

Argentina, officially the Argentine Republic, is a country in the southern half of South America. Argentina covers an area of 2,780,400 km2 (1,073,500 sq mi), making it the second-largest country in South America after Brazil, the fourth-largest country in the Americas, and the eighth-largest country in the world. It shares the bulk of the Southern Cone with Chile to the west, and is also bordered by Bolivia and Paraguay to the north, Brazil to the northeast, Uruguay and the South Atlantic Ocean to the east, and the Drake Passage to the south. Argentina is a federal state subdivided into twenty-three provinces, and one autonomous city, which is the federal capital and largest city of the nation, Buenos Aires. The provinces and the capital have their own constitutions, but exist under a federal system. Argentina claims sovereignty over the Falkland Islands, South Georgia and the South Sandwich Islands, the Southern Patagonian Ice Field, and a part of Antarctica.
Argentina‘s health care system is composed of a universal health care system and a private system. The government maintains a system of public medical facilities that are universally accessible to everyone in the country, but formal sector workers are also obligated to participate in one of about 300 labor union-run health insurance schemes, which offer differing levels of coverage. Private medical facilities and health insurance also exist in the country. The Ministry of Health (MSAL), oversees all three subsectors of the health care system and is responsible for setting of regulation, evaluation and collecting statistics.
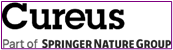
GLOBAL PRETERM BIRTH RATES – ARGENTINA
Estimated # of preterm births: 8% (USA 9.56-Global Average: 10.6)
Source:https://data.un.org/Data.aspxd=WHO&f=MEASURE_CODE%3AWHS_PBR

COMMUNITY

Young Argentine medical professionals force government to back down and withdraw law
The government of Buenos Aires withdrew a law that defined medical residents and concurrents as trainees and stripped them of labor right. This followed continuous mass protests by the medicos
December 07, 2019 by Peoples Dispatch
The young Argentine health professionals staged a number of protests in the first week of December against the law. Photo: Photo: Assembly of Residents and Concurrents of CABA.
Thousands of young Argentine healthcare professionals won a victory on December 5, Thursday, when the government withdrew a law that did not recognize them as health workers and promoted their exploitation. The victory came after a massive demonstration held outside the Buenos Aires city hall on December 4.
The protests were led by the Assembly of Residents and Concurrents of CABA.
Following the mass protests, the head of the government of Buenos Aires, Horacio Rodriguez Larreta, moved a resolution in the city legislature that revoked the Law of Residents and Concurrents of CABA. The motion was passed. In addition, Larreta promised to draft a new law after cosulting residents, concurrents and their union.
The residents and concurrents are medics who work and receive in-service training in public hospitals of Buenos Aires as part of the city’s healthcare system. Residents are full-time workers who get paid for providing their services. Concurrents are part-time workers who do not receive any remuneration.
The law disregarded their status as healthcare professionals and termed them as trainees. It also defined their work in emergency departments as a “continuous intensive training process.” The law set a minimum work duration of 36 hours and a maximum of 64 hours per week, making it unhealthy for both professionals and the people who access their services.
It also took away the right to take part in collective negotiation processes and reduced maternity or paternity leaves from 30 to 14 and stress leaves from 10 to 7. It made marking attendance compulsory, thus guaranteeing a precarious labor force, since it included concurrents, who do not receive salary or other labor rights, but comply with the same practices as residents and other healthcare professionals.
The law was passed on November 28, while on the streets, the doctors protesting against it were repressed by the police. The bill was presented on November 20, one week before it was voted on, without consulting the professionals involved and without enough time for discussion.

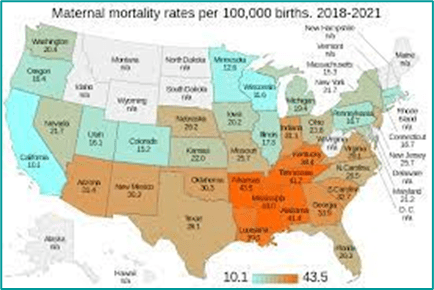
Breaking News: CDC reports largest infant mortality increase in more than two decades:

On November 1, the CDC released sobering new data that showed a 3% increase in infant mortality in 2022. This is critical as infant mortality has steadily decreased over the last several years and this data shows the largest year-to-year increase in more than 20 years. Maternal and infant health is fundamental to all health. Read our statement.
One of the leading factors in infant mortality is preterm birth. Now, more than ever, it’s critical that we do all we can towards ending preventable preterm birth. This November is the 20th anniversary of Prematurity Awareness Month. Please join us to raise awareness of the maternal and infant health crisis our country is facing.
The U.S. remains among the most dangerous developed nations for childbirth. Prematurity affects too many moms and babies and is fueled significantly by disparities in our healthcare system, communities, and institutions. Let’s all come together for action and advocacy.
How can you help? Make a difference by donating today and on November 17, World Prematurity Day, to help ensure that all moms, babies, and families get the best possible start.
Kelly Ernst SVP, Chief Revenue & Impact Officer – March of Dimes


Enrique Iglesias, Maria Becerra – ASI ES LA VIDA (Official Video)
Enrique Iglesias (SPAIN): 27,241,727 views Premiered Oct 5, 2023 #AsiEsLaVida #EnriqueIglesias #MariaBecerra
María Becerra (Argentina):María de los Ángeles Becerra (born 12 February 2000) is an Argentine singer and former YouTuber

Infant Mortality in the United States: Provisional Data From the 2022 Period Linked Birth/Infant Death File
Danielle M. Ely, Ph.D., and Anne K. Driscoll, Ph.D.
Abstract Objectives—This report presents provisional 2022 data on infant mortality rates using the U.S. linked birth/infant death files. Infant mortality rates are shown by infant age at death, maternal race and Hispanic origin and age, gestational age and sex of the newborn, state of residence of the mother, and 10 leading causes of infant death.
Methods—Data are from the period linked birth/infant death files, which link infant deaths with the corresponding birth certificates. Comparisons are made between provisional 2022 and final 2021 data. The linked birth/infant files are based on 100% of birth certificates and 98%–99% of infant death certificates registered in all states and the District of Columbia. For 2022, 1.4% of infant deaths remained unlinked. Infant deaths in states with less than 100% of infant death records linked to their respective birth records are weighted.
Results—The provisional infant mortality rate for the United States in 2022 was 5.60 infant deaths per 1,000 live births, 3% higher than the rate in 2021 (5.44). The neonatal mortality rate increased 3% from 3.49 to 3.58, and the postneonatal mortality rate by 4% (from 1.95 to 2.02) from 2021 to 2022. Mortality rates increased significantly among infants of American Indian and Alaska Native non-Hispanic (7.46 to 9.06) and White non-Hispanic (4.36 to4.52) women. From 2021 to 2022, infant mortality rates increased significantly for infants of women ages 25–29, from 5.15 to 5.37. Mortality rates increased significantly for total preterm (less than 37 weeks of gestation) and early preterm (less than 34 weeks of gestation) infants. The mortality rate increased significantly only for male infants from 2021 to 2022. Infant mortality rates increased in four states and declined in one state. Mortality rates increased for 2 of the 10 leading causes of death: maternal complications and bacterial sepsis.
Source:Vital Statistics Rapid Release, Number 33 (November 2023) (cdc.gov)

HEALTHCARE PARTNERS

Effects of Virtual Reality Simulation Program Regarding High-risk Neonatal Infection Control on Nursing Students
Author links open overlay panel Mi Yu 1, Miran Yang 2, Boram Ku 3, Jon S. Mann 4

