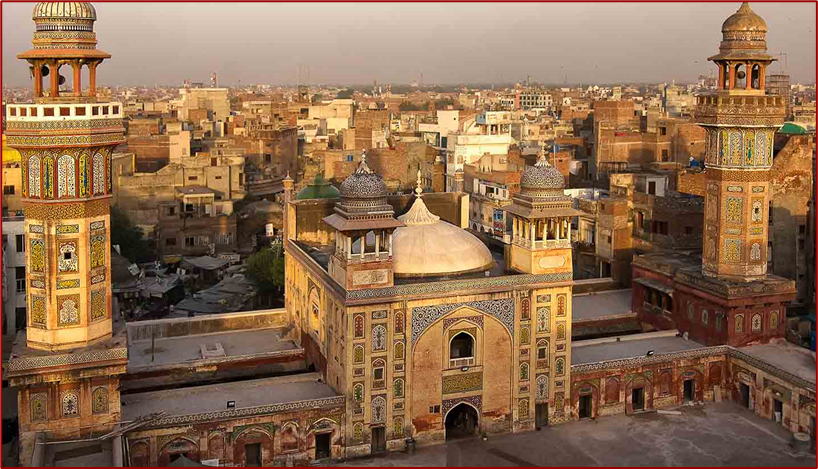

Pakistan, officially the Islamic Republic of Pakistan, is a country in South Asia. It is the fifth-most populous country, with a population of over 241.5 million, having the largest Muslim population as of 2023.Islamabad is the nation’s capital, while Karachi is its largest city and financial centre. Pakistan is the 33rd-largest country by area, being the second largest in South Asia. Bounded by the Arabian Sea on the south, the Gulf of Oman on the southwest, and the Sir Creek on the southeast, it shares land borders with India to the east; Afghanistan to the west; Iran to the southwest; and China to the northeast. It shares a maritime border with Oman in the Gulf of Oman, and is separated from Tajikistan in the northwest by Afghanistan’s narrow Wakhan Corridor.
Pakistan is a middle power nation, and has the world’s sixth-largest standing armed forces. It is a declared nuclear-weapons state, and is ranked amongst the emerging and growth-leading economies, with a large and rapidly-growing middle class. Pakistan’s political history since independence has been characterised by periods of significant economic and military growth as well as those of political and economic instability. It is an ethnically and linguistically diverse country, with similarly diverse geography and wildlife.
The healthcare delivery system of Pakistan is complex because it includes healthcare subsystems by federal governments and provincial governments competing with formal and informal private sector healthcare systems. Healthcare is delivered mainly through vertically managed disease-specific mechanisms. The different institutions that are responsible for this include: provincial and district health departments, parastatal organizations, social security institutions, non-governmental organizations (NGOs) and private sector. The country’s health sector is also marked by urban-rural disparities in healthcare delivery and an imbalance in the health workforce, with insufficient health managers, nurses, paramedics and skilled birth attendants in the peripheral areas. Pakistan’s gross national income per capita in 2021 was $4,990 and the total expenditure on health per capita in 2021 was Rs 657.2 Billion, constituting 1.4% of the country’s GDP. The health care delivery system in Pakistan consists of public and private sectors. Under the constitution, health is primarily responsibility of the provincial government, except in the federally administered areas. Health care delivery has traditionally been jointly administered by the federal and provincial governments with districts mainly responsible for implementation. Service delivery is being organized through preventive, promotive, curative and rehabilitative services. The curative and rehabilitative services are being provided mainly at the secondary and tertiary care facilities. Preventive and promotive services, on the other hand, are mainly provided through various national programs; and community health workers’ interfacing with the communities through primary healthcare facilities and outreach activities. The state provides healthcare through a three-tiered healthcare delivery system and a range of public health interventions. Some government/ semi government organizations like the armed forces, Sui Gas, WAPDA, Railways, Fauji Foundation, Employees Social Security Institution and NUST provide health service to their employees and their dependents through their own system, however, these collectively cover about 10% of the population. The private health sector constitutes a diverse group of doctors, nurses, pharmacists, traditional healers, drug vendors, as well as laboratory technicians, shopkeepers and unqualified practitioners.
Source:https://en.wikipedia.org/wiki/Pakistan
- GLOBAL PRETERM BIRTH RATES – Pakistan
- Estimated # of preterm births: 14.3 per 100 live births
- (USA 9.56-Global Average: 10.6)
- Source- WHO 2023- https://ptb.srhr.org/https://www.who.int/news/item/06-10-2023-1-in-10-babies-worldwide-are-born-early–with-major-impacts-on-health-and-survival

COMMUNITY
AKU neonatologists contribute to Pakistan guidelines for newborn care
Healthcare workers being trained across the country
Nov 20, 2023
Eight faculty members from Aga Khan University out of a total of 55 national and international neonatologists have contributed to the 352-page first National Guidelines for Small and Sick Newborn Care at Primary and Secondary Healthcare Facilities in Pakistan.
