Denmark is a Nordic country in Northern Europe. It is the metropolitan part of and the most populous constituent of the Kingdom of Denmark, a constitutionally unitary state that includes the autonomous territories of the Faroe Islands and Greenland in the North Atlantic Ocean. Metropolitan Denmark is the southernmost of the Scandinavian countries, lying south-west and south (Bornholm and Ertholmene) of Sweden, south of Norway, and north of Germany, with which it shares a short border, Denmark’s only land border.
As of 2013, the Kingdom of Denmark, including the Faroe Islands and Greenland, had a total of 1,419 islands above 100 square metres (1,100 sq ft); 443 of these have been named and 78 are inhabited.] Spanning a total area of 42,943 km (16,580 sq mi), metropolitan Denmark consists of the northern part of the Jutland peninsula and an archipelago of 406 islands.] Of these, the most populated island is Zealand, on which the capital and largest city, Copenhagen, is situated, followed by Funen, the North Jutlandic Island, and Amager. Denmark has flat, arable land, sandy coasts, low elevations, and a temperate climate. It had a population of 5.935 million (1 February 2023), of whom 800,000 live in Copenhagen (2 million in the wider area). Denmark exercises hegemonic influence in the Danish Realm, devolving powers to handle internal affairs. Home rule was established in the Faroe Islands in 1948 and in Greenland in 1979; the latter obtained further autonomy in 2009.
As of 2015, Denmark has a life expectancy of 80.6 years at birth (78.6 for men, 82.5 for women), up from 76.9 years in 2000. This ranks it 27th among 193 nations, behind the other Nordic countries. The National Institute of Public Health of the University of Southern Denmark has calculated 19 major risk factors among Danes that contribute to a lowering of the life expectancy; this includes smoking, alcohol, drug abuse and physical inactivity. Although the obesity rate is lower than in North America and most other European countries, the large number of overweight Danes results in an annual additional consumption in the health care system of DKK 1,625 million. In a 2012 study, Denmark had the highest cancer rate of all countries listed by the World Cancer Research Fund International; researchers suggest the reasons are better reporting, but also lifestyle factors like heavy alcohol consumption, smoking and physical inactivity.
Denmark has a universal health care system, characterised by being publicly financed through taxes and, for most of the services, run directly by the regional authorities. One of the sources of income was a national health care contribution (sundhedsbidrag) (2007–11:8%; ’12:7%; ’13:6%; ’14:5%; ’15:4%; ’16:3%; ’17:2%; ’18:1%; ’19:0%) but it was phased out from January 2019 in favor of income taxes. This means that most health care provision is free at the point of delivery for all residents. Additionally, roughly two in five have complementary private insurance to cover services not fully covered by the state, such as physiotherapy. As of 2012, Denmark spends 11.2% of its GDP on health care; this is up from 9.8% in 2007 (US $3,512 per capita). This places Denmark above the OECD average and above the other Nordic countries.
Source:https://en.wikipedia.org/wiki/Denmark#
GLOBAL PRETERM BIRTH RATES – Denmark
Estimated # of preterm births: 7 % (USA 9.56-Global Average: 10.6)
Source:https://data.un.org/Data.aspx?d=WHO&f=MEASURE_CODE%3AWHS_PBR

COMMUNITY

National Trends in Preterm Infant Mortality in the United States by Race and Socioeconomic Status, 1995-2020
Tim Venkatesan, MA(Cantab), MB, BChir, DTM&H1; Philippa Rees, BSc(Hons), MPhil, MBBCh1; Julian Gardiner, MA, MSc, PhD1,2; et alCheryl Battersby, PhD, BMBS, BMedSci3; Mitana Purkayastha, BDS, MPH, PhD1; Sept.5, 2023

Key Points
Question How have inequalities in US preterm infant mortality changed over time according to a mother’s race and socioeconomic status?
Findings This cross-sectional study including 12 256 303 preterm infant births over 26 years found widening inequality in preterm infant mortality rates between mothers of differing socioeconomic status, while racial and ethnic disparities remained constant over time. Receiving inadequate antenatal care was the biggest predictor of preterm infant mortality across the study period.
Meaning These findings indicate that between 1995 and 2020, US preterm infant mortality improved, but racial, ethnic, and socioeconomic inequalities in preterm infant mortality rate persisted.
Abstract
Importance Inequalities in preterm infant mortality exist between population subgroups within the United States.
Objective To characterize trends in preterm infant mortality by maternal race and socioeconomic status to assess how inequalities in preterm mortality rates have changed over time.
Design, Setting, and Participants This was a retrospective longitudinal descriptive study using the US National Center for Health Statistics birth infant/death data set for 12 256 303 preterm infant births over 26 years, between 1995 and 2020. Data were analyzed from December 2022 to March 2023.
Exposures Maternal characteristics including race, smoking status, educational attainment, antenatal care, and insurance status were used as reported on an infant’s US birth certificate.
Main Outcomes and Measures Preterm infant mortality rate was calculated for each year from 1995 to 2020 for all subgroups, with a trend regression coefficient calculated to describe the rate of change in preterm mortality.
Results The average US preterm infant mortality rate (IMR) decreased from 33.71 (95% CI, 33.71 to 34.04) per 1000 preterm births per year between 1995-1997, to 23.32 (95% CI, 23.05 to 23.58) between 2018-2020. Black non-Hispanic infants were more likely to die following preterm births than White non-Hispanic infants (IMR, 31.09; 95% CI, 30.44 to 31.74, vs 21.81; 95% CI, 21.43 to 22.18, in 2018-2020); however, once born, extremely prematurely Black and Hispanic infants had a narrow survival advantage (IMR rate ratio, 0.87; 95% CI, 0.84 to 0.91, in 2018-2020). The rate of decrease in preterm IMR was higher in Black infants (−0.015) than in White (−0.013) and Hispanic infants (−0.010); however, the relative risk of preterm IMR among Black infants compared with White infants remained the same between 1995-1997 vs 2018-2020 (relative risk, 1.40; 95% CI, 1.38 to 1.44, vs 1.43; 95% CI, 1.39 to 1.46). The rate of decrease in preterm IMR was higher in nonsmokers compared with smokers (−0.015 vs −0.010, respectively), in those with high levels of education compared with those with intermediate or low (−0.016 vs – 0.010 or −0.011, respectively), and in those who had received adequate antenatal care compared with those who did not (−0.014 vs −0.012 for intermediate and −0.013 for inadequate antenatal care). Over time, the relative risk of preterm mortality widened within each of these subgroups.
Conclusions and Relevance This study found that between 1995 and 2020, US preterm infant mortality improved among all categories of prematurity. Inequalities in preterm infant mortality based on maternal race and ethnicity have remained constant while socioeconomic disparities have widened over time.
Source:https://jamanetwork.com/journals/jamapediatrics/article-abstract/2808782?resultClick=24

