

Mauritania, officially the Islamic Republic of Mauritania is a sovereign country in Northwest Africa. It is bordered by the Atlantic Ocean to the west, Western Sahara to the north and northwest, Algeria to the northeast, Mali to the east and southeast, and Senegal to the southwest. By land area, Mauritania is the 11th-largest country in Africa and the 28th-largest in the world, and 90% of its territory is situated in the Sahara. Most of its population of 4.4 million lives in the temperate south of the country, with roughly one-third concentrated in the capital and largest
Mauritania is culturally and politically part of the Arab world; it is a member of the Arab League and Arabic is the sole official language. The official religion is Islam, and almost all inhabitants are Sunni Muslims. Despite its prevailing Arab identity, Mauritanian society is multiethnic; the Bidhan, or so-called “white moors”, make up 30% of the population, while the Haratin, or so-called “black moors”, comprise 40%. Both groups reflect a fusion of Arab-Berber ethnicity, language, and culture. The remaining 30% of the population comprises various sub-Saharan ethnic groups.
Despite an abundance of natural resources, including iron ore and petroleum, Mauritania remains poor; its economy is based primarily on agriculture, livestock, and fishing. Mauritania is generally seen as having a poor human rights record, and is particularly censured for the perpetuation of slavery as an institution within Mauritanian society. It abolished the practice in 1981, and criminalized the ownership of slaves outright in 2007.
Source:https://en.wikipedia.org/wiki/Mauritania

COMMUNITY

Lessons in lifesaving from Brazil
What the biggest country in South America can teach the world about healthcare.
By Bill Gates December 12, 2023 – EXEMPLARY

The country’s Bolsa Familia program—which provides cash transfers to poor families if they meet certain conditions, including vaccination for children and prenatal care—deserves credit too. Expanded in tandem with primary healthcare, Bolsa Familia is just one of the
many social programs Brazil has built out over the past few decades that have
helped lift almost a fifth of the country’s population out of poverty. But it’s
also helped broaden healthcare access and usage by giving people an incentive
to enter the healthcare system—which is how Bolsa Familia has contributed
to reductions in child mortality as well.
I’ve been able to learn about these initiatives through the Gates Foundation’s partnership with Brazil’s Ministry of Health—which has focused on combatting malaria, improving vaccine production, leveraging local brainpower to address global health issues, and
documenting the impact of social and health programs through data sciences. And
I’ve been really impressed.
Of course, despite all the progress that’s been made in recent decades, Brazil still faces challenges. Financial crises and austerity budgets have led to cuts in healthcare spending, for example, and there are still districts where poorer residents have no access to
CHWs.
But Brazil’s healthcare system doesn’t have to be perfect to serve as proof of what happens when a country invests strategically in care for its most vulnerable: The returns are often
far-reaching and life-changing.
That is why Brazil is highlighted by the Exemplars in Global Health program, which I helped launch in 2020. The program’s mission is to identify countries that have made remarkable progress on health problems, understand the keys to their success, and share those insights globally so others can make similar progress. By that
standard, Brazil has a lot to teach.
That’s not to say any country can or should replicate Brazil’s approach exactly, since no two countries are alike. But with the right mix of investment and innovation, Brazil has made great strides in becoming a healthier place for its people. If the country continues
on that path and keeps doing what it’s done well already, and if other
countries follow—or simply forge their own paths with Brazil in mind—we’ll have
a healthier world, too.


Susan Hepworth, Suzanne Staebler, DNP, APRN, NNP-BC, FAANP, FAAN, Mitchell Goldstein, MD, MBA, CML
When hospital procurement decisions are focused on cost, patients pay the price
Hospitals must include NICU and PICU clinicians in the procurement process for medications, devices, supplies and services to ensure vulnerable infants and young children receive the safest care possible.
Hospital procurement is the process of purchasing medications, devices, and other supplies and services for use at the hospital. Procurement is a long process, usually completed by teams of doctors, nurses and other hospital staff. The process can be a determining factor in health outcomes for patients. Some hospital procurement teams face pressure to keep costs low, so clinical staff have less input in the process than administrators. This can lead to the hospital purchasing products and services that present safety issues for certain patient populations.
INFANTS AND CHILDREN ARE NOT LITTLE ADULTS.
The problem is especially pressing in neonatal and pediatric intensive care units. For example, the hospital may procure a large inventory of tubing and syringe systems to be used across all hospital units. But these tubing and syringe systems can present serious safety issues for NICU patients. Inefficient procurement processes can force clinicians to find workarounds, causing them to lose time with their patients. Inventory imbalances in the NICU and PICU can also force hospitals to delay or cancel procedures or treatments. NICU and PICU clinical staff members know the unique needs of their patients. Ensuring they are part of hospital procurement processes will promote the safest and best care possible for infants and young children.
Infants need medications and devices that are specifically designed and tested for them.
Policies must prioritize and incentivize companies to develop medications and devices specifically for the neonatal and pediatric populations to ensure safe and optimal care.
Infants and young children need care that is tailored to their needs and size. Infants are not tiny adults, yet they are often given smaller doses of adult medications or smaller sized adult medical devices.
ADULT MEDICATIONS AND DEVICES THAT ARE ALTERED FOR BABIES CAN PRESENT SAFETY CONCERNS.
This practice can result in medication dosing errors or device safety issues, which can lead to poor patient outcomes. For example, the pulse oximeter was made for adults but was often used on infants. Although the device saved many adult lives, it was not reliable when used on infants and children because they have reduced blood flow to their fingers and toes, which makes it harder to accurately measure oxygen saturation with the oximeter. Clinicians recognized infants needed technology specifically for their size, and since then, innovators have developed new oxygen monitoring technologies specifically for infants.
But innovation for new medications and devices faces barriers. Innovation for this small group of patients can be costly and time consuming, and enrolling infants and children in clinical trials can be challenging.
Providers also need to be willing to become early adopters of new technology.
It is important to ensure each patient in the NICU and PICU receives the highest quality of care during their hospital stay, which includes devices and medications that are specifically designed for their size and unique needs.
Policies that incentivize and prioritize innovation, like patent extensions, priority review vouchers or tax credits, will ensure more innovation to meet the needs of infants and young children.
Source:https://neonatologytoday.net/newsletters/nt-nov23.pdf
Hamzo Bryn & Macsim Daddy Feat Mouna DenDenni – Vive La Mauritanie | عاشت موريتان
Mouna DenDenni and Macsim Daddy are native Mauritanians and Hamzo Bryn is Mauritian and Moroccan


