a big deal if your child doesn’t meet a milestone exactly on schedule.
Get help if you need it. If you do notice your child seems to be lagging behind, talk to their doctor. Make sure to ask about a state program called Early Intervention. It offers special services to help babies up to age 3 who have higher odds of developmental delays or disabilities. Some of these services are free. Other options include referral to private therapies such as physical therapy, occupational therapy, feeding therapy, and speech therapy.
Getting Your Child Ready for School
Watching your child go off to school is exciting — and stressful, too. To help make the transition smoother and give your child support, you can:
Get in touch with the school early. Before your child starts school, talk to the staff — like their teacher or the principal — about their health issues and concerns you have. Ask questions about the school’s special education programs. If your child’s teachers understand their needs, they’ll be better able to help them succeed.
Be alert for any new problems. Sometimes, learning disabilities or behavior problems only show up once a child starts school. If your child seems to be struggling, work with their teacher — and make sure your youngster gets special services if they need them.
Gradually give your child more independence. After you spend so much time caring for your child, it can be hard to let them go off on their own. But you have to find a balance between protecting them when they need it and giving them the freedom they need to grow.
As Your Preemie Grows Up
Will the effects of being born premature last into your child’s adulthood? It’s possible. Some studies have linked being a preemie with a higher chance of getting conditions like diabetes, high blood pressure, and lung and vision problems in adults.
But again, remember that your child only has a higher risk of these problems. They may not develop any of them. You can look at being born premature as another factor that may raise your risk of developing health issues, like a person’s genes, habits, home life and environment. After all, plenty of adults who weren’t born prematurely develop the same health conditions.
The most important need for a child who was born prematurely is to get good, consistent care — both as a child and an adult. Being a preemie can create barriers to your child’s development. But with the help of the right experts — doctors, specialists, therapists, and others — you can often find ways to work around them.
Source: https://www.webmd.com/children/preemies-growth-development-age-two-up

INNOVATIONS

Transforming Healthcare 2024: Changing the Practice of Medicine with Artificial Intelligence (AI)

University of Colorado Anschutz Medical Campus Apr 9, 2024
While a recent explosion in AI technology has exposed its possibilities to the public with online systems such as ChatGPT and Dall·E, researchers at the University of Colorado Anschutz Medical Campus have been exploring the rapidly evolving technology for years and are beginning to harness its problem-solving powers to change healthcare.
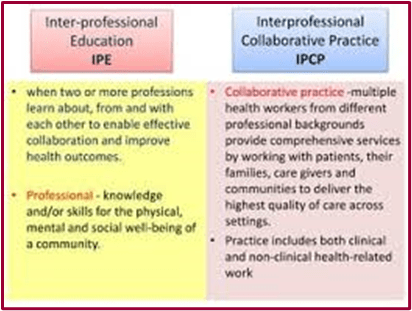
Defining IPE & IPCP

Interprofessional Education (IPE) is more than sitting passively in a classroom together. It is integrative, experiential, and about learning and practicing the skills needed to function effectively as a highly collaborative team. Interprofessional collaborative practice makes care safer, more patient-centered, and it leads to lower burnout and higher job satisfaction amongst health professionals. Explore below to learn more about the opportunities to grow your skills in collaboration.
Interprofessional Education (IPE) is an approach to teaching and learning that brings together students from two or more professions to learn about, from, and with each other in service of enabling effective collaboration. The goal of IPE is to improve health outcomes through the education of a practice-ready health care team that is prepared to respond to local health needs (WHO, 2010).
Interprofessional Collaborative Practice (IPCP), or “Practice Transformation,” in health care occurs when multiple health workers from different professional backgrounds provide comprehensive services by working with patients, their families, carers and communities to deliver the highest quality of care across setting (WHO, 2010). The Interprofessional Education Collaborative (IPEC) states that, “interprofessional collaborative practice drives safe, high-quality, accessible, person-centered care and improved health outcomes” (2019).
Source:https://collaborate.uw.edu/about-us/defining-ipe-and-ipcp/

Preterm birth and educational disadvantage: Heterogeneous effects
Anna Baranowska-Rataj, Kieron Barclay, Joan Costa-Font,Mikko Myrskylä, Berkay Özcan
Population Studies/ Research Article
A Journal of Demography – Volume 77, 2023 – Issue 3
Abstract
Although preterm birth is the leading cause of perinatal morbidity and mortality in advanced economies, evidence about the consequences of prematurity in later life is limited. Using Swedish registers for cohorts born 1982–94 (N = 1,087,750), we examine the effects of preterm birth on school grades at age 16 using sibling fixed effects models. We further examine how school grades are affected by degree of prematurity and the compensating roles of family socio-economic resources and characteristics of school districts. Our results show that the negative effects of preterm birth are observed mostly among children born extremely preterm (<28 weeks); children born moderately preterm (32–<37 weeks) suffer no ill effects. We do not find any evidence for a moderating effect of parental socio-economic resources. Children born extremely preterm and in the top decile of school districts achieve as good grades as children born at full term in an average school district.
Full Article

Supplementary material for this article is available at: http://dx.doi.org/10.1080/00324728.2022.2080247.