Lukas Graham – Say Forever (Live from In The Round)

“Say Forever” by Lukas Graham, Live from In The Round Listen to 4 (The Pink Album) now: https://LukasGraham.lnk.to/4ThePinkAlbum


New resources released to help more preterm and low birthweight babies benefit from kangaroo mother care

Mothers and babies should stay together after birth even when the baby is small or sick
16 May 2023
Today, WHO released two new resources to support wider uptake of kangaroo mother care (KMC) – a lifesaving technique which includes ongoing skin-to-skin contact and exclusive breastfeeding – to benefit more small and preterm babies.
Now the leading cause of death of children under 5, prematurity is an urgent public health issue. Every year, an estimated 13.4 million babies are born preterm (before 37 weeks of pregnancy) while an even higher number – over 20 million babies – have a low birthweight (under 2.5 kg at birth). For these babies, KMC is a proven, effective intervention for saving lives and improving their health and development.
“Kangaroo mother care is one of the most critical, lifesaving measures to improve the survival prospects and wellbeing of babies born early or small,” said Dr Anshu Banerjee, Director for Maternal, Newborn, Child and Adolescent Health at WHO. “Ensuring mothers and babies everywhere can stay together and practice kangaroo mother care immediately after birth will require a radical rethink of how maternal and newborn care is organized – these new publications aim to support this process.”
The two publications – a global position paper and implementation strategy – seek to enable the expansion of KMC within health facilities and at home, globally. They follow the release of landmark new guidelines published last year, which recommend KMC as the essential standard of care for all preterm and low birthweight babies, starting right after birth. The new documents highlight that it should be available both for babies that are well and sick – for at least eight hours a day – including in intensive care.
“For most health facilities, achieving the widespread adoption of kangaroo mother care for all preterm or low birthweight babies will require fundamental changes in newborn care provision, especially neonatal intensive care,” said Dr Shuchita Gupta, Medical Officer at WHO who coordinated the development of the new documents. “This includes changes to the physical layout of care facilities, that enable the mother to stay with her small and sick baby inside the newborn care unit on a 24/7 basis. It also means changing the way healthcare is provided so that obstetricians, midwives, paediatricians, and nurses work together in harmony to care for mothers and babies in one place, as a unit.”
KMC has been shown to significantly improve survival and health outcomes for preterm and low birthweight babies, compared to clinical stabilization in a more ‘high-tech’ incubator or warmer. In fact, data shows it can increase preterm survival rates by as much as a third, reduce infections, prevent hypothermia, and improve feeding and growth. It is also empowering and reassuring for mothers and families who take a leading role in providing care for their infants.
Despite these benefits, only around a third of countries are estimated to have an updated policy or guideline on KMC, meaning millions of preterm and low birthweight babies are likely to be missing out on this lifesaving technique.
The new documents outline some key actions that should be taken to enable the wider adoption and implementation of KMC:
- Governments should recognize and include KMC as essential care for all preterm or small babies, ensuring it is financed and monitored – including the necessary infrastructure changes within hospitals – as part of national programmes. Additional parental leave and entitlements can help address the special needs of caregivers of preterm or low birthweight infants so that they can provide the requisite care.
- Facilities and healthcare providers should help ensure small and preterm babies can benefit from skin-to-skin contact with their mother for the recommended 8-24 hours a day, starting immediately after birth.
- Critically, both mother and newborn should receive respectful care, together, as a unit – even when the infant is sick and requires care inside the newborn care unit.
- Parents and caregivers should be involved in routine care and all aspects of decision-making around care for their newborns. They should be supported – with coaching, emotional and practical assistance – to provide KMC for their small and preterm babies.
- Partners and family members can help in providing KMC, providing relief for the mother, stepping in if she is unwell, and helping meet her needs while she is caring for her baby.
Developed in collaboration with a multi-country, multi-stakeholder working group, these resources are directed to governments, programme partners, policy makers and the broader public health community, to help countries expand KMC for babies born early or small. Around the world, WHO is providing ongoing assistance in implementing and scaling up KMC as the foundation of small and/or sick newborn care within national maternal, newborn and child health programmes.
Editor’s note:
The Working Group that developed these documents is comprised of various scientific experts, Ministries of Health and representatives from UN agencies (UNICEF, the World Bank, WHO), bilateral agencies (USAID, Japan International Cooperation Agency -JICA, Norwegian Agency for Development Cooperation-NORAD, the Foreign and Commonwealth Development Office of the United Kingdom- UK-FCDO), donor organizations (Bill and Melinda Gates Foundation, the Children’s Investment Fund Foundation (CIFF), Laerdal Foundation), parents groups (European Foundation for the Care of Newborn Infants, FUNDAPREMA, Preemie Connect), professional associations (the American Academy of Pediatrics,, Council of International Neonatal Nurses (COINN), the International Confederation of Midwives, the International Federation of Gynecology and Obstetrics (FIGO), the International Pediatric Association), and non-governmental organizations (Kangaroo Foundation, Médecins sans Frontières, Save the Children) and specialized partnerships like the Partnership for Maternal, Newborn and Child Health.