5 Facts About Healthcare In Mauritania
– Olivia Bielskis 09/25/2020
The Islamic Republic of Mauritania is a vast desert country with a significant nomadic population. These facets of Mauritania’s geography present challenges for creating healthcare infrastructure. In particular, physical distance and large rural populations make distributing care a massive undertaking. Accordingly, there are only 0.19 practicing physicians per 1,000 people in Mauritania. Here are five facts about healthcare in Mauritania.
- A lack of proper infrastructure devastates public health in rural, vulnerable regions. Problems stemming from poor sanitation and a lack of clean water plague Mauritania. Many areas of Mauritania go completely without consistent water sources due to geographic barriers. Overall, the capital city of Nouakchott is the only region with adequate water supply and treatment. This lack of water leads to serious consequences for healthcare in Mauritania. According to the World Health Organization, 2,150 Mauritanians die from diarrheal disease per year. Ninety percent of these deaths are linked to a lack of sanitation and insufficient access to clean water. In addition, droughts and desertification are preventing rural populations from accessing water at all. This is yet another challenge to improving healthcare in Mauritania.
- Many political barriers inhibit attempts to improve healthcare in Mauritania. The country suffers from a shortage of doctors and treatment facilities in rural areas of the country. While there are potential avenues for funding expansion, the Mauritanian government tends to keep infrastructure projects centralized to the capital region. Although the capital is the largest city and presents the most promise for economic growth, this neglects rural citizens. For example, the national insurance program prioritizes a portion of the urban population, as it only covers government officials and those who are formally employed. Poverty-stricken people are further disadvantaged by the astronomical cost of healthcare without any insurance. Thankfully, groups like the Institute of Tropical Medicine are working to provide a concerted effort to expand healthcare in Mauritania.
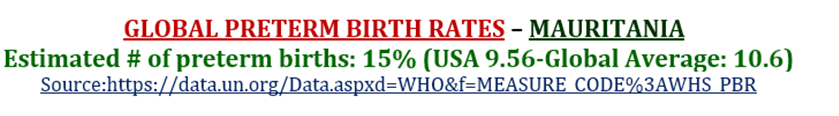
- Mauritania struggles with reproductive and neonatal care. According to the World Bank, Mauritania has a birthrate of 4.62. Combined, the birthrate and lack of adequate neonatal care lead to high infant and maternal mortality. However, the International Development Association is dedicating $23 million to expanding the reach and quality of maternal, neonatal and reproductive healthcare in Mauritania. The initiative also aims to combat childhood malnutrition by investing in further healthcare and nutrition services for children. These efforts, part of the Mauritania Health System Support project, aspire to alleviate issues in healthcare beyond the capital city. This will provide much-needed relief to rural and refugee populations.
- International aid is going toward healthcare in Mauritania. The International Development Association of the World Bank is providing funds to help local governments build sanitation and water treatment infrastructure. These funds will address the gross centralization of public utilities and expand access to water and sanitation services into rural areas. With tools to manage public services provided through the Decentralization and Productive Intermediate Cities Support project, localities will have the means to create a substantive foundation for healthcare in Mauritania.
- The Institute of Tropical Medicine is also promoting healthcare in Mauritania. In her 2018 article for the Institute of Tropical Medicine, public health expert Kirsten Accoe details how the ITM intends to establish a local health system team in the country. This team would tackle healthcare on the district level in conjunction with centralized efforts to improve healthcare. The initiative aims to create sustained quality care by increasing the retention of healthcare workers in each district, which has previously been an issue due to lack of funding, equipment and trained personnel. ITM’s effort can therefore allow more to people get the relief they deserve.
Improving healthcare in Mauritania is certainly a complex task. But the government and aid organizations can come together to cultivate a coordinated effort to improve infrastructure, assist healthcare professionals at the district level and expand the reach of care. In doing so, they will begin to create an equitable healthcare system and provide all Mauritanians with the care they deserve.
Source:https://borgenproject.org/healthcare-in-mauritania/

HEALTHCARE PARTNERS

Preterm Birth and Infantile Appendicitis
2023 Dec 1;152(6):e2023063815. doi: 10.1542/peds.2023-063815.
Yakun Liu 1, Xiaoxiao Yu2, Guoqing Zhang3, Chuanping Xie4, Yang Li 5, Pengfei Mu 6 7, Shuai Chen 6 7, Yajun Chen4, Shungen Huang1