Ten percent of neonatal deaths globally take place in Pakistan. The guidelines will be used to train primary and secondary healthcare workers, paediatricians and neonatologists in Pakistan with the goal of lowering these mortality rates.
“Ten percent of neonatal deaths globally take place in Pakistan.”
The guidelines were the initiative of Pakistan’s Ministry of National Health Services, Regulations & Coordination, and have been supported by the Neonatology Group of Pakistan Pediatric Association (PPA), UNICEF, Pakistan and WHO, Pakistan.
Prof Sabina Durrani, the director-general of the Population Program Wing at the Ministry of National Health Services, Regulations and Coordination, Pakistan has said that these guidelines will be disseminated at and followed in all primary and secondary level healthcare facilities in Pakistan which will contribute to the achievement of SDG 3.2. The high rate of preterm babies and slow decline in neonatal mortality are key concerns towards achieving SDG 3.2. The major proportion of our neonatal mortality is from primary or secondary healthcare facilities.
AKU’s Dr Muhammad Sohail Salat led the effort from Sindh and his concerted follow-up with the team and his commitment to the project have resulted in these much-needed guidelines. From Aga Khan University these are the contributing authors:
- Distinguished Professor Zulfiqar A. Bhutta
- Associate Professor of Paediatrics Muhammad Sohail Salat
- Associate Professor of Paediatrics Khalil Ahmad
- Assistant Professor of Paediatrics Ali Shabbir Hussain
- Assistant Professor of Paediatrics Adnan Mirza
- Assistant Professor of Paediatrics Muhammad Hussain Shah
- Assistant Professor of Paediatrics Vinod Kumar
- Senior Instructor & Neonatologist Waqar Hussain Khawaja
The manual provides national standards and protocols to guide clinicians, administrators and teams working across maternity and neonatal services. These guidelines will standardize the development of neonatal units at secondary level hospitals and quality management of small and sick newborns in them.
The chapters include guidance on setting up a neonatal unit at a secondary level healthcare facility. The guidelines even specify dress codes, effective handwashing in Neonatal Units, hands-on techniques of Neonatal Resuscitation and Neonatal Transport.
These guidelines will be updated every two to three years. Work started in May-June 2022 and the book was published by July 2023. Over 100 trainers have been trained so far (Nov 2023) with pre- and post-workshop testing. The three-day sessions are divided into covering Neonatal resuscitation, Essential newborn care, Prevention of infections, Neonatal transport, Oxygen therapy, NIV, nHFT, nCPAP, CMV, Approach to respiratory failure. Workshops on Non-Invasive Ventilation, Kangaroo Mother Care and Neonatal Resuscitation have been held.
The guidelines have been edited by Prof. Khalid N. Haque, Visiting Professor of Neonatal Medicine, University of Child Health Sciences, The Children’s Hospital, Lahore, Former Professor and Reader in Neonatal Medicine, University of London, Consultant Neonatologist, Director of Research and Development, Epsom & St Helier University Hospitals Trust, London, UK.
Dr Muhammad Sohail Salat commented, “We are hopeful that the guidelines and effective training will serve to standardise the quality and level of new-born care in primary and secondary healthcare facilities across the country.”
Strengthening neonatal and obstetric healthcare in the war-affected regions of Ukraine (October 2023)

By Milena Chodola and Dorota Zadroga – October 02, 2023
For 12 months, the Polish Medical Mission conducted a program in Ukrainian neonatology hospitals aimed at improving the standard of maternal and newborn care, training medical personnel in European standards and the latest national guidelines for patient care, including in wartime conditions.
Within the framework of the project “Strengthening neonatal and obstetric healthcare in the war-affected regions of Ukraine” which lasted from September 2022 to the end of August 2023, the Polish Medical Mission equipped neonatal intensive care units in 10 hospitals in Ukraine with specialized medical equipment – neonatal resuscitation stations, patient monitors and dual-syringe infusion pumps. The project was implemented in hospitals in the following cities: Kyiv, Dnipro, Chernihiv, Kharkiv, Chernivtsi, Zaporizhzhia, Poltava and Lviv. In its implementation, the Polish Medical Mission cooperated with the Association of Neonatologists of Ukraine, the Ukrainian NGO “Early Birds,” the National Health Service of Ukraine and the Ministry of Health of Ukraine.