Abstract
Purpose
Virtual reality simulation can give nursing students a safe clinical experience involving high-risk infants where access to neonatal intensive care units is limited. This study aimed to examine the effects of a virtual reality simulation program on Korean nursing students’ knowledge, performance self-efficacy and learner satisfaction.
Methods
A nonequivalent control group design was applied. Senior nursing students were divided into an experimental group (n = 25) experiencing virtual reality simulation and routine neonatal intensive care unit practice and a control group (n = 25) having routine neonatal intensive care unit practice. The program consisted of three scenarios: basic care, feeding management and skin care and environmental management for prevention of neonatal infection. The total execution time for the three scenarios was 40 minutes. The simulation created immersive virtual reality experiences using a head-mounted display with hand-tracking technology. Data were collected from December 9, 2019, to January 17, 2020, and were analyzed using descriptive statistics and the t-test, paired t-tests, Mann-Whitney test and Wilcoxon signed-ranks test.
Results
Compared to the control group, the experimental group showed significantly greater improvements in high-risk neonatal infection control performance self-efficacy (t = −2.16, p = .018) and learner satisfaction (t = −5.59, p < .001).
Conclusion
The virtual reality simulation program can expand the nursing students’ practice experience in safe virtual spaces and enhance their performance self-efficacy and learning satisfaction.

Female leadership in neonatology: The value of mentorship

Posted on March 21, 2023 by Nancy Fliesler | Our Community, People
Martha Sola-Visner, MD, and Patricia Davenport, MD, enjoy a strong mentoring relationship where benefits flow in both directions. (Photos: Michael Goderre, Boston Children’s Hospital)
While the majority of neonatologists are women, women make up a far smaller proportion of neonatologists in leadership positions. A recent national survey led by Kristen Leeman, MD, in the Division of Newborn Medicine at Boston Children’s and Lindsay Johnston, MD, at Yale, finds that many female neonatologists face roadblocks to career development. They often miss out on speaking engagements, career guidance, additional training, networking opportunities, and above all, mentors.
To learn more about their needs, Leeman and her colleagues contacted nearly 4,000 female neonatologists from the AAP-affiliated Women in Neonatology group and a Facebook group for female neonatologists. They received 451 survey responses, revealing several additional challenges:
• gender-based salary discrepancies, reported by 49 percent of respondents
• delayed promotion (37 percent)
• harassment by colleagues (31 percent), trainees (8 percent), staff (24 percent), and patient families (32 percent)
• lack of an established mentor (61 percent).
Female neonatologists also tend to struggle more than their male counterparts with work/life balance issues, Leeman notes, making it hard to advance. “Women commented on child care stress and burnout,” she says. “The supports are not there at vulnerable times in their careers. It’s a leaky pipeline.”
Building a mentoring program for female neonatologists
Leeman and Johnston decided to address what they see as the key missing ingredient — mentors.
“Both of us have had the benefit of superb mentorship, which has been integral to our careers,” says Leeman. “We wanted to offer an opportunity for all women across the U.S. to have access to female role models to help mentor them through different elements of their careers.”
With colleagues across the country, they created the National Women in Neonatology Mentorship Program. Bringing together senior, mid-career, and junior neonatologists, the year-long pilot program, which concludes in August, has three goals:
• to provide resources to facilitate career advancement and professional and personal satisfaction
• to identify strategies to help female neonatologists gain appropriate compensation, promotions, and professional recognition
• to foster a feeling of community.
In virtual and in-person meetings, the program’s 250-plus participants read and discuss materials, hear speakers, share their thoughts and experiences, network, offer mutual encouragement, and consult with mentors. The program has various subgroups, including groups for women practicing in community NICUs, groups for specific interests like global health or lab research, and groups for women from backgrounds that tend to be underrepresented in medicine.
Neonatology mentorship at Boston Children’s: Balancing medicine, research, and family
Patricia Davenport, MD, and Martha Sola-Visner, MD, neonatologists at Boston Children’s, illustrate the value of mentorship. As a junior faculty member, Davenport found herself juggling her clinical, research, and family responsibilities. In addition to caring for patients in the NICU, she joined Sola-Visner’s lab to conduct research on neonatal platelet transfusions. Sola-Visner quickly became a mentor.
“Martha’s mentorship has been crucial to me,” Davenport says. “She values her patients, her research, and her family. Holding those three things equally in your hands is really important. I had never done basic science before and needed a lot of mentoring, not just at the bench but also writing and presenting.”
Whether it’s an unfortunate patient outcome, an experiment that didn’t work, or a family emergency, Sola-Visner has been a vital support and sounding board. And the benefits of mentorship flow in both directions.
“I’m established now, and at this stage in my career, seeing other people progress and move forward is the most rewarding part of what I do,” says Sola-Visner. “Making sure that the people who I’ve mentored are succeeding becomes more and more important over time. I get great joy to see that.”
Davenport is also an enthusiastic participant in the national pilot mentorship program, where she is part of a subgroup on basic science.
“We talk about funding difficulties, how to organize a lab, wellness, how to care for yourself,” she says. “There’s a real sense of community across the nation. You’re always asking, ‘am I good enough?’ and it’s nice to hear other women having the same thoughts and feelings of ‘imposter syndrome.’ But we’re all doing good work.”
Source:https://answers.childrenshospital.org/mentorship-neonatology

PREEMIE FAMILY PARTNERS


Why This Pediatrician Loves NICU Babies: ‘They’re Some of the Toughest People I Know’ -American Academy of Pediatrics

What happens when you love the technical side of medicine and the emotional draw of babies in need? You become a neonatologist. Dr. Joanna Parga-Belinkie explains why the traumas and the triumphs of her tiny patients, many of them premature babies, make neonatology the “best job.” #wearepediatricians