Abstract
Objective: To investigate the potential association between preterm birth and infantile appendicitis.
Methods: We conducted a retrospective, multicenter, matched case-control study. This study included consecutive patients <1 year of age with surgery- or autopsy-confirmed appendicitis, admitted between December 2007 and May 2023. For each case, 10 healthy infants were randomly selected and matched by age. Infants were categorized as neonates (0 to 28 days) or older infants (>28 days and <1 year).
Results: The study included 106 infants diagnosed with appendicitis (median age 2.4 months) and 1060 age-matched healthy controls. In the univariate analysis, preterm birth was significantly associated with the development of appendicitis within the first year of life (odds ratio [OR], 4.23; 95% confidence interval [CI], 2.67-6.70). Other factors associated with a higher risk of infantile appendicitis included being male (OR, 1.91; 95%CI, 1.25-2.94), weight-for-age z-score (OR, 0.72; 95%CI, 0.64-0.81), and exclusively fed on formula (OR, 2.95; 95%CI, 1.77-4.91). In multivariable analyses, preterm remained significantly associated with appendicitis (adjusted OR, 3.32; 95%CI, 1.76-6.24). Subgroup analysis revealed that a preterm birth history increased the risk of appendicitis in both neonates (adjusted OR, 4.56; 95%CI, 2.14-9.71) and older infants (adjusted OR, 3.63; 95%CI, 1.72-7.65). However, preterm did not significantly influence the incidence of appendiceal perforation.
Conclusions: Preterm infants have an increased risk of appendicitis during the first year of life. A preterm birth history may help improve the timely diagnosis of infantile appendicitis.

The Pediatric Subspecialty Physician Workforce
Frederick P. Rivara, MD, MPH1; Javi Gonzalez-del-Rey, MD2; Christopher B. Forrest, MD, PhD3
JAMA Pediatr. Published online December 18, 2023. doi:10.1001/jamapediatrics.2023.5235 December 18, 2023

Over the past 20 years, the health care needs of children and the increasing complexity of their care has changed due to medical advances and rapidly changing developmental ecosystems. In addition, patterns of where and how children are treated in the health care system have evolved. These changes have contributed to an increased demand for pediatric subspecialty services and have raised concerns about the current and future availability of pediatric subspecialty care and research. Combined with substantial disincentives to pursuing a career as a pediatric subspecialist, these changes hold the potential to negatively influence children’s health.
In 2022, the National Academies of Sciences, Engineering, and Medicine, with support from a coalition of sponsors, formed the Committee on the Pediatric Subspecialty Workforce and Its Impact on Child Health and Well-Being1 to recommend actions for a future that ensures adequate pediatric subspecialty care and a robust research portfolio to advance the health and health care of for the nation’s infants, children, and adolescents. This Viewpoint summarizes 4 strategic goals with associated recommendations the committee developed to help achieve this vision.
Promote Collaboration and the Effective Use of Services Between Pediatric Primary Care Clinicians and Subspecialty Physicians
The committee envisioned a health system that enables all children to receive the appropriate type and amount of primary and specialty care whenever they need it. A larger workforce alone is not sufficient. Efforts are needed to recruit and retain subspecialists while more judiciously using all members of the health care team in effective models of care. The committee recommends that the Agency for Healthcare Research and Quality should periodically report on the changing demands and needs for pediatric primary and subspecialty care, access to to care, disparities in receipt of services, and the nature of the workforce (including data on clinicians from backgrounds underrepresented in medicine).
Data indicate that a substantial proportion of visits to pediatric subspecialists are for problems that should be managed in primary care. To foster more appropriate referrals, the committee recommends that the American Academy of Pediatrics, the Council of Pediatric Subspecialties, and other pediatric professional societies should collaboratively develop, disseminate, and implement testing, management, and referral guidelines for conditions commonly managed by subspecialists. The ability to provide interprofessional and team-based care to enhance access to pediatric subspecialty care will require insurers to adequately reimburse these newer delivery models such as virtual consultations, telehealth, and integrated care teams. Although the committee was not tasked with reviewing health care systems and delivery models, innovations in the primary–specialty care interface and the pediatric subspecialty referral and care coordination processes are needed and should be sponsored, developed, and evaluated by the Centers for Medicare and Medicaid Services in conjunction with state Medicaid agencies, private foundations, and health systems.
Reduce Financial and Payment Disincentives
Physician payment is largely driven by private and public health insurers who contract with and reimburse clinicians. Medicaid covers 35% of children overall and 50% or more of the children with complex medical needs treated by pediatric subspecialty physicians. The high percentage of patients covered by Medicaid, which generally has lower reimbursement rates compared to Medicare, coupled with low relative value unit–based payment rates, adversely affects the financing of pediatric care. To address the factors that contribute to limited access and invest in children’s health, the committee calls on Congress to provide funds within the next 5 years to increase Medicaid payment rates for pediatric services, achieving or exceeding parity with Medicare rates. These federal funds should be provided to all states, and the payment increases should be mandatory. The Centers for Medicare and Medicaid Services should prioritize attention to pediatric services in assigning relative value units that accurately reflect time and resource use for pediatric subspecialty care.
As a result of lower salaries for some subspecialties and longer training, pediatric subspecialists may face a high debt burden, which can discourage pediatricians from careers in lower-paid subspecialties. Funding of the Pediatric Specialty Loan Repayment Program should be increased to $30 million as originally authorized. The program should focus on loan repayment for high-priority pediatric medical subspecialties as well as subspecialists from backgrounds that are underrepresented in medicine or economically disadvantaged.
Enhance Education, Training, Recruitment, and Retention
The current model requiring 3 years of training for pediatric medical subspecialists has limited flexibility in the design and length of fellowship. Currently, streamlined pathways are not available for trainees who are committed to careers in clinical practice. The committee asks the American Board of Pediatrics, the American Osteopathic Board of Pediatrics, and the Accreditation Council for Graduate Medical Education to develop, implement, and evaluate distinct fellowship pathways, including a 2-year option for those who aspire to a career with a primary focus on clinical care. It also calls on the Association of Medical School Pediatric Department Chairs to convene representatives from the American Board of Pediatrics, the Accreditation Council for Graduate Medical Education, pediatric professional societies, and pediatric education organizations to adjust training curricula for pediatric residents and fellows. Achieving this goal will likely require input from the different pediatric specialties to the American Board of Pediatrics.
The current funding of graduate medical education, including Medicare graduate medical education and Children’s Hospital graduate medical education, needs to be reformed by Congress. Funding should be distributed to address priority pediatric workforce needs, such as increased inclusion of clinicians from backgrounds underrepresented in medicine, high-priority subspecialties, geographic shortages, and enhanced training for new models of care.
Pediatric department chairs, medical school deans, and health systems should develop, implement, and publicly report on plans and outcomes to attract, support, and retain students, residents, fellows, and faculty from backgrounds that are underrepresented in in pediatric subspecialties. These plans should include efforts to further the development and growth of recruitment programs for precollege students from backgrounds underrepresented in medicine and initiatives to make learning and working environments more inclusive.
Support the Pediatric Physician-Scientist Pathway
Pediatric subspecialty physician-scientists play a critical role in advancing children’s health through research. However, the number and level of funding for career development programs are inadequate to develop and maintain a robust pediatric-scientist workforce. The National Institutes of Health and Agency for Healthcare Research and Quality should increase the number of career development grants in pediatrics, particularly institutional training awards, the Pediatric Loan Repayment Program, and K awards, with attention to providing such grants to physician-scientists from backgrounds that are underrepresented in the scientific workforce and for high-priority subspecialties in pediatric research. Funding for individual K awards should be increased to reflect current salaries and research expenses and should include additional funding for mentorship.
It is difficult to fully characterize the pediatric subspecialty physician-scientist workforce due to data limitations, with little to no coordination between the funders of pediatric research training programs. The committee asks the National Institutes of Health Pediatric Research Consortium, with leadership from the National Institute of Child Health and Human Development and input from the National Institutes of Health’s Scientific Workforce Diversity Office to engage with other government and nongovernment pediatric research funders to create and maintain a publicly available central repository for data on pediatric physician-scientists’ funding and success throughout their careers, including the development of new measures to understand the initial success and retention of pediatric physician-scientists. The Association of Medical School Pediatric Department Chairs should provide supplemental data as needed.
Summary
The current health care system is expensive, inequitable, and not fully satisfying to the people who work in it or the patients and families it serves. This report outlines recommendations that may improve the quality of pediatric medical subspecialty care. Ensuring an adequate level of pediatric subspecialty care to meet the needs of US children will require concerted efforts across federal and state governments, professional societies, major education and training organizations, medical schools, fellowship programs, and health systems, with authentic participation from patients and families. It will also require a willingness to adapt to the rapidly changing needs of children and clinicians. Implementing these recommendations while providing necessary support to primary care will contribute to development of a health care system that better serves the needs of all children and improves the current and future health of the nation.
Corresponding Author: Frederick P. Rivara, MD, MPH, Seattle Children’s and the University of Washington, Building Cure, PO Box 5371, Seattle, WA 98145-5005 (fpr@uw.edu).