At each of the 10 hospitals, PMM conducted monthly in-person sessions for patients to raise their awareness about patient rights, newborn care and caring for well-being, supplemented by regular online sessions. These sessions also discussed changes in the operation of hospitals and medical services due to the war in Ukraine, available medical packages within the National Health Service of Ukraine, and options for psychological support. Patients admitted that, despite sometimes being in the hospital for several weeks, they often had no knowledge of how the National Health Service of Ukraine’s packages functioned, how to be treated at the state’s expense, and their rights and options for psychological support. Doctors from 10 project hospitals also participated in training sessions on patient rights in Ukraine. At these trainings, doctors also learned about the issue of patient rights in the European Union. This is an important issue for Ukrainian hospitals in the context of Ukraine’s introduction of more EU solutions and practices into the Ukrainian system on the way to receiving membership in the European Union. Medical staff from the 10 participating hospitals were also trained in doctor-patient communication, including under wartime conditions. The trainings also included recommendations on the well-being of medical personnel, counteracting professional burnout and maintaining a work-life balance. The training and session program on patient rights were supervised and coordinated by patient rights experts Oleksandra Balyasna and Yevgeniya Kubakh.
As part of the strengthening of professional competence, the medical staff of the aforementioned hospitals took part in four-day in-person medical training courses on neonatal intensive care, post-intensive care and various perinatal problems of newborns and premature infants, among others. The training program was developed on the basis of European neonatal treatment standards, the latest international research, but also on the basis of the latest national clinical guidelines, and is designed to update and expand doctors’ knowledge and promote good practice in Ukraine. During the medical training sessions at each hospital, the trainers, together with the medical staff, discussed and tried to work out solutions to the current challenges of a particular hospital – concerning both difficult clinical cases at a particular hospital and working under wartime conditions. The medical training program as well as its coordination in hospitals was supervised by medical experts, Prof. Tetiana Znamenska and Prof. Olga Vorobiova. At the beginning and end of the training, the doctors filled out anonymous knowledge tests – the results show that about 95% of the participating doctors increased their level of knowledge in the topics covered in the trainings.
During monitoring visits that the trainers conducted several months after the training, they undertook to identify problems that may have gone undetected during medical training, and reassessed the level of doctors’ knowledge using a test of the knowledge gained during medical training. The trainers also analyzed in detail the work of neonatology departments in terms of adherence to national guidelines, international recommendations and clinical protocols, reviewed department reports with indicators and statistics (number of patients, morbidity, mortality, length of stay in hospitals), and assessed the quality of neonatal care, including premature and sick newborns. They also discussed the organization of primary and specialized care, taking into account the conditions of individual hospitals. On the basis of this detailed analysis and audit, the trainers jointly gave a rating to each hospital and made recommendations for further professional development of doctors and for improving the operation of hospitals under wartime conditions (preserving the availability and continuity of care for newborns and pregnant and post-partum women). After summarizing and approving the results of the assessment, the medical trainers, together with the staff of the hospital in question, developed an action plan for the hospitals and individual departments (including neonatal intensive and post-intensive care, labor and delivery, and postpartum). Each hospital received an individually prepared plan.
Hospital administration representatives from 10 facilities indicated in their reports after medical monitoring that the project’s activities helped ensure the necessary standards of patient care and reduce mortality in the unit during the reporting period. For example, at a hospital in Poltava, mortality in the neonatal intensive care unit decreased by 5.8 times during the reporting period. In one hospital in Dnipro, on the other hand, the mortality rate and treatment time in the neonatal intensive care unit decreased almost 2 times during the reporting period. At a hospital in Chernihiv, morbidity and mortality among premature babies in the neonatal intensive care unit decreased thanks to modern medical equipment received under the project – the morbidity rate fell by 8%, and the mortality rate fell by 5%.
In an effort to reach a larger audience, including those outside the 10 participating hospitals, on the Ukrainian medical online platform the Polish Medical Mission published a comprehensive course on patient rights, doctor-patient communication and preventing professional burnout for medical professionals, as well as a webinar on patient rights, well-being and neonatal care for patients from across Ukraine. Prominent Ukrainian experts were invited to participate in these events, including the head of the National Health Service of Ukraine, who spoke about available neonatology and obstetrics services during the war. It will also be used in the next year of the ongoing second edition of the project to support neonatology in 10 more hospitals in new locations in Ukraine.
Key statistics of the project:
– 1,717 female patients attended sessions conducted in 10 hospitals in both in-person and online formats, as well as a webinar for female patients from across Ukraine.