What Is Hygge, and Why Is It Good for Your Well-Being?

Taking cues from the Danish art of getting comfy and cozy can definitely be a way to practice self-care.
By Stacey Colino Medically Reviewed by Allison Young, MD November 3, 2022
Practicing hygge is all about doing things we know are good for lowering stress and boosting wellness, from drinking warm, soothing beverages to spending time with people we care about.
People have been talking about “hygge” for a few years now. It’s the Danish word for coziness or feeling warm, comfortable, and safe, according to the Cambridge Dictionary. It was back in 2016 that The New Yorker reported it was the “year of hygge.”
And wellness experts say that if you haven’t joined the trend yet, these colder weather months are the perfect time to do so.
It’s not so much an activity you might choose to do or not do; hygge is more a way of life, one that makes ordinary moments feel special, pleasurable, and meaningful, according to Meik Wiking, CEO of the Happiness Research Institute and the author of The Little Book of Hygge: Danish Secrets to Happy Living.
The concept of hygge is about creating a cozy, comforting physical environment: lighting candles, snuggling up with soft blankets, and consuming warm, soothing drinks. But it’s also (and perhaps more importantly) a mindset and a philosophy, Wiking explains.
“Hygge is about an atmosphere and an experience, rather than about things,” Wiking says. Hygge is also about creating a comforting social and emotional environment for yourself; it’s about who you choose to surround yourself with and what you choose to spend your time doing.
“It is about being with the people we love; a feeling that we are safe, that we are shielded from the world and are allowing ourselves to let our guard down,” Wiking says.
It’s not just the cooler weather that may make adopting a hygge mindset attractive; it’s a way to take care of yourself during a time filled with all sorts of worldwide stressors and negative news cycles, says Holly Schiff, PsyD, a Connecticut-based licensed clinical psychologist for Jewish Family Services of Greenwich.
“During this time of uncertainty and stress, we crave consistency, predictability, and a sense of control,” Schiff explains. As such, she notes that hygge practices and its emphasis on self-care can help individuals exercise control amid uncontrollable circumstances.
A note on pronunciation: For us English speakers, “HUE-geh” is pretty close. Complicating matters, the word can be used as a noun, a verb, and an adjective. “Hygge” in both Danish and Norwegian means “coziness,” and is derived ultimately from Old Norse. As a concept and cultural practice, hygge became popular in Denmark in the 19th century as a celebration of comfortable conviviality during the long, dark Scandinavian winters, Wiking says.
The Benefits of Hygge and Why It’s Self-Care
Hygge may be part of the reason why Denmark consistently ranks among the happiest countries on the planet, alongside Finland, Norway, and Switzerland (these rankings come from the annual World Happiness Report).
Experiencing hygge reportedly reduces stress and improves emotional well-being, though there isn’t any scientific research examining the perks of the practice as a whole. “The support for hygge comes from its independent components — it hasn’t been tested as a set of environmental conditions,” notes Sally Augustin, PhD, environmental and design psychologist, and principal at the Chicago-based design firm Design With Science. Dr. Augustin’s work focuses on using design in science-backed ways to improve cognitive, emotional, and physical experiences.
For example, research published in the February 2020 issue of the journal Ergonomics found that people perceived warm, dimmer light as more relaxing than bright, white lights.
In addition, there’s strong evidence that having nurturing social connections (another component of hygge — spending time with friends and family) is beneficial for physical and emotional health; several such studies are included in a review published in 2018 in the journal Annual Review of Psychology.
Previous research has also shown, for example, that when premenopausal women get more frequent hugs from their partners, they have higher levels of oxytocin (often called the “love hormone” or the “cuddle hormone”) as well as lower blood pressure and heart rate.
Science has also shown that being around certain scents (yes, aromatherapy counts) can induce relaxation: A study from Japan found that when women were exposed for 90 seconds to air infused with the scent of rose or orange essential oil, it induced physiological relaxation in their brains and led to an increase in “comfortable” and “relaxed” feelings.
What’s more, “when we’re in a more positive or relaxed mood, we get better at problem-solving, we think more creatively, and we get along better with each other,” Augustin says. All these potential benefits of practicing hygge explain why and how it can be a method of self-care.
Additionally, Schiff notes that hygge principles, including those involving self-care, could have positive mental health implications. These include less stress, reduced anxiety, and better mood overall.
In one of the few studies that has looked at practicing hygge, researchers found that the lifestyle had significant positive impacts from women in a women’s correctional facility in Denmark who used hygge practices, such as food and props in their cells to create a hygge environment. Results from the small study (it only involved 9 women) were reported in 2019 in the journal Appetite.
How to Make Hygge Part of Your Life
Why does creating a cozy, inviting, appealing environment make a difference in terms of our well-being? “It’s about creating environmental flow and warmth, about making you feel comfortable and cozy through visual, spatial, and other sensory properties,” says Allen Elkin, PhD, a clinical psychologist based in New York City and author of Stress Management for Dummies.
How do you get started with creating the hygge effect? It’s really up to you. “The important thing to remember is that your environment does influence how you feel — and you can take control of your environment and actually make it really good,” Augustin says. That “taking control” aspect is really important, she adds. “One of our fundamental human motivations is to feel that we have an element of autonomy in our lives” — that you have options in terms of what you do.
To that end, you can choose from the following strategies to get started with hygge and practice it as a form of self-care.
Opt for mood lighting. At home, dim the lights and light some candles. Or make a fire in the fireplace if you can do so safely. Or, buy warm amber bulbs for your lamps and light fixtures then “turn on whatever is appropriate at any particular moment,” Augustin suggests.
Hang out with a small circle of close friends. “The most important social relationships are close relationships in which you experience things together with others, and experience being understood; where you share thoughts and feelings; and both give and receive support,” Wiking explains. That togetherness is the essence of hygge.
Make yourself comfortable. Add flannel or fleece blankets, pillows, and throws to your home environment for snuggling opportunities. Go casual and wear comfy, loose pullovers, leggings or jeans you’re not afraid to get wrinkled, thick socks that keep your feet warm, and big scarves (a Danish signature). “Opt for soft textures that feel good against your skin,” Augustin advises.
Establish a comforting bedtime ritual and space. Aside from sticking with a regular sleep schedule, Schiff recommends creating your sleeping space as comfortable and cozy as possible, per the hygge philosophy. “Cuddle up with some hot tea, wrap yourself in a warm blanket, and make your bedroom the most relaxing place in the house,” she suggests. Try breathing exercises for more relaxation, she says.
Get cooking. Food and beverages are a big part of the hygge experience. It’s about pleasure, so go ahead and enjoy sweets, cakes, hot chocolate, mulled wine, and other tasty treats. “Few things contribute more to the hygge factor than the smell of fresh baked goods,” Wiking says. So roll up your sleeves and bake something delicious at home (by yourself or with friends). Remember: “Hygge food may be comfort food,” Wiking says, “but hygge food is also very much slow food” — meaning, part of the magic is in its preparation.
Relish the here and now. Mindfulness and gratitude are key components of hygge, says Schiff. Turn off your phone and other digital devices and focus on the present moment. Listen to music that soothes your heart and soul. Light a candle and treat yourself to good scents that have a calming effect (think: lavender, rose, jasmine, or bergamot). Read an enjoyable book or play a fun board game with friends or family. Hygge is about giving the responsible, stressed-out, perhaps overachieving part of yourself a break, says Wiking. It’s about joy and contentment. “It is about experiencing happiness in simple pleasures and knowing that everything is going to be okay.”
Source:https://www.everydayhealth.com/wellness/what-is-hygge-and-why-is-it-good-for-your-wellbeing/