NICU versus Mother/Baby Unit Admission for Low-Acuity Infants Born at 35 Weeks’ Gestation

For low-acuity 35-week gestation infants, NICU (versus Mother/Baby Unit) admission was associated with increased length of stay, decreased exclusive breast milk feeding, and decreased readmission.
PLAY VIDEO HERE:



PREEMIE FAMILY PARTNERS

New parent? Check 10 ways to support the developmental needs of premature babies
By Zarafshan Shiraz, New Delhi Oct 17, 2023 04:16 PM IST

Bringing a new life into the world is a remarkable and awe-inspiring experience however, for parents of premature babies, it can also be a journey filled with unique challenges. Premature birth, defined as birth before 37 weeks of pregnancy, can raise concerns about a baby’s development.
In an interview with HT Lifestyle, Dr Suresh Birajdar, Neonatologist and Pediatrician at Motherhood Hospital in Kharghar, spilled the beans on navigating the early journey of developmental concerns in premature babies, what to expect and how to support their developmental needs.
1. Delicate Beginnings: Understanding Prematurity
Premature birth can happen for various reasons, including maternal health issues, multiple pregnancies (e.g., twins or triplets), or unknown causes. The degree of prematurity can vary, with some babies born just a few weeks early and others several months prematurely. Each premature baby’s developmental journey is unique.
2. Adjusted Age: A Key Concept
When assessing the developmental milestones of premature babies, it’s essential to consider their “adjusted age.” This means calculating their developmental age based on their due date rather than their actual birth date. Adjusted age accounts for the time spent in the womb, providing a more accurate picture of their developmental progress. Sometimes, it is also called as “corrected gestation”.
3. Growth and Weight Gain: Early Priorities
Premature babies often need specialized care in neonatal intensive care units (NICUs) to support their growth and weight gain. Adequate nutrition is critical during this period, as it helps preemies catch up to their full-term peers in terms of size and strength. Healthcare professionals closely monitor their weight and growth to ensure they are thriving.
4. Respiratory Challenges: Breathing Support
Premature babies may have underdeveloped lungs, requiring respiratory support in the form of oxygen therapy or mechanical ventilation. These interventions can affect their early development, but the good news is that with proper care, many preemies eventually outgrow these challenges.
5. Neurodevelopmental Delays: Monitoring Progress
Premature birth can increase the risk of neurodevelopmental delays, which may manifest as challenges in motor skills, language development, and cognitive abilities. Early intervention programs and developmental assessments can help identify and address these concerns.
6. Feeding Challenges: Patience and Persistence
Feeding can be a significant concern for premature babies. They may have difficulty breastfeeding or bottle-feeding due to weak sucking reflexes or coordination issues. Working closely with a lactation consultant or feeding therapist can be instrumental in overcoming these challenges.
7. Sensory Sensitivities: A Gradual Adjustment
Premature babies may exhibit heightened sensitivity to light, noise, and touch. Creating a calm and soothing environment in the NICU and at home can help premature infants gradually adjust to the sensory stimuli of the outside world.
8. Kangaroo Care: The Power of Touch
Kangaroo care, where the baby is held against the parent’s skin, has proven to be highly beneficial for premature infants. It promotes bonding, regulates the baby’s body temperature, and supports overall development.
9. Developmental Milestones: Celebrate Progress
Parents and caregivers need to celebrate every developmental milestone achieved, no matter how small. Premature babies may reach certain milestones later than full-term infants, but with time and support, most babies catch up.
10. Seek Support: You’re Not Alone
Parenting a premature baby can be emotionally challenging. Reach out to support groups, healthcare professionals, and early intervention services for guidance and reassurance. Connecting with other parents who have experienced similar journeys can provide invaluable support.
The developmental concerns in premature babies are real but they are also surmountable and with early intervention, specialised care and unwavering parental love and support, premature babies can overcome many challenges and thrive. Every milestone achieved is a testament to their strength and resilience, reminding us of the remarkable journey they’ve embarked upon from their very first breath.