– 78 stationary awareness-raising sessions for female patients on patient rights, newborn care, doctor-patient communication, changes in the functioning of hospitals and medical services due to the war in Ukraine, and opportunities for psychological support.
– 2578 newborns had benefited from medical equipment purchased under the project by the end of August.
– 346 doctors from the 10 hospitals participating in the project took part in medical training, and 160 in training on patient rights.
– 995 doctors from across Ukraine took a course on patient rights registered with the Ministry of Health of Ukraine, conducted online on a Ukrainian medical platform, passed the test, received a certificate and credits from the Ministry of Health of Ukraine.
– During medical monitoring, 94.42% of medical professionals trained at medical training courses showed improvement in patient care.
– 8 live online trainings on patient rights, doctor-patient communication and preventing professional burnout for medical workers from 10 hospitals. They were attended by 160 health workers.
– 10 individual plans were developed to improve the operation of hospitals and individual departments under wartime conditions.
– 1 live webinar on the popular Ukrainian medical platform Medvoice for patients from across Ukraine.

A nonprofit is racing to get its portable baby incubators into Israel and Gaza as crisis deepens
By Parija Kavilanz, CNN – October 27, 2023
New York CNN —
Jane Chen is racing against the clock, again. She knows well how every minute that passes is crucial for a new life that emerges prematurely into the world in the most vulnerable of circumstances — in the midst of war, in the aftermath of a natural disaster or in a remote village far away from a medical center.
Acutely aware of the deepening crisis between Israel and Gaza, Chen is mobilizing her team at Embrace Global, a nonprofit she co-founded to help save babies’ lives, in a way that’s become second nature to her.
Embrace, based in San Francisco, California, makes low-cost portable baby incubators that don’t require a stable electricity supply.
The Embrace incubator resembles a sleeping bag, but for a baby. It’s a three-part system consisting of an infant sleeping bag, a removable and reusable pouch filled with a wax-like phase-change material which maintains a constant temperature of 98 degrees F for up to eight hours at a stretch when heated, and a heater to reheat the pouch when it cools.
Chen said the pouch requires just a 30-minute charge to be fully ready for reuse. “This is really ideal for settings that have intermittent access to electricity, which is a lot of places where we work in the world,” she said.
According to the UN Population Fund (UNFPA), an estimated 50,000 pregnant women currently reside in Gaza, 5,500 of whom are due to give birth in the coming month.
The stats are startling to Chen, who is bracing for a swell of need there. She’s learned how access to incubators becomes critical in conflict areas through the organization’s efforts to donate 3,000 Embrace incubators with the help of UNICEF to doctors and hospitals in Ukraine where a war with Russia rages on. The nonprofit also sent the devices to Turkey and Syria after devastating earthquakes there earlier this year.
Medical experts point to elevated stress as a potentially serious factor that could trigger preterm deliveries in these situations.
“There’s been plenty of data that show stress not only causes preterm birth but also low-birth-weight,” said Dr. Veronica Gillispie-Bell, an obstetrician-gynecologist and associate professor with Ochsner Health in New Orleans, Louisiana
In general, babies born preterm or before 37 weeks, have difficulty maintaining their body temperature, said Bell. “Specifically, if we are speaking of disasters…. in my own experience of being here during [Hurricane] Katrina, in those very stressful situations, we have seen an uptick during those times in preterm birth and low birth weight,” she said.
Chen said the pouch requires just a 30-minute charge to be fully ready for reuse. “This is really ideal for settings that have intermittent access to electricity, which is a lot of places where we work in the world,” she said.
In general, babies born preterm or before 37 weeks, have difficulty maintaining their body temperature, said Bell. “Specifically, if we are speaking of disasters…. in my own experience of being here during [Hurricane] Katrina, in those very stressful situations, we have seen an uptick during those times in preterm birth and low birth weight,” she said.
Because preterm and low-birth-weight babies don’t have as much body fat, it’s harder for them to maintain their body temperature, which for a healthy baby is between 96.8 and 99.5 degrees F, she said. “The lower it is below that, the more oxygen and energy they need to stay warm. So they would have use even more energy.”
In both cases of preterm and low-birth-weight infants, quick and constant access to an incubator is vital.
From Ukraine to Gaza
In Ukraine, Chen said doctors have indicated that preterm births are on the rise across the country at the same time that intermittent power outages have made the use of conventional incubators very challenging. Several doctors and nurses, she said, also must consistently take babies and mothers to basement shelters as bombings continue.
Dr. Halyna Masiura, a general practitioner, is experiencing this first hand at the Berezivka Primary Healthcare Center in the Odesa region of Ukraine.