PREEMIE FAMILY PARTNERS

Improving the lives of parents of neonatal patients: 2023 Curtin Medalist Joanne Beedie

Joanne is the CEO and co-founder of Helping Little Hands, a charity that has supported thousands of Western Australian families with premature and sick babies in the Neonatal Intensive Care Unit (NICU) at King Edward Memorial Hospital. A mother of five, Joanne has firsthand experience of the NICU rollercoaster when her twin son Lewis was born at 27 weeks’ gestation. Tragically, she lost his brother Logan at just 21 weeks. Determined to use her own lived experience to help others, Joanne set up her charity to provide practical assistance, financial aid, peer support and advocacy to struggling families. Helping Little Hands focuses on stepping in when families fall between the gaps in government services; providing petrol vouchers, cots and car seats; funding accommodation for Aboriginal mothers; and raising hundreds of thousands of dollars to fund essential medical equipment. Congratulations Joanne, on receiving the 2023 John Curtin Medal. The John Curtin Medal is awarded to those who have made a remarkable difference to the world we live in, and who have exhibited John Curtin’s qualities of vision, leadership and community service.

Your BABY had a desaturation or desat? The NICU Doc Explains on the What is…? series


It’s science: Premature babies have fewer siblings
By Stephanie Loomis Pappas February 25, 2019

Do you have kids? When are you having kids? How old are your kids?
Our questions about other people’s children are often asked as plurals. “Kids” not “kid” is the default assumption, but it is time for us to rethink the language we use. Asking a stranger at the grocery store “Are they your first?” suggests, however innocently, that a parent ought to have a “second”, but some parents are not keen to go through birth more than once.
A study in the journal Pediatrics suggests that whether or not a child is “first” or “only” depends in part on how early they was born, and how traumatic it was for their parents.
Researchers at Finland’s National Institute for Health and Welfare (THL) identified all 230,308 recorded singleton infants born in Finland between January 1987 and September 1990 and interviewed those infants’ parents.
The study revealed that parents of infants born preterm were less likely to have subsequent children than parents whose born at term. Infants born “extremely” preterm (between 23 and 27 weeks) were the least likely to have a subsequent sibling, but even those born nearly at term (between 34 and 36 weeks) were less likely to have a subsequent sibling. The researchers concluded that for every 1,000 preterm births, there were 142 “missing siblings” from parents who would have been statistically likely to have more children.
A THL press release put the results in simple terms: “The more premature a child is born, the greater the probability that it will be the last child in the family.”
The researchers have not determined a cause for this lowered birth rate among parents of preterm infants, but speculate that the lowered rate “may reflect the crisis a premature birth may cause for the parents and its far-reaching impact. The birth of a premature infant is often a surprise, and can place the parents in a situation where their hopes and resources do not meet their expectations on parenting or the challenges during early childhood.”
In other words, parents’ experiences with their preterm children – which may include harrowing weeks or months in neonatal intensive care units as well as lifelong health problems – may make them more hesitant to have more children. The sole exception were parents whose children born preterm died within their first year. Those parents were actually more likely to have subsequent children.
In a post to the American Academy of Pediatrics’ blog, editor-in-chief Lewis First stresses that the issue will require further study before researchers can draw a causal link between preterm birth and the subsequent birth rate.
In the interim, however, we might want to consider the pain inflicted by probing questions about subsequent children. There’s no need to ask a family member when she’s planning to have more kids. Instead of asking these kinds of close-ended questions about family planning and family size, we could all do better by asking open-ended questions about the kid who is actually right there in front of us.

Advice for NICU moms from a NICU mom

Welcoming a new baby into the family is a massive transition. But when the baby arrives earlier than expected, the stress can feel overwhelming. For parents of a premature baby, having support can help lighten the load.


HEALTHCARE PARTNERS

Insights on Residency Training
Notes from chief residents in family and internal medicine.