Bilingual Boost: Preterm Children Thrive with Two Languages
October 29, 2023

Summary: Researchers discovered that bilingualism benefits children born prematurely, contradicting some health care professionals’ advice. The study found bilingual preterm children outperformed monolingual peers in cognitive tests.
Bilingualism could be an early intervention strategy to improve executive functions in preterm children. The research suggests bilingualism’s potential role in enhancing the developmental skills of preterm-born children.
Key Facts:
- Bilingual children born prematurely performed better in cognitive tests than monolingual peers, displaying skills crucial for academic success.
- Executive functions like attention, planning, and decision-making are often compromised in preterm children, leading to misconceptions about bilingualism causing delays.
- The study involved 17 preterm children (ages 6-7); results indicated bilingual children performed more accurately and made more switches in the Creature Counting task.
Source: Florida International University
Researchers from FIU have found that speaking more than one language can be beneficial for children born prematurely, counter to advice often given by health care professionals.
The study, published in Advances in Neonatal Care, compared two groups who were born preterm: bilingual children and children who only spoke one language. The bilingual group performed better on a cognitive test, showing better organization, accuracy and response time, compared to monolingual children—important skills for academic success.
“The conventional advice provided by health care professionals is not to speak more than one language with children born prematurely,” said Caroline Gillenson, lead author and doctoral student in FIU Center for Children and Families (CCF) Clinical Science Program.
“Our findings show that shouldn’t be the case and that bilingualism could be an early intervention strategy to help strengthen preterm-born children’s executive functioning.”
Children born prematurely are often at increased risk for poor executive functioning—cognitive processes that include paying attention, planning, memory, decision-making, carrying out a task, among others. Researchers say this is one of the reasons misconceptions arose that speaking more than one language can interfere with language acquisition or cause delays.
The researchers followed a small group of 17 children, between the ages of 6 and 7, born very preterm (before 35 weeks) with low birth weight and long hospital stays in the neonatal intensive care unit (NICU). There were eight monolingual children and nine children who spoke English and Spanish.
To test their executive function, researchers gave the children a Creature Counting task—a test that had them counting the number of animals from top to bottom, starting with one, and then switching between counting upward or downward, according to arrows.
The ability to switch from counting upward to downward or vice versa is key to measuring executive functioning. Correct responses and the time it took to complete the task were recorded.
Preterm-born bilingual children performed significantly more accurately and with more total switches than the preterm-born monolingual children.
The study’s authors point out that although they had a small sample size, their preliminary data has real-world implications and shines a light on the advantages bilingualism may give to preterm-born children’s executive functioning abilities.
“This really shows speaking more than one language can be tremendously helpful for preterm-born children just as it is for children born full term,” said FIU Psychology Professor and study author Daniel Bagner.
Next, the team hopes to also explore additional advantages that may arise when preterm-born children speak more than one language, including spatial reasoning (the understanding of how objects can move in a 3-dimensional world), and meta-linguistic awareness (the ability to consciously reflect on the nature of language and figure out rules and patterns).
“Unfortunately, many parents who have a child that was born prematurely have shared with us that their pediatric provider advised them to stop using their native language at home. They were told to use English only with their child,” said Melissa Baralt, FIU psycholinguistics professor and one of the study’s authors.
“We hope this research can serve as a call-to-action for parents and health care professionals to embrace the advantages of bilingualism in nurturing the developmental skills of preterm-born children.”
Tips for parents to promote bilingualism in their children
Melissa Baralt shared the following tips:
- Read with your baby every day. Public libraries have books in many different languages! Interact with the book and with your child.
- Learning can happen anywhere. You can turn everyday moments into learning opportunities for your baby by having conversations, asking questions, and narrating what you are doing together. These are the moments that matter.
- Get the entire family involved! Grandparents are linguistic experts, and talking on Facetime or WhatsApp video gives them a great opportunity to have interactive conversations.
- Try not to depend on television or tablets. Promoting bilingualism requires interactive conversations.
- Help children associate positive feelings with the language. Sing in Spanish or the language of your choice, play together and listen to music.
- Be enthusiastic when you speaking and have fun!
- Focus on what your child has achieved rather than perfection. Interactive conversations and the creative use of language is more important than correct grammar.
Summary: Researchers discovered that bilingualism benefits children born prematurely, contradicting some health care professionals’ advice. The study found bilingual preterm children outperformed monolingual peers in cognitive tests.
Bilingualism could be an early intervention strategy to improve executive functions in preterm children. The research suggests bilingualism’s potential role in enhancing the developmental skills of preterm-born children.
Key Facts:
Bilingual children born prematurely performed better in cognitive tests than monolingual peers, displaying skills crucial for academic success.
Executive functions like attention, planning, and decision-making are often compromised in preterm children, leading to misconceptions about bilingualism causing delays.
The study involved 17 preterm children (ages 6-7); results indicated bilingual children performed more accurately and made more switches in the Creature Counting task.
Researchers from FIU have found that speaking more than one language can be beneficial for children born prematurely, counter to advice often given by health care professionals.
The study, published in Advances in Neonatal Care, compared two groups who were born preterm: bilingual children and children who only spoke one language. The bilingual group performed better on a cognitive test, showing better organization, accuracy and response time, compared to monolingual children—important skills for academic success.
Preterm-born bilingual children performed significantly more accurately and with more total switches than the preterm-born monolingual children. Credit: Neuroscience News
“The conventional advice provided by health care professionals is not to speak more than one language with children born prematurely,” said Caroline Gillenson, lead author and doctoral student in FIU Center for Children and Families (CCF) Clinical Science Program.
“Our findings show that shouldn’t be the case and that bilingualism could be an early intervention strategy to help strengthen preterm-born children’s executive functioning.”
Children born prematurely are often at increased risk for poor executive functioning—cognitive processes that include paying attention, planning, memory, decision-making, carrying out a task, among others. Researchers say this is one of the reasons misconceptions arose that speaking more than one language can interfere with language acquisition or cause delays.
The researchers followed a small group of 17 children, between the ages of 6 and 7, born very preterm (before 35 weeks) with low birth weight and long hospital stays in the neonatal intensive care unit (NICU). There were eight monolingual children and nine children who spoke English and Spanish.
To test their executive function, researchers gave the children a Creature Counting task—a test that had them counting the number of animals from top to bottom, starting with one, and then switching between counting upward or downward, according to arrows.
The ability to switch from counting upward to downward or vice versa is key to measuring executive functioning. Correct responses and the time it took to complete the task were recorded.
Preterm-born bilingual children performed significantly more accurately and with more total switches than the preterm-born monolingual children.
The study’s authors point out that although they had a small sample size, their preliminary data has real-world implications and shines a light on the advantages bilingualism may give to preterm-born children’s executive functioning abilities.
“This really shows speaking more than one language can be tremendously helpful for preterm-born children just as it is for children born full term,” said FIU Psychology Professor and study author Daniel Bagner.
Next, the team hopes to also explore additional advantages that may arise when preterm-born children speak more than one language, including spatial reasoning (the understanding of how objects can move in a 3-dimensional world), and meta-linguistic awareness (the ability to consciously reflect on the nature of language and figure out rules and patterns).
“Unfortunately, many parents who have a child that was born prematurely have shared with us that their pediatric provider advised them to stop using their native language at home. They were told to use English only with their child,” said Melissa Baralt, FIU psycholinguistics professor and one of the study’s authors.
“We hope this research can serve as a call-to-action for parents and health care professionals to embrace the advantages of bilingualism in nurturing the developmental skills of preterm-born children.”
Tips for parents to promote bilingualism in their children
Melissa Baralt shared the following tips:
Read with your baby every day. Public libraries have books in many different languages! Interact with the book and with your child.
Learning can happen anywhere. You can turn everyday moments into learning opportunities for your baby by having conversations, asking questions, and narrating what you are doing together. These are the moments that matter.
Get the entire family involved! Grandparents are linguistic experts, and talking on Facetime or WhatsApp video gives them a great opportunity to have interactive conversations.
Try not to depend on television or tablets. Promoting bilingualism requires interactive conversations.
Help children associate positive feelings with the language. Sing in Spanish or the language of your choice, play together and listen to music.
Be enthusiastic when you speaking and have fun!
Focus on what your child has achieved rather than perfection. Interactive conversations and the creative use of language is more important than correct grammar.
About this neurodevelopment research news – Author: Caroline J. Gillenson -Source: Florida International University
Contact: Caroline J. Gillenson – Florida International University
Original Research: Closed access. “A Preliminary Study of Executive Functioning in Preterm-Born Children” by Caroline J. Gillenson et al. Advances in Neonatal Care