Obstetric and neonatal outcomes in pregnant women with and without a history of specialist mental health care: a national population-based cohort study using linked routinely collected data in England
Julia Langham, PhD-Ipek Gurol-Urganci, PhD-Patrick Muller PhD-Kirstin Webster, MSc-Emma Tassie, MSc-Margaret Heslin, PhD

Summary:
Background
Pregnant women with pre-existing mental illnesses have increased risks of adverse obstetric and neonatal outcomes compared with pregnant women without pre-existing mental illnesses. We aimed to estimate these differences in risks according to the highest level of pre-pregnancy specialist mental health care, defined as psychiatric hospital admission, crisis resolution team (CRT) contact, or specialist community care only, and the timing of the most recent care episode in the 7 years before pregnancy.
Methods
Hospital and birth registration records of women with singleton births between April 1, 2014, and March 31, 2018 in England were linked to records of babies and records from specialist mental health services provided by the England National Health Service, a publicly funded health-care system. We compared the risks of adverse pregnancy outcomes, including fetal and neonatal death, preterm birth, and babies being born small for gestational age (SGA; birthweight <10th percentile), and composite indicators for neonatal adverse outcomes and maternal morbidity, between women with and without a history of contact with specialist mental health care. We calculated odds ratios adjusted for maternal characteristics (aORs), using logistic regression.
Findings
Of 2 081 043 included women (mean age 30·0 years; range 18–55 years; 77·7% White, 11·4% South Asian, 4·7% Black, and 6·2% mixed or other ethnic background), 151 770 (7·3%) had at least one pre-pregnancy specialist mental health-care contact. 7247 (0·3%) had been admitted to a psychiatric hospital, 29 770 (1·4%) had CRT contact, and 114 753 (5·5%) had community care only. With a pre-pregnancy mental health-care contact, risk of stillbirth or neonatal death within 7 days of birth was not significantly increased (0·45–0·49%; aOR 1·11, 95% CI 0·99–1·24): risk of preterm birth (<37 weeks) increased (6·5–9·8%; aOR 1·53, 1·35–1·73), as did risk of SGA (6·2– 7·5%; aOR 1·34, 1·30–1·37) and neonatal adverse outcomes (6·4–8·4%; aOR 1·37, 1·21–1·55). With a pre-pregnancy mental health-care contact, risk of maternal morbidity increased slightly from 0·9% to 1·0% (aOR 1·18, 1·12–1·25). Overall, risks were highest for women who had a psychiatric hospital admission any time or a mental health-care contact in the year before pregnancy.
Interpretation
Information about the level and timing of pre-pregnancy specialist mental health-care contacts helps to identify women at increased risk of adverse obstetric and neonatal outcomes. These women are most likely to benefit from dedicated community perinatal mental health teams working closely with maternity services to provide integrated care.
Funding: National Institute for Health Research.
Source:https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(23)00200-6/fulltext


Down Syndrome for New Parents: What to Know During the First Year | Mass General Brigham
Mar 11, 2022 Mass General Brigham

What will the first year of life be like for a baby with Down syndrome? What kind of support and care do they need? What is it like being a sibling of a child with Down syndrome? Brian Skotko, M.D, M.P.P., Medical Geneticist and Emma Campbell Endowed Chair on Down Syndrome at MassGeneral Hospital for Children, explains what parents can expect during the first year of raising a child with Down syndrome, including information on breastfeeding, necessary testing, and more. Down Syndrome Clinic to You: https://www.dsc2u.org/