Dr. Temte is a Chief Resident in Internal Medicine at Providence Portland Medical Center in Portland, OR.
We currently find ourselves at the start of another academic year. By this time in August, many medical trainees are settling into new roles. Recently graduated medical students are getting used to hearing Dr. before their name. New senior residents who were interns a short time ago now find themselves leaders of their own teams. As for myself, I am starting a pulmonary and critical care fellowship at a new academic center. By August, all these training doctors are considering the question of how they will lead and teach in their new roles.
Throughout medical school, we have the privilege of being taught by excellent instructors. While all our instructors had various pros and cons, very few of them provided dedicated instruction on how to be leaders and educators. Most residents have observed that their fellow residents doing most of the teaching. Early on, we model our teaching tactics based on what we’ve observed during our own learning. However, I found very quickly as I advanced from medical student to senior resident that it is a bit more complex than teaching others in the way that I would like to be taught. Diagnosing the learner and effectively teaching the student in front of me requires intention and training.
Residents as Teachers
At my residency program, we were fortunate to be able to create a Residents as Teachers program during the height of the COVID-19 pandemic. During the first few months of 2020, some clinic and elective time was canceled, which created an unexpected opening in our schedules. While we were at home working on research and learning via Teams, a few of us came together with our best teaching attendings and started to create a curriculum.
Luckily, many successful Residents as Teachers programs have been instituted at other programs, and we modeled our intervention after them. Together, we created resident-led workshops, curriculum, syllabus, and an elective rotation. During the 2021-2022 year, we had our inaugural Residents as Teachers session. We focused primarily on instructing second- and third-year residents and were excited to have 9 of the 18 senior residents join our group. As a result of the program, we’ve participated in some excellent teaching workshops, had more resident-led noon conferences, and increased teaching on the hospital wards.
One prerequisite for a Residents as Teachers certification was to get involved in a medical education project. This requirement has led to an improved simulation lab, medical student curriculum, and further POCUS teaching. To this day, helping to create and lead the first year of our Residents as Teachers is one of my favorite projects.
Resident Educator Tips – What I’ve Learned So Far
Resident-led education is so important and can create a meaningful impact for both the teacher and learner. During this last part of the article, I’ll leave you with a few tips I’ve acquired from my mentors. These are not all-encompassing but are a great place to start during your early career as a medical educator.
- Get involved in teaching. This may be daunting at first, especially early in your career. However, we all have something we are interested in and can pass along to our fellow trainees. Practice makes progress when it comes to teaching.
- Create psychological safety. Everyone learns best in a safe environment that is free of ridicule and undue stress. Bloggers on our site have discussed psychological safety before — for those interested in learning more.
- Focus on illness scripts. Many new learners are still building their pattern recognition skills. Comparing and contrasting illness scripts for a presenting illness can solidify clinical reasoning around a particular disease or framework.
- Teach one or two things at a time. Once you find a teaching point or area of improvement, focus on providing instruction around a few key takeaways. Make sure to emphasize the key points you want your learner to remember at the end of the lesson.
- Set clear goals and expectations. Make sure everyone knows how, when, and who will be doing the teaching.
- Prepare a few talks on your favorite subjects. This is your chance to dive deeply into an interesting topic and be the go-to expert on this subject.
- Provide take-home materials. This can be something as simple as a paper to read afterward or a framework you’ve created.
- Seek out frequent feedback. Having a mentor or an educator you look up to provide feedback on your teaching can be an invaluable experience.
- Join your residency’s Residents as Teachers program. If you do not have a Residents as Teachers program, creating one can help expand the education culture of your residency and be very rewarding.
I believe we all have a duty to train the next generation and pay it forward. Improving your skills as an educator will not only help the field of medicine but also improve your skills as a physician. I hope everyone experiences the joy of helping someone along their professional journey.
Source: https://blogs.jwatch.org/general-medicine/

HealthySimulation – Medical Simulation Resources Mar 23, 2023 #IMSH2023
https://HealthySimulation.com was provided a demonstration of the latest #ClinicalSimulation pediatric neonate technologies from SIMCharacters @SIMCharacters at #IMSH2023 !
Walking the PATH: Guidelines for Attending Physicians, APPs, and Trainees
Scott D. Duncan, M.D., M.H.A.
In the sweltering heat of the summer, medical students, residents, and fellows begin the next stage of their career journey. Recently graduated fellows become attending physicians with expanded responsibilities, including supervision of trainees. However, in the current healthcare environment, provider shortages, and reduced intensive care training requirements demand unique solutions for the provision of patient care. One option to expand the workforce is to include APPs as employed qualified healthcare providers.
Depending on the employment model, scope of practice, and state regulations, APPs may bill independently for services. In many academic institutions, both physicians and APPs are employed by provider organizations, separate from the hospital or university. With the expansion of types of healthcare providers found in the NICU, a trainee may interact with an attending neonatologist and/ or APP. In some academic institutions, an APP may supervise a trainee. These different training and employment models require an understanding supervision and correct billing practices.
Given the following codes, the correct coding for the neonatologist includes:
Q 1: On the first day of service, a neonatologist in a teaching hospital attends a delivery with a pediatric resident. The infant is apneic at birth and requires PPV via face mask. The neonatologist instructed the resident to intubate the infant, which the resident accomplished under direct bedside supervision. The infant required additional PPV via an endotracheal tube, with subsequent recovery. The infant was subsequently transferred to the NICU.
99465 – Delivery Room Resuscitation 31500 – Intubation
A. 99465, 31500
B. 99465
C. 31500
D. There was no billable service
Q 2: On the first day of service, a neonatologist in a teaching hospital attends a delivery with an APP, is employed by the care provider group, and is permitted to bill under state regulations. The infant is apneic at birth and requires PPV via face mask. The neonatologist instructs the APP to intubate the infant, which was accomplished by the APP. The infant required PPV via an endotracheal tube, with subsequent recovery. The infant was subsequently transferred to the NICU.
Correct coding includes:
A. 99465 by the neonatologist, 31500 by the APP
B. 99465 by the APP
C. 99465,31500 by the neonatologist
D. There was no billable service
Q 3: On the first day of service, an APP in a teaching hospital attends a delivery with a pediatric resident. The infant is apneic at birth and requires PPV via face mask. The APP instructed the resident to intubate the infant, which the resident accomplished under direct bedside supervision. The infant required PPV via an endotracheal tube with subsequent recovery. The infant was subsequently transferred to the NICU. Correct coding for the APP includes:
A. 99465
B. 99465, 31500
C. 31500
D. There was no billable service
In each of the preceding scenarios, the correct answer is A. The focus of the questions is based on the supervision of trainees and the collaboration of care providers. In the first scenario, the neonatologist is supervising a trainee. Supervision and proper coding are dictated by Teaching Physicians, Interns & Resident Guidelines, published by the Centers for Medicare & Medicaid Services, often referred to as Physician at Teaching Hospitals or PATH guidelines. These guidelines can be found here: www.cms. gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/teaching-physicians-fact-sheet-icn006437. pdf. When a teaching physician supervises a resident trainee, the physician must ensure proper documentation, demonstrating their involvement in the patient’s care. In this case, a delivery room note detailing the request for attendance at delivery, services provided,
Similarly, according to PATH guidelines, an APP is not considered a supervising physician. As such, in the third scenario, the APP may bill for the resuscitation, as this would be considered their work. However, the APP cannot bill for the intubation performed by the resident. Appropriate documents should be included in the medical record by the APP for the attendance at delivery and the infant’s resuscitation, as well as a procedure note by the resident for the intubation of the infant. As new models of providing patient care are developed and supervision of trainees shifts to include APPs, it is paramount to walk the correct PATHway!
Source:http://neonatologytoday.net/newsletters/nt-aug23.pdf