Bilingual Boost: Preterm Children Thrive with Two Languages
October 29, 2023

Summary: Researchers discovered that bilingualism benefits children born prematurely, contradicting some health care professionals’ advice. The study found bilingual preterm children outperformed monolingual peers in cognitive tests.
Bilingualism could be an early intervention strategy to improve executive functions in preterm children. The research suggests bilingualism’s potential role in enhancing the developmental skills of preterm-born children.
Key Facts:
- Bilingual children born prematurely performed better in cognitive tests than monolingual peers, displaying skills crucial for academic success.
- Executive functions like attention, planning, and decision-making are often compromised in preterm children, leading to misconceptions about bilingualism causing delays.
- The study involved 17 preterm children (ages 6-7); results indicated bilingual children performed more accurately and made more switches in the Creature Counting task.
Source: Florida International University
Researchers from FIU have found that speaking more than one language can be beneficial for children born prematurely, counter to advice often given by health care professionals.
The study, published in Advances in Neonatal Care, compared two groups who were born preterm: bilingual children and children who only spoke one language. The bilingual group performed better on a cognitive test, showing better organization, accuracy and response time, compared to monolingual children—important skills for academic success.
“The conventional advice provided by health care professionals is not to speak more than one language with children born prematurely,” said Caroline Gillenson, lead author and doctoral student in FIU Center for Children and Families (CCF) Clinical Science Program.
“Our findings show that shouldn’t be the case and that bilingualism could be an early intervention strategy to help strengthen preterm-born children’s executive functioning.”
Children born prematurely are often at increased risk for poor executive functioning—cognitive processes that include paying attention, planning, memory, decision-making, carrying out a task, among others. Researchers say this is one of the reasons misconceptions arose that speaking more than one language can interfere with language acquisition or cause delays.
The researchers followed a small group of 17 children, between the ages of 6 and 7, born very preterm (before 35 weeks) with low birth weight and long hospital stays in the neonatal intensive care unit (NICU). There were eight monolingual children and nine children who spoke English and Spanish.
To test their executive function, researchers gave the children a Creature Counting task—a test that had them counting the number of animals from top to bottom, starting with one, and then switching between counting upward or downward, according to arrows.
The ability to switch from counting upward to downward or vice versa is key to measuring executive functioning. Correct responses and the time it took to complete the task were recorded.
Preterm-born bilingual children performed significantly more accurately and with more total switches than the preterm-born monolingual children.
The study’s authors point out that although they had a small sample size, their preliminary data has real-world implications and shines a light on the advantages bilingualism may give to preterm-born children’s executive functioning abilities.
“This really shows speaking more than one language can be tremendously helpful for preterm-born children just as it is for children born full term,” said FIU Psychology Professor and study author Daniel Bagner.
Next, the team hopes to also explore additional advantages that may arise when preterm-born children speak more than one language, including spatial reasoning (the understanding of how objects can move in a 3-dimensional world), and meta-linguistic awareness (the ability to consciously reflect on the nature of language and figure out rules and patterns).
“Unfortunately, many parents who have a child that was born prematurely have shared with us that their pediatric provider advised them to stop using their native language at home. They were told to use English only with their child,” said Melissa Baralt, FIU psycholinguistics professor and one of the study’s authors.
“We hope this research can serve as a call-to-action for parents and health care professionals to embrace the advantages of bilingualism in nurturing the developmental skills of preterm-born children.”
Tips for parents to promote bilingualism in their children
Melissa Baralt shared the following tips:
- Read with your baby every day. Public libraries have books in many different languages! Interact with the book and with your child.
- Learning can happen anywhere. You can turn everyday moments into learning opportunities for your baby by having conversations, asking questions, and narrating what you are doing together. These are the moments that matter.
- Get the entire family involved! Grandparents are linguistic experts, and talking on Facetime or WhatsApp video gives them a great opportunity to have interactive conversations.
- Try not to depend on television or tablets. Promoting bilingualism requires interactive conversations.
- Help children associate positive feelings with the language. Sing in Spanish or the language of your choice, play together and listen to music.
- Be enthusiastic when you speaking and have fun!
- Focus on what your child has achieved rather than perfection. Interactive conversations and the creative use of language is more important than correct grammar.
Summary: Researchers discovered that bilingualism benefits children born prematurely, contradicting some health care professionals’ advice. The study found bilingual preterm children outperformed monolingual peers in cognitive tests.
Bilingualism could be an early intervention strategy to improve executive functions in preterm children. The research suggests bilingualism’s potential role in enhancing the developmental skills of preterm-born children.
Key Facts:
Bilingual children born prematurely performed better in cognitive tests than monolingual peers, displaying skills crucial for academic success.
Executive functions like attention, planning, and decision-making are often compromised in preterm children, leading to misconceptions about bilingualism causing delays.
The study involved 17 preterm children (ages 6-7); results indicated bilingual children performed more accurately and made more switches in the Creature Counting task.
Researchers from FIU have found that speaking more than one language can be beneficial for children born prematurely, counter to advice often given by health care professionals.
The study, published in Advances in Neonatal Care, compared two groups who were born preterm: bilingual children and children who only spoke one language. The bilingual group performed better on a cognitive test, showing better organization, accuracy and response time, compared to monolingual children—important skills for academic success.
Preterm-born bilingual children performed significantly more accurately and with more total switches than the preterm-born monolingual children. Credit: Neuroscience News
“The conventional advice provided by health care professionals is not to speak more than one language with children born prematurely,” said Caroline Gillenson, lead author and doctoral student in FIU Center for Children and Families (CCF) Clinical Science Program.
“Our findings show that shouldn’t be the case and that bilingualism could be an early intervention strategy to help strengthen preterm-born children’s executive functioning.”
Children born prematurely are often at increased risk for poor executive functioning—cognitive processes that include paying attention, planning, memory, decision-making, carrying out a task, among others. Researchers say this is one of the reasons misconceptions arose that speaking more than one language can interfere with language acquisition or cause delays.
The researchers followed a small group of 17 children, between the ages of 6 and 7, born very preterm (before 35 weeks) with low birth weight and long hospital stays in the neonatal intensive care unit (NICU). There were eight monolingual children and nine children who spoke English and Spanish.
To test their executive function, researchers gave the children a Creature Counting task—a test that had them counting the number of animals from top to bottom, starting with one, and then switching between counting upward or downward, according to arrows.
The ability to switch from counting upward to downward or vice versa is key to measuring executive functioning. Correct responses and the time it took to complete the task were recorded.
Preterm-born bilingual children performed significantly more accurately and with more total switches than the preterm-born monolingual children.
The study’s authors point out that although they had a small sample size, their preliminary data has real-world implications and shines a light on the advantages bilingualism may give to preterm-born children’s executive functioning abilities.
“This really shows speaking more than one language can be tremendously helpful for preterm-born children just as it is for children born full term,” said FIU Psychology Professor and study author Daniel Bagner.
Next, the team hopes to also explore additional advantages that may arise when preterm-born children speak more than one language, including spatial reasoning (the understanding of how objects can move in a 3-dimensional world), and meta-linguistic awareness (the ability to consciously reflect on the nature of language and figure out rules and patterns).
“Unfortunately, many parents who have a child that was born prematurely have shared with us that their pediatric provider advised them to stop using their native language at home. They were told to use English only with their child,” said Melissa Baralt, FIU psycholinguistics professor and one of the study’s authors.
“We hope this research can serve as a call-to-action for parents and health care professionals to embrace the advantages of bilingualism in nurturing the developmental skills of preterm-born children.”
Tips for parents to promote bilingualism in their children
Melissa Baralt shared the following tips:
Read with your baby every day. Public libraries have books in many different languages! Interact with the book and with your child.
Learning can happen anywhere. You can turn everyday moments into learning opportunities for your baby by having conversations, asking questions, and narrating what you are doing together. These are the moments that matter.
Get the entire family involved! Grandparents are linguistic experts, and talking on Facetime or WhatsApp video gives them a great opportunity to have interactive conversations.
Try not to depend on television or tablets. Promoting bilingualism requires interactive conversations.
Help children associate positive feelings with the language. Sing in Spanish or the language of your choice, play together and listen to music.
Be enthusiastic when you speaking and have fun! Focus on what your child has achieved rather than perfection. Interactive conversations and the creative use of language is more important than correct grammar.
About this neurodevelopment research news – Author: Caroline J. Gillenson -Source: Florida International University
Contact: Caroline J. Gillenson – Florida International University
Original Research: Closed access. “A Preliminary Study of Executive Functioning in Preterm-Born Children” by Caroline J. Gillenson et al. Advances in Neonatal Care
Source: https://neurosciencenews.com/bilingual-neurodevelopment-25120/