Preterm Birth Increases Health Vulnerabilities of Babies With Down Syndrome
April 19, 2023 – JoAnna Pendergrass, DVM
Babies with Down syndrome who are born preterm have higher prenatal morbidity and mortality rates than those in babies with Down syndrome born at term, suggesting pediatricians can lower their risk threshold for certain screenings or interventions.
Compared with age-matched neonates without Down syndrome, babies with Down syndrome are more likely to experience developmental delay, gastrointestinal disorders and poor growth, among other challenges.
Neonates with Down syndrome who are born prematurely face an even steeper uphill health battle.
In a study published in the Journal of Perinatology, researchers reported that morbidity and mortality rates were significantly higher in neonates with Down syndrome born before 34 weeks of gestation than in those born later.
“Studies of babies with Down syndrome have not reported health outcomes according to gestational age,” says Emily Messick, DO, pediatrician at Nationwide Children’s Hospital and lead author of the study. “We began this project to address this gap in the literature.”
For their single-center retrospective study, the team analyzed the medical records of 314 neonates with Down syndrome who were treated at Nationwide Children’s NICU from 2010 to 2020.
Neonates were grouped according to gestational age: <34 weeks (n=31), 34 to 36 weeks (n=68), 37 to 38 weeks (n-127) and ≥39 weeks (n=88).
Data collected included prenatal and neonatal characteristics and morbidities experienced during the first year of life, such as necrotizing enterocolitis (NEC) and congenital abnormalities.
Morbidity rates were highest in neonates born before 34 weeks of gestation.
Fox example, three of the six neonates in the study who developed NEC were born before 34 weeks. The rates of oxygen supplementation and gastrostomy tube placement were greatest for the <34-week group than the other groups. Also, the use of nitric oxide, commonly used to treat respiratory failure associated with persistent pulmonary hypertension of the newborn, was highest for neonates born before 34 weeks.
The overall mortality rate in the study was 4.5%, with in-hospital mortality rates being highest (19%) in those born before 34 weeks. The most recent data for infant mortality in the US indicate a <1% mortality rate for infants born at 34 to 36 weeks.
“Awareness of those neonates’ higher morbidity risks can drop the threshold for certain screening tests and prompt the early involvement of other sub-specialists to help improve long term outcomes,” says Dr. Messick.
A multidisciplinary approach that is comprehensive and individualized is integral to improving outcomes for neonates with Down syndrome. For example, “A team of dietitians, speech therapists and gastroenterologists can help optimize growth for patients with feeding difficulties and poor growth,” notes Dr. Messick.
Keeping a patient’s family informed while the baby is in the NICU is key. “It is also helpful to look at the big picture and assess what goals need to be met for the baby to be discharged home with the family,” she adds.


The joy of raising a child with Down syndrome
KING 5 Seattle Oct 3, 2019

KING 5 Meteorologist Jordan Steele’s son was born earlier this year with Down syndrome. His family went through a wave of emotions, but say they’re trusting the journey.


INNOVATIONS

Maternal Migration Background and Mortality Among Infants Born Extremely Preterm
Joaquim Vidiella-Martin, PhD1,2; Jasper V. Been, PhD3,4,5 December 13, 2023

Key Points
Question Is maternal migration background associated with neonatal intensive care unit (NICU) admission and survival?
Findings In this cross-sectional study of 1405 live births in the Netherlands (2010-2017), infants born to migrant mothers between 24 weeks 0 days and 25 weeks 6 days of gestation had lower risk of mortality within the first year of life than infants born to mothers with no migration background. This was unlikely to be explained by differences in admission, in care across NICUs, or in preferences for active obstetric management across migration backgrounds.
Meaning These results suggest that maternal migration background is associated with increased survival of extremely preterm infants admitted to Dutch NICUs, and further research is needed to understand the underlying factors.
Abstract
Importance Extremely preterm infants require care provided in neonatal intensive care units (NICUs) to survive. In the Netherlands, a decision is made regarding active treatment between 24 weeks 0 days and 25 weeks 6 days after consultation with the parents.
Objective To investigate the association between maternal migration background and admissions to NICUs and mortality within the first year among extremely preterm infants.
Design, Setting, and Participants This cross-sectional study linked data of registered births in the Netherlands with household-level income tax records and municipality and mortality registers. Eligible participants were households with live births at 24 weeks 0 days to 25 weeks 6 days gestation between January 1, 2010, and December 31, 2017. Data linkage and analysis was performed from March 1, 2020, to June 30, 2023.
Exposure Maternal migration background, defined as no migration background vs first- or second-generation migrant mother.
Main Outcomes and Measures Admissions to NICUs and mortality within the first week, month, and year of life. Logistic regressions were estimated adjusted for year of birth, maternal age, parity, household income, sex, gestational age, multiple births, and small for gestational age. NICU-specific fixed effects were also included.
Results Among 1405 live births (768 male [54.7%], 546 [38.9%] with maternal migration background), 1243 (88.5%) were admitted to the NICU; 490 of 546 infants (89.7%) born to mothers with a migration background vs 753 of 859 infants (87.7%) born to mothers with no migration background were admitted to NICU (fully adjusted RR, 1.03; 95% CI, 0.99-1.08). A total of 652 live-born infants (46.4%) died within the first year of life. In the fully adjusted model, infants born to mothers with a migration background had lower risk of mortality within the first week (RR, 0.81; 95% CI, 0.66-0.99), month (RR, 0.84; 95% CI, 0.72-0.97), and year of life (RR, 0.85; 95% CI, 0.75-0.96) compared with infants born to mothers with no migration background.
Conclusions In this nationally representative cross-sectional study, infants born to mothers with a migration background at 24 weeks 0 days to 25 weeks 6 days of gestation in the Netherlands had lower risk of mortality within the first year of life than those born to mothers with no migration background, a result that was unlikely to be explained by mothers from different migration backgrounds attending different NICUs or differential preferences for active obstetric management across migration backgrounds. Further research is needed to understand the underlying mechanisms driving these disparities, including parental preferences for active care of extremely preterm infants.
Published: December 13, 2023. doi:10.1001/jamanetworkopen.2023.47444

Babies born very premature can have brain development disrupted in intensive care unit, review finds
03/08/23