Improved exclusive breastfeeding rates in preterm infants after a neonatal nurse training program focusing on six breastfeeding-supportive clinical practices.
Maastrup R 1,2, Rom AL 2, Walloee S 3, Sandfeld HB 4, Kronborg H 5

Abstract
Background
Early breast milk expression, prolonged skin-to-skin contact, rooming-in, use of test-weighing and minimizing use of pacifiers are positively associated with exclusive breastfeeding of preterm infants, whereas use of nipple shields is negatively associated.
Aim
To test whether a training program for neonatal nurses with a focus on these six breastfeeding-supportive clinical practices affects the rate of preterm infants exclusively breastfed at discharge to home, the postmenstrual age at establishment of exclusive breastfeeding, and maternal self-reported use of the practice in the neonatal intensive care unit.
Methods
A quasi-experimental multi-centre intervention study from 2016-2019 including a control group of 420 preterm mother-infant dyads, an intervention with a training program for neonatal nurses and implementation of weekly breastfeeding meetings for neonatal nurses, and an intervention group of 494 preterm mother-infant dyads.
Results
Significantly more preterm infants in the intervention group were exclusively breastfed at discharge to home (66.6%) than in the control group (58.1%) p = 0.008. There was no significant difference in postmenstrual age at establishment of exclusive breastfeeding between control and intervention group (37.5 vs.37.8 weeks, p = 0.073). Compared to the control group the number of infants continuing daily skin-to-skin contact after incubator care increased (83.2% vs. 88.3%, p = 0.035), infants using a nipple shield decreased (61.8% vs. 54.2%, p = 0.029), and the number of mothers initiating breast milk expression before six hours post-partum increased (32.6% vs. 42.4%, p = 0.007). There was a significant correlation between percentage of neonatal nurses participating in the breastfeeding training program and changes in exclusive breastfeeding rates (Pearson Correlation 0.638, p = 0.047).
Conclusion
Exclusive breastfeeding rates in preterm infants and maternal self-reported use of breastfeeding-supportive practices increased by training neonatal nurses in the six clinical practices. It is important to include all nurses in the breastfeeding training program to ensure positive effect on exclusive breastfeeding rates.
Source:https://europepmc.org/article/pmc/7857627
INNOVATIONS
Eat, Sleep, Console Approach or Usual Care for Neonatal Opioid Withdrawal