Episode Highlight: Most Premature Babies PSP Survey

Are you a NICU Parent or Adult born premature? Have your say! The Most Premature Babies Priority Setting Partnership (PSP) Survey wants you to help choose the 10 questions that matter the most to you helping to determine the top 10 research priorities for extremely premature babies. The results will be shared with the international research community and funding bodies, to help researchers design and conduct studies and act as a guide for funding bodies and research institutions to determine where resources should be prioritised.
INNOVATIONS
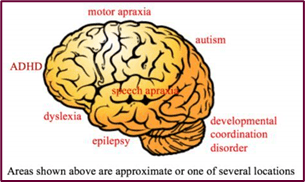
Neurodevelopmental Outcomes in Preterm Babies: A 12-Month Observational Study
Shresth Jain • Putun Patel • Nimisha Pandya • Dhruva Dave • Trupti Deshpande
Published: October 27, 2023
ABSTRACT
Background
Preterm births are a significant concern worldwide due to their association with both short- and long-term morbidity. Modern neonatal intensive care techniques have improved the survival of infants born at the brink of viability. However, there remain significant challenges concerning their neurodevelopment. A considerable proportion of very low birth weight infants exhibit significant motor deficits such as cerebral palsy or cognitive, behavioral, or attention disabilities. The consequences of these impairments, particularly given their life-long nature, can be severe for the affected individuals, families, and public health resources. Consequently, timely neurodevelopmental assessment is critical in recognizing delayed development and selecting infants for neurodevelopmental stimulation. This study aimed to estimate the neurodevelopment of preterm infants, identify influencing factors, detect at-risk groups, and refer/recommend early intervention when developmental delays are observed.
Methodology
This prospective, observational, hospital-based study done in the department of pediatrics, Gujarat Medical Education and Research Society (GMERS) Medical College and Hospital, Gotri, Vadodara, Gujrat, India included inborn and outborn preterm neonates admitted to the Neonatal Intensive Care Unit (NICU) or the Sick Newborn Care Unit from their first day of life. The study period was from October 2020 to January 2021, and only neonates with an uncomplicated clinical course were included. Newborns were enrolled in a high-risk clinic, and follow-up appointments were scheduled at three, six, nine, and 12 months of corrected gestational age (CGA). We used the Baroda Developmental Screening Tool (BDST) to calculate the developmental quotient (DQ) at each appointment. This assessment involved parental interviews, observation of developmental milestones, and simple test demonstrations. The gathered DQ data at different ages were analyzed and compared across groups.
Results
Of 100 preterms enrolled, 62 preterms were followed up until 12 months of CGA. Thirteen patients out of the 62 (approximately one-fifth) preterm neonates exhibited developmental delays at one year of CGA, most of whom were early preterm infants. Twenty-six patients (approximately two-fifths) were delayed at three months of CGA, and thus 13 patients (half) showed catch-up growth and development. There was no statistically significant difference between the neurodevelopment of female and male infants. However, infants born to mothers with better socioeconomic status and higher education showed improved neurodevelopment.
Conclusions
Our study findings suggest that preterm infants discharged from the NICU exhibit poor neurodevelopmental outcomes, especially those born early preterm. This pattern indicates an inverse relationship between neurodevelopmental delay and the maturity of the neonate. Maternal education and socioeconomic status positively impacted the neurodevelopment of preterm NICU graduates. Thus, regular follow-up (at least once every three months), early detection by a screening scale like the BDST and intervention significantly improved neurodevelopmental outcomes.

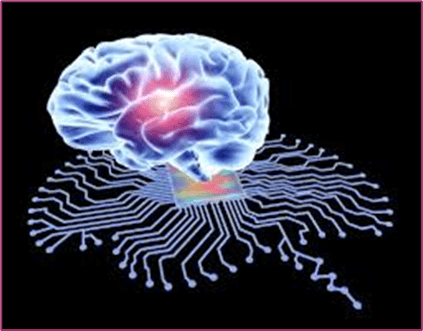
ChatGPT outperforms doctors in following clinical guidelines for depression treatment
Reviewed by Megan Craig, M.Sc. Oct. 16, 2023

ChatGPT, the AI language model capable of mirroring human conversation, may be better than a doctor at following recognized treatment standards for clinical depression, and without any of the gender or social class biases sometimes seen in the primary care doctor-patient relationship, finds research published in the open access journal Family Medicine and Community Health.
However, further research is needed into how well this technology might manage severe cases as well as potential risks and ethical issues arising from its use, say the researchers.
Depression is very common, and many of those affected turn first to their family (primary care) doctors for help. The recommended course of treatment should largely be guided by evidence-based clinical guidelines, which usually suggest a tiered approach to care, in line with the severity of the depression.
ChatGPT has the potential to offer fast, objective, data-derived insights that can supplement traditional diagnostic methods as well as providing confidentiality and anonymity, say the researchers.
They therefore wanted to find out how the technology evaluated the recommended therapeutic approach for mild and severe major depression and whether this was influenced by gender or social class biases, when compared with 1249 French primary care doctors (73% women).
They drew on carefully designed and previously validated vignettes, centering around patients with symptoms of sadness, sleep problems, and loss of appetite during the preceding 3 weeks and a diagnosis of mild to moderate depression.
Eight versions of these vignettes were developed with different variations of patient characteristics, such as gender, social class, and depression severity. Each vignette was repeated 10 times for ChatGPT versions 3.5 and 4.
For each of the 8 vignettes, ChatGPT was asked: ‘What do you think a primary care physician should suggest in this situation?’ The possible responses were: watchful waiting; referral for psychotherapy; prescribed drugs (for depression/anxiety/sleep problems); referral for psychotherapy plus prescribed drugs; none of these.
Only just over 4% of family doctors exclusively recommended referral for psychotherapy for mild cases in line with clinical guidance, compared with ChatGPT-3.5 and ChatGPT-4, which selected this option in 95% and 97.5% of cases, respectively.
Most of the medical practitioners proposed either drug treatment exclusively (48%) or psychotherapy plus prescribed drugs (32.5%).
In severe cases, most of the doctors recommended psychotherapy plus prescribed drugs (44.5%). ChatGPT proposed this more frequently than the doctors (72% ChatGPT 3.5; 100% ChatGPT 4 in line with clinical guidelines). Four out of 10 of the doctors proposed prescribed drugs exclusively, which neither ChatGPT version recommended.
When medication was recommended, the AI and human participants were asked to specify which types of drugs they would prescribe.
The doctors recommended a combination of antidepressants and anti-anxiety drugs and sleeping pills in 67.5% of cases, exclusive use of antidepressants in 18%, and exclusive use of anti-anxiety and sleeping pills in 14%.
ChatGPT was more likely than the doctors to recommend antidepressants exclusively: 74%, version 3.5; and 68%, version 4. ChatGPT-3.5 (26%) and ChatGPT-4 (32%) also suggested using a combination of antidepressants and anti-anxiety drugs and sleeping pills more frequently than did the doctors.
But unlike the findings of previously published research, ChatGPT didn’t exhibit any gender or social class biases in its recommended treatment.
The researchers acknowledge that the study was limited to iterations of ChatGPT-3 and ChatGPT-4 at specific points in time and that the ChatGPT data were compared with data from a representative sample of primary care doctors from France, so might not be more widely applicable.
Lastly, the cases described in the vignettes were for an initial visit due to a complaint of depression, so didn’t represent ongoing treatment of the disease or other variables that the doctor would know about the patient.
“ChatGPT-4 demonstrated greater precision in adjusting treatment to comply with clinical guidelines. Furthermore, no discernible biases related to gender and [socioeconomic status] were detected in the ChatGPT systems,” highlight the researchers.
But there are ethical issues to consider, particularly around ensuring data privacy and security which are supremely important, considering the sensitive nature of mental health data, they point out, adding that AI shouldn’t ever be a substitute for human clinical judgement in the diagnosis or treatment of depression.
Nevertheless, they conclude: “The study suggests that ChatGPT…. has the potential to enhance decision making in primary healthcare.”
“However, it underlines the need for ongoing research to verify the dependability of its suggestions. Implementing such AI systems could bolster the quality and impartiality of mental health services.”