Study says little progress has been made in preventing development problems when infants born more than two months early
While most babies born more than two months prematurely now survive thanks to medical advances, little progress has been made in the past two decades in preventing associated developmental problems, an expert review has found.
The review also found that very preterm babies can have their brain development disrupted by environmental factors in the neonatal intensive care unit (NICU), including nutrition, pain, stress and parenting behaviours.
Each week in Australia more than 50 babies are born very preterm – at fewer than 32 weeks’ gestation – increasing their risk of disrupted brain development. Many of these infants have no or mild issues but some experience developmental delays, deafness, blindness, cerebral palsy and behavioural issues.
A review conducted by experts from the Children’s Hospital of Orange County in the US and the Turner Institute for Brain and Mental Health at Monash University in Australia found that while these neurodevelopmental problems can be related to brain injury during gestation or due to cardiac and respiratory issues in the first week of life, the environment of the NICU is also critical.
Published on Thursday in the New England Journal of Medicine (NEJM), the review examined research that used brain magnetic resonance imaging (MRI) shortly after birth, including new insights from advanced neuroimaging techniques as well as studies of infant nervous systems.
“Over the past two decades, the incidence of cerebral palsy, particularly severe cerebral palsy, has declined,” the review found. “However, there has been no decline in the high incidence of cognitive impairment and social and emotional challenges among children and young adults born preterm.”
Dr Peter Anderson, a co-author of the paper and professor of paediatric neuropsychology at Monash University, said the review sought to better understand why some children born very early experience significant problems while others experience none.
“This particular period in their third trimester of pregnancy is well known to be a period where there is an enormous development in the brain … probably the most dynamic and rapid period of development in the brain throughout the lifespan,” Anderson said.
An injury during this period can alter the normal brain development processes . But the review found that even if the infant has no injury to the brain, development can be affected by environmental factors after birth.
“They’re experiencing enormous levels of stress as a result of a whole range of different factors, including loud noises and lights, which they wouldn’t be being exposed to in utero,” Anderson said.
To improve outcomes for very preterm babies, the review recommended family based interventions that reduce parental stress during gestation, more research into rehabilitation in intensive care and in the early months of life, and greater understanding of the role of environment and parenting after birth.

Evaluation of Sleep Practices and Knowledge in Neonatal Healthcare
de Groot, Eline R. MSc; Ryan, Mary-Anne MSc, RN; Sam, Chanel BSc; Verschuren, Olaf PhD; Alderliesten, Thomas PhD, MD; Dudink, Jeroen PhD, MD; van den Hoogen, Agnes PhD, RN
Abstract
Background:
Developmental care is designed to optimize early brain maturation by integrating procedures that support a healing environment. Protecting preterm sleep is important in developmental care. However, it is unclear to what extent healthcare professionals are aware of the importance of sleep and how sleep is currently implemented in the day-to-day care in the neonatal intensive care unit (NICU).
Purpose:
Identifying the current state of knowledge among healthcare professionals regarding neonatal sleep and how this is transferred to practice.
Methods:
A survey was distributed among Dutch healthcare professionals. Three categories of data were sought, including (1) demographics of respondents; (2) questions relating to sleep practices; and (3) objective knowledge questions relating to sleep physiology and importance of sleep. Data were analyzed using Spearman’s rho test and Cramer’s V test. Furthermore, frequency tables and qualitative analyses were employed.
Results:
The survey was completed by 427 participants from 34 hospitals in 25 Dutch cities. While healthcare professionals reported sleep to be especially important for neonates admitted in the NICU, low scores were achieved in the area of knowledge of sleep physiology. Most healthcare professionals (91.8%) adapted the timing of elective care procedures to sleep. However, sleep assessments were not based on scientific knowledge. Therefore, the difference between active sleep and wakefulness may often be wrongly assessed. Finally, sleep is rarely discussed between colleagues (27.4% regularly/always) and during rounds (7.5%-14.3% often/always).
Implications:
Knowledge about sleep physiology should be increased through education among neonatal healthcare professionals. Furthermore, sleep should be considered more often during rounds and handovers.
Source:https://journals.lww.com/advancesinneonatalcare/pages/currenttoc.aspx

Mauritania: Zeinebou Abdeljelil promotes innovation and youth entrepreneurship
By : Melchior KobaDate : mercredi, 07 décembre 2022
With formal training in information technology and banking and finance, she helps entrepreneurs fulfill their ambition. Apart from being a business advisor, she also runs a startup incubator.
Zeinebou Abdeljelil (photo) is a Mauritanian tech entrepreneur and a financial management consultant. She holds two master’s degrees, one in banking and financial support services from IFID in Tunisia and the other in business and IT from ISG in Tunisia. She also completed a six-week program on entrepreneurship at the University of Notre Dame’s Mendoza College of Business in the United States.
With a firm belief that innovation and digital technologies have the potential to drive sustainable and inclusive growth in Africa, she co-founded – in 2014- Hadina RIMTIC, the first incubator focused on ICTs in Mauritania. Through her incubator, she organizes pitch competitions (MauriApp Challenge or the entrepreneurship marathon) and, to date she has supported more than 100 projects in the field of digital, livestock feed production, natural compost, and solar energy equipment.
“ There is a need to build the capacity of entrepreneurs in Mauritania, whether it is in the ideation of their projects, in the financial and day-to-day management of their start-ups, or in building their resilience to shocks,”she said earlier this year.
In 2015, she also co-founded IKLAAA Consulting, an agency aimed at building entrepreneurs’ capacities with strategic counseling and management advice. Apart from her entrepreneurship career, the Mandela Washington Fellowship Alumni has over a decade-long professional and consulting experience. Her professional career started, in 2010, with BAMIS Bank where she was a corporate relations manager.
In 2016, UNDP hired her as a capacity-building consultant for small and medium producers in Mauritania. After three months of working for the UNDP, she joined the anti-inequality non-profit organization, Oxfam Intermón, as a microfinance consultant in her country. In 2017, she officiated as a youth entrepreneurship development consultant for the World Bank Group and a Peace consultant for the United Nations Population Fund (UNFPA). The following year, she worked for Caritas Mauritania as a youth entrepreneurship development consultant.