Leslie W. Young, M.D., Songthip T. Ounpraseuth, Ph.D., Stephanie L. Merhar, M.D., Zhuopei Hu, M.S., Alan E. Simon, M.D.,Andrew A. Bremer, M.D., Ph.D., Jeannette Y. Lee, Ph.D., Abhik Das, Ph.D., Margaret M. Crawford, B.S., Rachel G. Greenberg, M.D., P. Brian Smith, M.D., Brenda B. Poindexter, M.D.
ABSTRACT
BACKGROUND
Although clinicians have traditionally used the Finnegan Neonatal Abstinence Scoring Tool to assess the severity of neonatal opioid withdrawal, a newer function-based approach — the Eat, Sleep, Console care approach — is increasing in use. Whether the new approach can safely reduce the time until infants are medically ready for discharge when it is applied broadly across diverse sites is unknown.
METHODS
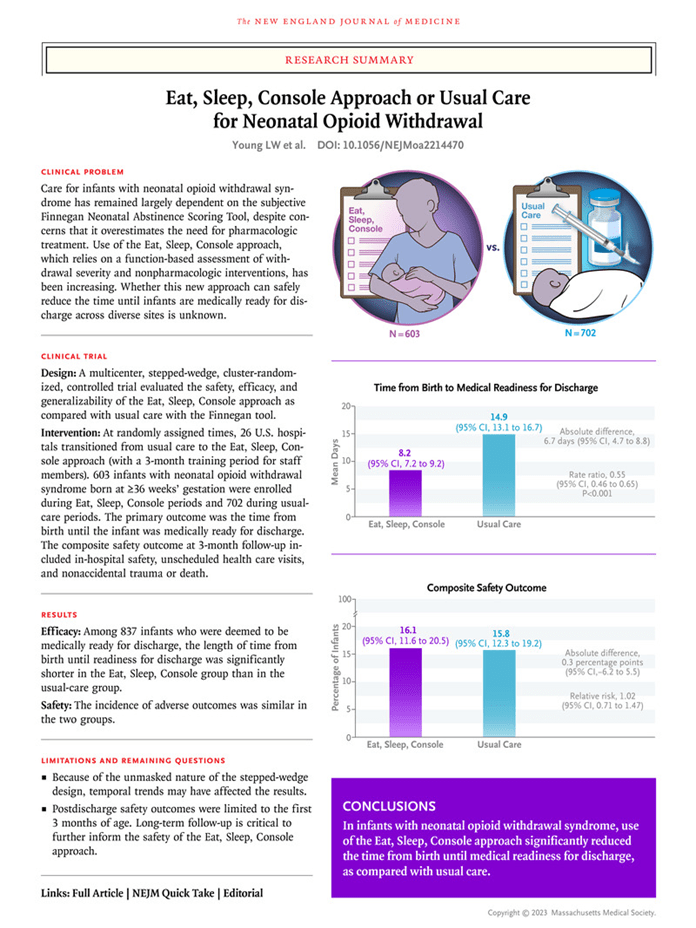
In this cluster-randomized, controlled trial at 26 U.S. hospitals, we enrolled infants with neonatal opioid withdrawal syndrome who had been born at 36 weeks’ gestation or more. At a randomly assigned time, hospitals transitioned from usual care that used the Finnegan tool to the Eat, Sleep, Console approach. During a 3-month transition period, staff members at each hospital were trained to use the new approach. The primary outcome was the time from birth until medical readiness for discharge as defined by the trial. Composite safety outcomes that were assessed during the first 3 months of postnatal age included in-hospital safety, unscheduled health care visits, and nonaccidental trauma or death.
RESULTS
A total of 1305 infants were enrolled. In an intention-to-treat analysis that included 837 infants who met the trial definition for medical readiness for discharge, the number of days from birth until readiness for hospital discharge was 8.2 in the Eat, Sleep, Console group and 14.9 in the usual-care group (adjusted mean difference, 6.7 days; 95% confidence interval [CI], 4.7 to 8.8), for a rate ratio of 0.55 (95% CI, 0.46 to 0.65; P<0.001). The incidence of adverse outcomes was similar in the two groups.
CONCLUSIONS
As compared with usual care, use of the Eat, Sleep, Console care approach significantly decreased the number of days until infants with neonatal opioid withdrawal syndrome were medically ready for discharge, without increasing specified adverse outcomes. (Funded by the Helping End Addiction Long-term (HEAL) Initiative of the National Institutes of Health; ESC-NOW ClinicalTrials.gov number, NCT04057820. opens in new tab.)
Source:https://www.nejm.org/doi/full/10.1056/NEJMoa2214470
Eye-Tracking–Based Measurement of Social Visual Engagement Compared With Expert Clinical Diagnosis of Autism
Warren Jones, PhD1,2,3; Cheryl Klaiman, PhD1,2; Shana Richardson, PhD1; et alChrista Aoki, PhD1; Christopher Smith, PhD4; Mendy Minjarez, PhD5; Raphael Bernier, PhD5; Ernest Pedapati, MD6; Somer Bishop, PhD7; Whitney Ence, PhD7; Allison Wainer, PhD8; Jennifer Moriuchi, PhD8; Sew-Wah Tay, PhD9; Ami Klin, PhD1,2,3JAMA. 2023;330(9):854-865. doi:10.1001/jama.2023.13295 September 5, 2023
Key Points
Question Can eye-tracking–based measurement of social visual engagement aid in early diagnosis and assessment of autism in young children?
Findings In a multisite, prospective, double-blind study of 475 children aged 16 to 30 months assessed for autism in 6 specialty clinics, measurement of social visual engagement had 71.0% sensitivity and 80.7% specificity relative to expert clinical diagnosis. In the subgroup of children whose autism diagnosis was certain (n = 335), the test had 78.0% sensitivity and 85.4% specificity.
Meaning Eye-tracking–based measurement warrants further evaluation for early diagnosis and assessment of autism in young children referred to specialty clinics.
Abstract
Importance In the US, children with signs of autism often experience more than 1 year of delay before diagnosis and often experience longer delays if they are from racially, ethnically, or economically disadvantaged backgrounds. Most diagnoses are also received without use of standardized diagnostic instruments. To aid in early autism diagnosis, eye-tracking measurement of social visual engagement has shown potential as a performance-based biomarker.
Objective To evaluate the performance of eye-tracking measurement of social visual engagement (index test) relative to expert clinical diagnosis in young children referred to specialty autism clinics.
Design, Setting, and Participants In this study of 16- to 30-month-old children enrolled at 6 US specialty centers from April 2018 through May 2019, staff blind to clinical diagnoses used automated devices to measure eye-tracking–based social visual engagement. Expert clinical diagnoses were made using best practice standardized protocols by specialists blind to index test results. This study was completed in a 1-day protocol for each participant.
Main Outcomes and Measures Primary outcome measures were test sensitivity and specificity relative to expert clinical diagnosis. Secondary outcome measures were test correlations with expert clinical assessments of social disability, verbal ability, and nonverbal cognitive ability.
Results Eye-tracking measurement of social visual engagement was successful in 475 (95.2%) of the 499 enrolled children (mean [SD] age, 24.1 [4.4] months; 38 [8.0%] were Asian; 37 [7.8%], Black; 352 [74.1%], White; 44 [9.3%], other; and 68 [14.3%], Hispanic). By expert clinical diagnosis, 221 children (46.5%) had autism and 254 (53.5%) did not. In all children, measurement of social visual engagement had sensitivity of 71.0% (95% CI, 64.7% to 76.6%) and specificity of 80.7% (95% CI, 75.4% to 85.1%). In the subgroup of 335 children whose autism diagnosis was certain, sensitivity was 78.0% (95% CI, 70.7% to 83.9%) and specificity was 85.4% (95% CI, 79.5% to 89.8%). Eye-tracking test results correlated with expert clinical assessments of individual levels of social disability (r = −0.75 [95% CI, −0.79 to −0.71]), verbal ability (r = 0.65 [95% CI, 0.59 to 0.70]), and nonverbal cognitive ability (r = 0.65 [95% CI, 0.59 to 0.70]).
Conclusions and Relevance In 16- to 30-month-old children referred to specialty clinics, eye-tracking–based measurement of social visual engagement was predictive of autism diagnoses by clinical experts. Further evaluation of this test’s role in early diagnosis and assessment of autism in routine specialty clinic practice is warranted.