AI Will—and Should—Change Medical School, Says Harvard’s Dean for Medical Education
Yulin Hswen, ScD, MPH; Jennifer Abbasi JAMA. Published online October 25, 2023. doi:10.1001/jama.2023.19295

This conversation is part of a series of interviews in which JAMA Editor in Chief Kirsten Bibbins-Domingo, PhD, MD, MAS, and expert guests explore issues surrounding the rapidly evolving intersection of artificial intelligence (AI) and medicine.
How is generative AI catalyzing a paradigm shift in medical education? What will it mean for AI to assist in medical school applications or clinical teaching? And can AI be harnessed to elevate the skills and acumen of clinicians while also allowing them to connect more deeply with their humanity in encounters with patients?
Needless to say, when it comes to med school, it’s a brave new world.
It’s the world Bernard S. Chang, MD, MMSc (Video), has been steeped in since being named dean for medical education at Harvard Medical School this summer. JAMA Editor in Chief Kirsten Bibbins Domingo, PhD, MD, MAS, recently spoke with Chang, who is the Daniel D. Federman, MD, professor of neurology at Harvard and a practicing neurologist at Beth Israel Deaconess Medical Center in Boston.
Dr Bibbins-Domingo: Well, it is an interesting time for medical schools. You recently wrote an editorial that accompanied what JAMA publishes every year about the demographics of the students in medical schools in the US. Your editorial focused on how AI is going to transform medical education.
Dr Chang: I think this is about to be a major inflection point in medical education akin to what we experienced when the internet and internet search engines became available. The internet was around when I was in medical school in the mid-1990s, but it wasn’t really a source of medical information. Certainly as students, we didn’t go to the internet to help in our courses or help to learn material. But when search engines became available, it became clear that access to knowledge was so much easier and cheaper and simpler than it had been before. And what many medical schools around that time did was evolve their curriculum from one that emphasized lectures, which of course are very efficient ways of transferring facts and knowledge, to small group discussion formats which are more beneficial toward knowledge integration and knowledge analysis and interpretation and help students with oral presentation skills.
Dr Bibbins-Domingo: So it’s not as much that we have to memorize everything and just have all of that knowledge transferred to us. It’s more that medical education is focused on the higher-order skills of integrating that knowledge to try to make a clinical decision.
Dr Chang: Exactly. And I think coming up in these next few years, we’re going to have a similar transformation, which is that what generative artificial intelligence, these AI tools like ChatGPT, can do very effectively is summarize and even analyze and even make probabilistic decisions for us using data that we provide to it.
And so like what happened years ago, I think in undergraduate medical education we need to similarly evolve our curricula to reflect this new era. Our students of course still need to learn the fundamentals of how to be a doctor. That will never change. But we can more quickly move our students toward doing even higher levels of cognitive analysis, higher levels of understanding the individual patient nuance, which I think might still be difficult for AI to handle. Higher levels of compassionate and culturally competent communication, which we know AI might have some difficulty with. And returning students to the primacy of the physical exam, which as far as I know chatbots are not going to be replacing in the next few years.
So in other words, what I point out in my Viewpoint is that we need our students to be even more human in their doctoring skills than ever before, working at the highest levels of cognitive analysis, [engaging in] the most personally nuanced forms of communication, and remembering the importance of the actual laying on of hands.
Dr Bibbins-Domingo: Let’s take those 3 elements together. We already know that things like ChatGPT take tests pretty well, but you are challenging us that the medical student then of the future will need to not just be building this font of knowledge but be even better at integrating and figuring out how to synthesize that knowledge for the types of clinical decisions that are being made. So they might rely on ChatGPT for a first order, but they have to be even better using their human skills at figuring out how to integrate that for the patient. ChatGPT communicates, it seems to be very good at being empathetic, but you’re challenging us to be more human in our communication skills that we are teaching medical students. And then the physical exam, which presumably these gen [generative] AI tools are not going to ever be able to do.
Dr Chang: Right. So as an example, we know that ChatGPT when given a set of signs and symptoms can produce a fairly good differential diagnosis. And that’s something that we still need to teach our students, but maybe more quickly than before we can move our students to a level at which they’re working with that differential diagnosis to make it individualized to their particular patient. To take into account some of the particular nuances and specifics of their patient’s history or their patient’s lived experience that ChatGPT really can’t take into account. And that’s where their role as medical students and future doctors can be most useful.
We want to train our students to be the physicians of the future who are going to be AI-enabled physicians. Artificial intelligence is not going to replace physicians, right? But physicians who use artificial intelligence are really going to be working at the top of their game in clinical medicine. So we want to train our medical students to be those physicians, to be the physicians who in a clinical visit can really focus on that interpersonal interaction to really get to know their patients as human beings, to be that compassionate provider, and to do the most incisive levels of clinical decision-making while AI is presumably running in the background and doing some of the lower-level tasks that otherwise would’ve occupied those physicians in the past.
So it’s not that we don’t need to start from the basics. Of course medical students need to start from the basics, but I believe they can move more quickly from the basics to more advanced levels of reasoning and communication, knowing that they’ll be supported by AI in the future to do the fundamentals of decision analysis and communication.
Dr Bibbins-Domingo: What I like about your piece so much is that it seems like this natural evolution. We used to never think we would have calculators at exams or we would never have these other types of catalogs of medical knowledge as a part of our exams. And now we routinely accept them because we want our clinicians to be functioning at much higher levels. So it resonates so much for me what you’ve written. Now, how do we do that? How are you going to do that at Harvard Medical School?
Dr Chang: Our students learn to take a history, they learn to perform a physical exam, and then they learn to write a proper clinical note. And then we ask them to do it over and over and over again to basically instill that into their minds and show us with confidence that they can automatically generate solid clinical notes that are interpretable by other providers. Well, we know that ChatGPT writes pretty good clinical notes if given the right inputs. So I’d love for our students to learn the basics of history and physical exam and writing clinical notes. But instead of spending as much time as we do now writing notes over and over and over again, we can move our students to higher levels of analysis and interpretation earlier in their medical education.
Dr Bibbins-Domingo: So you’re not talking about replacing the building blocks. You’re talking about moving more quickly through those to get to the point that we’re actually focused on still, the big gap between what we learn in medical education and what we need as a practicing physician. How do we do that? Where do you see the changes? Are they going to be in the first few years of medical education? Are they going to be in the later years? I recognize you’re a new dean, but do you have a sense of what type of things will look different as we go into the future?
Dr Chang: Honestly, I think every phase of medical education is going to look different and every phase of undergraduate medical education, from preclerkship curriculum to the clinical clerkships to the postclerkship phase. I think everything is going to look different. In the preclerkship curriculum, for example, in the basic science and social science courses, AI is going to be present as an educational tool. It’s already happening. The entering class of first-year students, many of them were college seniors when ChatGPT became available last academic year, and they are now going to be using ChatGPT, GPT-4, and other tools like that to help them learn, to help them preview the material in our flipped classroom environment, to help them consolidate the knowledge afterward, and to study the content for exams.
So that’s already present. They’re using it as an educational tool. They can use it to serve as a self-tutor because you can ask ChatGPT to serve as a tutor, to test you with certain questions, and to alter the level of difficulty of the questions based on your responses. So already that’s right from the beginning of medical school.
In our clinical skills course where we’re preparing our students to be able to have the fundamental building blocks to go onto the clerkships, again, I think we’re going to be able to use the fact that ChatGPT is available to move our students to those higher-level clinical skills earlier on. And then I think after the clerkships, as students are exploring subinternships and electives and thinking about applying to residencies, of course this is going to be 2 or 3 years from now for our entering students, and we will have 2 or 3 years of generative AI under our belts. I think it’s going to play a very large role in our students’ experience as they, as subinterns, actually lead the care of their own inpatients on teams.
We’re already seeing that among our house officers, who after all are some of the primary teachers of our students, among our residents and fellows ChatGPT is being used to help refine a differential diagnosis to make sure that nothing is missed, to help with some of the difficult or rare conditions that we know that AI can be very helpful for and that sometimes humans have cognitive biases against. And so as our students see this being used by residents and fellows and attendings on the wards, that’s going to be part of their education because AI is going to be part of the future of clinical medicine. And just like any aspect of clinical medicine, as medical school leaders, we need to adapt what we’re teaching and how we’re teaching to prepare our students for clinical medicine in the future.
Dr Bibbins-Domingo: When these types of generative AI tools first came into prominence or awareness, educators, whatever level of education they were involved with, had to scramble because their students were using them. They were figuring out how to put up the right types of guardrails, set the right types of rules. Are there rules or danger zones right now that you’re thinking about?