The Transformative Power of Sports: A Journey from Micro-Preemie to Empowered Adult
As a micro-preemie, my early days were filled with challenges, but the encouragement from my mother to engage in sports became a pivotal part of my development. Growing up, I was introduced to various physical activities, from swimming to basketball, which not only helped me build strength but also instilled a sense of confidence that was essential for my growth. Research has shown that early engagement in sports can significantly benefit the physical and emotional development of children, particularly those with a history of premature birth. According to a study published in the Journal of Pediatrics, participation in physical activities helps improve motor skills and overall health, which are critical areas of development for preemies.
The benefits of sports extend beyond physical health; they also foster social skills and emotional resilience. Engaging in team sports allowed me to develop friendships and learn the value of teamwork. These experiences helped me navigate social dynamics and build a support network that would prove invaluable throughout my life. A report by the American Academy of Pediatrics emphasizes that participation in sports can promote social interactions and enhance communication skills, which are crucial for preemie survivors as they transition into adulthood. My mother’s encouragement to embrace sports created opportunities for me to thrive socially, fostering connections with peers who understood my unique journey.
Moreover, sports provided an essential outlet for stress relief and emotional expression. As I faced the lingering effects of my premature birth, participating in physical activities became a healthy way to cope with anxiety and build self-esteem. Studies have indicated that regular physical activity can reduce symptoms of anxiety and depression, particularly in children who may feel different or face health-related challenges. This therapeutic aspect of sports not only aided in my emotional well-being but also reinforced my belief in the importance of maintaining a healthy lifestyle, which I carry into adulthood.
Reflecting on my journey, I am grateful for my mother’s unwavering support and encouragement to engage in sports. The lessons I learned and the resilience I built through these experiences have shaped who I am today. For other preemie families, I encourage you to explore the world of sports and other physical activities you and they may prefer. The benefits are profound and can lead to a brighter, healthier future for your little ones.
Representation Matters: The Role of Adaptive Sports in the Lives of People with Disabilities
Mid-Atlantic ADA Center 453 views May 30, 2023
Dr. Anjali Forber-Pratt, Director of the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) and two-time Paralympian, talks about the importance of adaptive and inclusive sports and recreation for people with disabilities.
People with disabilities are athletes too | David Kyle | TEDxHuntsville

5,773 views Nov 14, 2017
David Kyle explains in his talk about his journey from discovering his disabilities and being depressed to a life full of challenges, mobility and opportunity for success as an athlete. David is the director of the UAH Ability Sport Network, which is a program that encourages participation among people with physical disabilities in adapted physical activity. In addition, he is a lecturer in the Department of Kinesiology of UAH’s College of Education. David holds a master’s degree in Health and Physical Education and will complete his doctoral degree in Kinesiology in 2019. He is also a Certified Exercise Physiologist and Disability Sport Specialist. David is a member of the USA Triathlon National Paratriathlon Committee, and competed internationally for 10 years with the USA Elite Paratriathlon Team in triathlon, duathlon, and XTERRA off-road events winning multiple world and national titles in each discipline.



Froggy Plays Soccer – Storytime With Miss Rosie
Miss Rosie’s Storytime Jun 15, 2019
Froggy Plays Soccer By: Jonathan London & Frank Remkiewicz It’s the day of the big game, and Froggy is ready. His soccer team is playing the Wild Things for the City Cup. All Froggy has to do is remember the rule: “Head it! Boot it! Knee it! Shoot it! BUT DON’T USE YOUR HANDS!” But Froggy’s busy doing cartwheels and picking daisies. Uh oh, Froggy! Here comes the ball! Budding soccer players and Froggy’s many fans will welcome Froggy’s latest hilarious adventure.


Roatan – 96 hour travel and kiteboarding in Honduras

2020 started off as a big kiting year. About a week after I got back from the Grenadines as buddy called saying he’d organized a trip to a little known kite spot in Honduras called Roatan. Everyone scrambled to move things around, and at the last minute it all came together.












 Published on Jan 31, 2019 Physician Mental Health & Suicide
Published on Jan 31, 2019 Physician Mental Health & Suicide