May 16, 2023 #Learntoread #readalong #autismawareness
Masterpiece is an inclusive kids book celebrating a child on the autism spectrum. An Award-winning book, it recently won The Golden Wizard Book Prize and placed as a Top 3 Finalist for Book of the Year! Masterpiece is an inclusive story featuring Samuel, a boy on the autism spectrum who sees the world differently than his peers. When Samuel’s teacher asks his class to create a piece of art, it quickly becomes apparent that his beautiful way of looking at the world makes him a true masterpiece!


Top Premature Infant Health Conditions: Understanding and Embracing the Journey
As many of you who follow our neonatal health blog know, the journey of premature birth is both complex and heartening. Premature birth, defined as delivery before 37 weeks of gestation, presents a unique set of challenges and demands specialized care and attention. These tiny warriors, known affectionately as “preemies,” embark on a journey that is as much about medical resilience as it is about the strength of the human spirit. In our continuous effort to support and inform the neonatal community, we delve into the common health conditions faced by these remarkable infants. With advances in neonatal medicine and technology, the outlook for premature infants has become increasingly positive, turning many potential hardships into stories of triumph and hope.
In-Depth Exploration of Common Premature Infant Health Concerns
1. Respiratory Distress Syndrome (RDS): A prevalent issue in preemies, RDS is caused by underdeveloped lungs lacking sufficient surfactant. Treatments like artificial surfactant administration and ventilatory support have greatly improved survival rates and outcomes.
2. Intraventricular Haemorrhage (IVH): This condition involves bleeding in or around the brain’s ventricles. Severity varies, and treatments range from monitoring to surgical interventions, with regular brain scans being crucial.
3. Necrotizing Enterocolitis (NEC): A serious gastrointestinal disorder, NEC involves tissue death in parts of the bowel. Management includes stopping oral feedings, providing intravenous nutrition, administering antibiotics, and possibly surgery in severe cases.
4. Patent Ductus Arteriosus (PDA): A heart condition where a fetal blood vessel remains open post-birth, leading to potential heart failure and other complications. Treatment options include NSAID medications and surgery.
5. Jaundice: Common due to immature liver function, jaundice in preemies is treated effectively with phototherapy, which lowers bilirubin levels.
Focusing on Vision Health in Premature Infant
Premature infants often face a higher risk for vision issues, including Retinopathy of Prematurity (ROP). ROP, a condition where abnormal blood vessels grow in the retina, necessitates regular eye exams for early detection. Treatments may involve laser therapy or other surgical procedures.
Glasses: A Fun Twist on Vision Health for Preemies
As we delve deeper into the realm of premature infant health, we mustn’t overlook the unique and heartwarming aspect of vision health, especially when it comes to preemies. Premature infants are more susceptible to a range of vision issues, with one of the most common being Retinopathy of Prematurity (ROP). ROP is a condition in which abnormal blood vessels grow in the retina, and it requires vigilant monitoring and intervention. However, there is a delightful twist to this narrative for some preemies – the introduction of eyeglasses.
For those tiny warriors who need glasses to address their vision challenges, this requirement can become an unexpected source of joy and excitement. In today’s world, paediatric eyewear isn’t just functional; it’s also stylish and fun. These pint-sized glasses come in an array of designs, colours, and shapes, catering to the unique personalities of each preemie. From playful patterns to vibrant hues, glasses for premature infants are a canvas for self-expression.
Glasses can quickly transform from a medical necessity into a delightful accessory that not only helps preemies see the world more clearly but also adds a touch of charm to their appearance. Parents often find themselves choosing frames that reflect their child’s personality, turning the process of selecting eyewear into a bonding experience. Whether it’s a pair adorned with their favourite cartoon character or a set with glittering frames, these glasses allow preemies to showcase their individuality and style.
Moreover, the joy of wearing glasses extends beyond aesthetics. For preemies who have had to navigate a world filled with medical procedures and treatments, glasses can be a beacon of normalcy and empowerment. They provide a sense of control and ownership over their own health journey. These little ones quickly discover that glasses help them see the world more clearly, enabling them to engage with their surroundings, recognize their loved ones’ faces, and explore their environment with greater confidence.
Parents, too, find solace and delight in the fact that their preemies can express their uniqueness and personality through their eyewear. It’s a small but significant way to celebrate the resilience and strength of their child. Watching their little one embrace their glasses with enthusiasm can be an emotionally uplifting experience, reminding parents that their preemie is not defined by their medical challenges but rather by their spirit and character.
In Conclusion: A Celebration of Resilience and Growth
The journey of premature infants is marked by countless hurdles and triumphs, and their vision health is just one facet of this remarkable adventure. Every challenge they face, including the need for glasses, is met with advanced medical care and a creative, supportive approach. The introduction of fun and stylish glasses for preemies not only aids in vision correction but also celebrates the individuality and spirit of each incredible preemie.
As we continue to support and cheer for these tiny warriors on their journey to growth and resilience, let us remember that their unique path is filled with opportunities for joy and self-expression. Through fun glasses, we celebrate not only the developmental milestones but also the unwavering spirit of these incredible preemies. Here’s to their continued growth, thriving, and conquering of each step of their journey, with a dash of style and a lot of heart!


Surf exploration in the heart of the desert, Mauritania”, by Kepa Acero.

A surf exploration along the Mauritanian desert by Kepa Acero