Neonatal Healthcare Professionals’ Experiences When Implementing a Simulation and Debriefing Program in Neonatal Intensive Care Settings
A Qualitative Analysis
Quinn, Jenny PhD, APRN, NNP-BC; Quinn, Megan PhD, RNC-NIC; Lieu, Brandon BS; Bohnert, Janine BS; Halamek, Louis P. MD; Profit, Jochen MD; Fuerch, Janene H. MD; Chitkara, Ritu MD; Yamada, Nicole K. MD; Gould, Jeff MD; Lee, Henry C. MD
Abstract
Background:
Simulation-based training (SBT) and debriefing have increased in healthcare as a method to conduct interprofessional team training in a realistic environment.
Purpose:
This qualitative study aimed to describe the experiences of neonatal healthcare professionals when implementing a patient safety simulation and debriefing program in a neonatal intensive care unit (NICU).
Methods:
Fourteen NICUs in California and Oregon participated in a 15-month quality improvement collaborative with the California Perinatal Quality Care Collaborative. Participating sites completed 3 months of pre-implementation work, followed by 12 months of active implementation of the simulation and debriefing program. Focus group interviews were conducted with each site 2 times during the collaborative. Content analysis found emerging implementation themes.
Results:
There were 234 participants in the 2 focus group interviews. Six implementation themes emerged: (1) receptive context; (2) leadership support; (3) culture change; (4) simulation scenarios; (5) debriefing methodology; and (6) sustainability. Primary barriers and facilitators with implementation of SBT centered around having a receptive context at the unit level (eg, availability of resources and time) and multidisciplinary leadership support.
Implications for Practice and Research:
NICUs have varying environmental (context) factors and consideration of unit-level context factors and support from leadership are integral aspects of enhancing the successful implementation of a simulation and debriefing program for neonatal resuscitation. Additional research regarding implementation methods for overcoming barriers for both leaders and participants, as well as determining the optimal frequency of SBT for clinicians, is needed. A knowledge gap remains regarding improvements in patient outcomes with SBT.


Ladybug Body Scan – 7 Minute Mindful Meditation for Kids

Feb 3, 2022 #kidsmeditation #mindfulnessforkids #bodyscanmeditation
Welcome to BrightenUp! Kids, we provide free meditation and mindfulness content for children of all ages! In this guided 7-minute body scan video, we play a fun relaxing game using our imaginations to practice mindfulness and body awareness with the help of a ladybug friend! About body scan activities: Body scan meditation is a mindfulness tool used to bring awareness to different parts of the body. This can be a fun exercise for building more body and emotional awareness and can help aid with relaxation.


MINDFULNESS – 3 MINUTE MEDITATION
Mindfulness has been shown to be very beneficial. (details below) Join our community/see our products: https://www.thehonestguys.co.uk/products In this short 3 minute exercise you’ll learn that you can to be completely present in the current moment, letting go of your thoughts and achieving calmness, at any time you choose.
THE HONEST GUYS We create effortless ways for anyone to reach a profound sense of deep relaxation, meditation and sleep, without ever having to try. In particular, we cater to anyone who is turned-off by the idea of “meditation”, but still want to reap the massive health benefits, that meditation can bring. We offer this through high-quality audio productions, called ‘guided visualisations’. These include sleep talk-downs, meditations, wonderful fantasy imagery and stories.



Hey Warriors, did you know that some of the most famous and beloved people in the world were born prematurely, just like many of our brave little fighters in the neonatal community? One such incredible individual is none other than the famous actor and action hero, Dwayne “The Rock” Johnson! That’s right, before he was the tough guy we see on the big screen, he was a tiny baby who couldn’t wait to make his grand entrance into the world. Born two months premature, baby Dwayne faced his early challenges head-on, and look at him now – a real-life superhero inspiring us all to be strong and resilient, just like him!”
Another remarkable person born prematurely is the musical sensation, Stevie Wonder. Long before he was a Grammy-winning artist and an icon in the music industry, he was a little preemie who showed the world the incredible power of determination and talent. Born six weeks early, Stevie didn’t let his early start hold him back. Instead, he used his love for music to create timeless hits that continue to touch the hearts of people of all ages.
So, to all the parents with preemies in the neonatal community, remember that your little ones may be tiny, but they have the potential to achieve greatness that knows no bounds. Keep nurturing their dreams, just like these famous preemies’ families did, and who knows what amazing things they’ll accomplish one day!
To all the superheroes working tirelessly in neonatal units, take heart in the knowledge that you’re in illustrious company. Your dedication and care are invaluable in shaping the futures of these little miracles. Together, you’re helping to write remarkable stories of strength and resilience that will inspire generations to come.
And, to all the neonatal warriors out there, remember that you are in excellent company with these famous figures and our Neonatal Womb Warrior/Preterm Birth Community at large.

😄💜🙌🏾 Children’s Book Read Aloud: GO Preemies! By: A.P. Male
On this episode of Nighty Nights with Miss Neli, we will be reading Go Preemies! By A.P. Male! Book Description: This book tells readers all about Famous Preemies who grew big and strong to do amazing things in this world!

Albert Einstein-Preemie

Lee-Ann Curren & Tom Curren surfing Cold Hawaii in Denmark
=
Panic Magazine 🇩🇰
Claudia Lederer captured a few waves of Lee-Ann Curren & Tom Curren during a short stay in Cold Hawaii, Klitmøller, Denmark. Locals gave evidence of unique dance moves while father and daughter were playing music together for the Ocean Love Festival.