Dr Chang: Absolutely, and I think there’s quite a number of these. This is a focus that we’re embarking on right now because as exciting as the future is and as much potential as these generative AI tools have, there are also dangers and there are also concerns that we have to address.
One of them is helping our students, who like all of us are still new to this within the past year, understand the limitations of these tools. Now these tools are going to get better year after year after year, but right now they are still prone to hallucinations, or basically making up facts that aren’t really true and yet saying them with confidence. Our students need to recognize why it is that these tools might come up with those hallucinations to try to learn how to recognize them and to basically be on guard for the fact that just because ChatGPT is giving you a very confident answer, it doesn’t mean it’s the right answer. And in medicine of course, that’s very, very important. And so that’s one—just the accuracy and the validity of the content that comes out.
As I wrote about in my Viewpoint, the way that these tools work is basically a very fancy form of autocomplete, right? It is essentially using a probabilistic prediction of what the next word is going to be. And so there’s no separate validity or confirmation of the factual material, and that’s something that we need to make sure that our students understand.
The other thing is to address the fact that these tools may inherently be structurally biased. Now, why would that be? Well, as we know, ChatGPT and these other large language models [LLMs] are trained on the world’s internet, so to speak, right? They’re trained on the noncopyrighted corpus of material that’s out there on the web. And to the extent that that corpus of material was generated by human beings who in their postings and their writings exhibit bias in one way or the other, whether intentionally or not, that’s the corpus on which these LLMs are trained. So it only makes sense that when we use these tools, these tools are going to potentially exhibit evidence of bias. And so we need our students to be very aware of that. As we have worked to reduce the effects of systematic bias in our curriculum and in our clinical sphere, we need to recognize that as we introduce this new tool, this will be another potential source of bias.
You alluded to the fact that we need to help our students understand what the right use of these tools is. Is it okay to use these tools to write an assignment? Is it okay to use these tools to help yourself study? Is it okay to use these tools to draft that clinical note, that writeup on the patient that you just saw in your doctoring course? Well, we need to establish a set of educational policies and so forth to make sure that our students are still learning the basics and are using these tools as aids to their education and aids to their work.
You used the calculator analogy before. A student who started with a calculator right at the beginning might not ever learn basic arithmetic, but once you’ve learned basic arithmetic, we want you to be able to go on to learn more advanced forms of mathematics by using a calculator to help you take care of the basic arithmetic more quickly and without as many errors. And that’s what we need to tell our students about for ChatGPT.
Dr Bibbins-Domingo: I like that. It does strike me that even language models that are not trained on all the world’s information on the internet but are just trained on health care data, the challenge is that it risks learning the patterns of bias and not optimal care that we in medicine have delivered for our patients.
One of the things that I’ve loved being part of an educational institution, and I’m sure I suspect the same is for you, is teaching the next generation of clinicians to imagine the world different than what we have currently created. It’s good, but we also want it to be better. And that’s part of the ambition, I think, for medical schools. And so it feels like that’s another thing—placing these tools in context as one of the tools but not something that substitutes from imagining the world differently than what currently exists.
Dr Chang: Absolutely. It seems a little bit counterintuitive to be talking about how we may be able to strengthen and return to more of that humanistic patient-physician encounter in the face of a computational revolution here. But I really believe it. I’d love to see in the future our medical students and future physicians be able to spend more time at the bedside, more time looking at the patient, and less time typing over on the keyboard. More time concentrating on the individual nuanced communication and making sure that everything is being understood and less time worrying about whether this or the other fact is going to be recalled.
And I’m imagining that after a clinical encounter, which is going to be more face-to-face time and more effective in compassionate communication, then the physician will be able to turn to the screen aided by AI and have a note drafted, have a differential diagnosis listed, have laboratory results from the online medical record that might be relevant to the conversation pulled up, maybe have letters to consultants already drafted—things that might’ve otherwise taken the physician quite a lot of time to search for in the past. And knowing that that is running in the background should give me as the physician more opportunity and more leeway to spend time talking with my patient the way I really ought to have been all along.
Dr Bibbins-Domingo: So as applicants to medical school become more AI savvy, what will be the impact either on the process of going to medical school or the class that you’ve admitted?
Dr Chang: This is a question that is at the top of our minds because one of the things that I think AI can help us with is distinguishing the content with which we are judging our applicants from the fluency and readability of their language.
And I think it’s very difficult for us to separate those two things. When a personal statement reads very well and sounds very good, we are naturally inclined to think, wow, this is somebody who expresses themselves very well and we’re naturally inclined to think that the content of what they’ve said, the substance of what they’ve said, is very valuable. And while that may be true in certain circumstances, I think it does inherently carry some bias against those for whom English was not a native language or their first language and against those for whom other forms of expression are more natural to them.
I think AI will level the playing field there, and it will force us to look more closely at the substance of what people are writing, the nature of their experiences, why they actually want to become physicians, what their visions for a career in medicine are, and not just simply the surface readability or fluency of their language, because ChatGPT can make everybody sound fluent in that way.
Dr Bibbins-Domingo: I certainly agree with you. As in our business in the editorial and publishing world, being able to have publishing be more accessible to a range of authors because they can give us a manuscript that sounds or reads much more like what we’re used to reading—that certainly resonates for me. But aren’t you worried we’re going to get the empathy from ChatGPT and confuse it with whether that person who’s applying is really that wonderful, empathetic human being who might make a good doctor?
Dr Chang: It’s a great question, and I think that’s something that we’re going to struggle with. ChatGPT generates what I would call generically empathic statements. It’s very good at doing that, but we don’t want generically empathic doctors. We want medical students who are going to take their own experiences and learn from their patients who have their own lived experiences and generate authentic conversations and authentic communication to help with that patient’s health. And I think that’s going to be the job of our admissions committees, which is to look beyond the generically empathic statements to see the substance behind what our students, our applicants, are offering and the substance behind their internal drive to come to the field of medicine.
Dr Bibbins-Domingo: I have one more question for you. We have all of these wonderful applicants and entering students who have lived in this AI world and then they’re still being taught by the faculty. How are you going to train us faculty members to be the faculty of the future?
Dr Chang: This is a great point, and this is a major challenge for us, but it’s also a great opportunity. Our faculty are excited to learn. They need to learn. They are not naive to this. They need to learn, but they want to learn because they see the potential for what this can mean for the education of our students.
First of all, they see, frankly, the potential that this can make their work a little bit quicker and a little bit easier in terms of generating new content, generating assessment questions, finding ways to instruct the students, and also to test the students on their knowledge. So in some ways, this is a tool that will make our faculty’s job easier, but what we need to do in medical school is work on faculty development. And we’re going to spend a lot of this next year doing that.
Right now anyway, there’s no better way to learn how these tools work than to try them. And that’s been our mantra to our faculty, which is just try it, try it, try it. Using your current course materials, try it with what you’re doing on the clerkships right now, or what you’re doing in the subinternships right now, and don’t just rely on the first response. And so we’ve had a couple of different messages for our faculty.
Number one is that “generative” is the key word in generative AI. This is not just a fancy Google search. Don’t use it just to try to find some more obscure fact than you were going to find on Google. This generates content for you. It writes human-sounding text for you. So it plays its most important role at times when you need to generate, when you need to write, when you need to create text content for the page. And that’s one thing we’re telling our faculty.
Another thing we’re telling our faculty is the importance of what’s now known as prompt engineering, which is knowing what questions to ask. It’s funny because that’s an old-fashioned thing we tell our students on the wards, right? That when students say, “That patient was a poor historian,” perhaps, in fact, it’s because you didn’t ask the right questions. And it’s the same thing with these generative AI tools. The quality of the prompt that you give it is proportional to the quality of the response that you’re going to get. And so we have to become better at generating specific prompts that we know are going to elicit the kinds of responses that we need that are going to be most helpful.
And I always tell our faculty, don’t just stop with the first response. The first answer that you get back is just a first draft, and you would never accept a first draft as your final version. So if there’s something that you don’t like about what came back, if there was an error, or if it was not quite what you were looking for, the beauty of ChatGPT is that you can converse. You can say, “Actually, that’s not quite what I was looking for. I was expecting X and Y and please don’t do Z again.” And then it’ll come back with another response. And in my experience, after just 2 or 3 iterations, you have something that’s much closer to what you intended than maybe the first try. So these are some of the simple mantras that we’ve been spreading to our faculty as they’re learning, and we’re all learning how to use these tools in our educational program.


We are thrilled to come together once again to celebrate the annual Neonatal Womb Warriors Blog; a testament to the strength and resilience of premature babies, preemie survivors, families, providers, and all community members alike. Every year holds a particularly special place in our hearts. We’ve had the privilege of shining a spotlight on 12 additional Nations from around the world, each presenting their unique neonatal community.
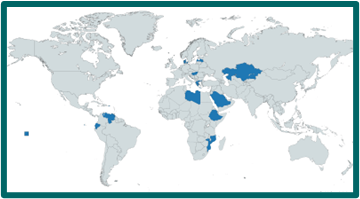
Please enjoy our annual Instagram posts @katkcampos, displayed in the photo below, where we highlight the remarkable 12 nations featured this year. Our fashionable posts feature music from each nation (listed below) and come with a delightful surprise (see Greece!). We are excited to share a mouthwatering assortment of our personal favorite home-baked goods, along with secret baking tips for added fun! These delectable treats are more than just a sweet indulgence; they symbolize the sweetness of the victories achieved by our Neonatal Womb Warriors/Preterm Birth Community and the love that binds our Global community together.
However, the fun doesn’t stop there; this year’s special gift is the sharing of our cherished original Red Velvet cake recipe. Just as the ingredients in this recipe blend harmoniously to create something beautiful, our Neonatal Womb Warriors community continues to strengthen through collaboration, research and innovation, the shared stories, love, and compassion that connect us all.
We extend our heartfelt thanks to each and every one of you for being an essential part of this incredible journey!

Moving from the top left to the right are hyperlinked songs for each Instagram post featuring an artist from each of the 12 nations we’ve highlighted this past year.
- Greece: Πέτρος Ιακωβίδης – Αχ Καρδούλα μου
- Ecuador: Alex Ponce – La Ultima Noche
- Latvia: Samanta Tīna – ATDEVU VISU TEV
- Saudi Arabia: Aseel Omran-Motouni أسيل عمران … موتوني
- Ethiopia: Master KG – Jerusalema [Feat. Nomcebo]
- Hungary: VALMAR ft. Szikora Robi – Úristen
- Venezuela: Chino y Nacho – Me Voy Enamorando
- Kazakhstan: Димаш 迪马什 Dimash
- Mozambique: Anderson Mário – Se Controla
- Puerto Rico: Bad Bunny ft. Bomba Estéreo – Ojitos Lindos
- Libya: Bahjat – Fiya || بهجت – فيا
- Denmark: Lukas Graham – Love Someone

RED VELVET CAKE
ORIGINAL RECIPE


Kids Share Their Holiday Traditions | Kids Try | HiHo Kids

794,455 views • Dec 25, 2021 • Kids try their holiday traditions with their best friends!

Profile ALAS. Martin Perez (Mar del Plata, Argentina)
ALAS Pro Tour May 31, 2020

¿QUE SIGNIFICA EL TOUR ALAS EN TU VIDA? Esa es la pregunta que le hicimos a algunxs surfistas que hace años viene siguiendo nuestro tour latinoamericano. Porque el surf es más que un deporte o una disciplina física. Es una forma de expresión, es vibrar desde la profundidad del ser, es sumergirse, es salir y estallar en segundos. Para quienes sienten el surf tan latente es como una constante perfección hermosamente imperfecta; porque nunca hay una ola igual a otra. Surfear es como el borrador de una obra maestra… es un arte.
WHAT DOES THE ALAS TOUR MEAN IN YOUR LIFE? That’s the question we asked some surfers who have been following our Latin American tour for years. Because surfing is more than a sport or a physical discipline. It is a form of expression, it is vibrating from the depth of one’s being, it is immersing oneself, it is coming out and exploding in seconds. For those who feel surfing so latent, it is like a constant, beautifully imperfect perfection; because there is never one wave the same as another. Surfing is like the draft of a masterpiece… it’s an art.