“Half of the babies being born in this area need more care,” Masiura told CNN. “They are being born early and with low birth weight. When air raids happen, we all have to go into shelters.” Masiura said her staff members have been relying on donated Embrace incubators for babies born with a birth weight of 2 kg (4 lbs.) and up.
In the Palestinian exclave of Gaza, Israel has instructed more than half of the more than 2 million residents in the north to evacuate to the southern region ahead of an anticipated ground operation in Gaza by the Israel Defense Forces (IDF) in response to Hamas’ deadly October 7 attack on Israel.
That attack killed more than 1,400 people.
In Gaza, where half of the overall population are children, access to medical aid, food, water, fuel, electricity and other normal daily necessities of life have evaporated in recent days amid sustained Israeli bombardment.
Over the weekend, after days of a complete siege of the exclave by Israel, the first trucks reported to be carrying medicine and medical supplies, food and water entered Gaza on Saturday.
For Chen, the most pressing problem is to figure out how to get the incubators to where they are most needed on the ground there. “As we did for Ukraine, we’re looking for partnerships with organizations that can get into the region effectively and also for funding,” she said. As a nonprofit, Chen said donations are sought through GoFundMe and a mix of individual donors, foundations and corporate donations.
Her team is working on a partnership with a humanitarian relief organization to respond in Gaza. “We’re also reaching out to organizations in Israel to assess the need for our incubators there,” she added.
A couple of hundred incubators are ready to immediately be sent to Israel and Gaza. Said Chen, “Depending on the need, we would go into production for more. But the big question is, can we get into those areas? We don’t want to ship products and then have them sit there.”
From a classroom idea to real-world solution
Linus Liang, along with Chen, was among the original team of graduate students at Stanford University who, as part of a class assignment in 2007, were given a challenge to develop a low-cost infant incubator for use in developing countries.
Liang, a software engineer who had already created and sold two gaming companies by then, was intrigued. “This class deliberately brought together people from different disciplines – law, business, medical school, engineers – to collaborate to solve world problems,” he said.
“Our challenge was that about 20 million premature and low-birth-weight babies are born globally every year,” he said. “Many of them don’t survive, or if they do, they live with terrible health conditions.”
The reasons why came down to factors such as a shortage of expensive conventional incubators or families living far away from medical centers to access quickly for their newborns.
The team formed their company in 2008 and then took a few years to engineer and produce the solution, with Liang and Chen both moving to India for a few years to get it off the ground and market test it there. Chen said the incubators, made in India, underwent rigorous testing and are CE certified, a regulatory standard that a device must meet to be approved for use in the European market and in Asia and Africa.
“We chose that route instead of seeking FDA approval because the need really is outside of the US,” said Liang. The cost per incubator is about $500, including cost of the product, training, distribution, shipping, implementation, monitoring and evaluation, said Chen. That compares to as much as $30,000 or more per conventional incubators, she said.
Chen estimates some 15,000 babies benefited from Embrace incubators in 2022.
Not just wars
Dr. Leah Seaman has been using Embrace incubators for three years in Zambia. Seaman is a doctor working in pediatrics for the last 12 years, including six years focusing on neonatal care at the Kapiri Mposhi District Hospital in the Central Province of Zambia.
Seaman has also been busy setting up a new specialized neonatal ward in the rural district hospital. “When I first came to Zambia, we had one old incubator that would draw a lot of power,” she said. “We often struggle with power cuts here, so even the voltage can be too low for the incubator to function well. Having enough space to set up conventional incubator was an issue as well.”
So she reached out to Chen in late 2020 after researching solutions that would work for the specific conditions in Zambia.
“In Zambia, 13% of births are premature, and that’s not even including low-birth-weight babies born at term,” she said. “We needed an effective solution.”
Embrace Global donated 15 incubators to the hospital. The new neonatal ward, set to open this month, is built around the Embrace incubator stations with Kangaroo mother care, or skin to skin contact between mother and baby.
“Last year we had 800 babies through the ward and maybe half of them used the Embrace incubator,” said Seaman. “This year we’ve had over 800 already. We haven’t asked for any conventional incubators because from 1 kg (2.2 lbs) and above, the Embrace incubator does the work.”
Because of their heavy use, Seaman said the main challenge with the incubators is making sure that the heating pad is kept warm and reheated in a timely manner. “We’ve built a mattress station where we will be teaching the new mothers how to do that,” she said.
“Why do we keep babies warm? It’s not just a nice thing. It literally does save lives,” Seaman said.
Source:https://www.cnn.com/2023/10/25/business/baby-incubators-israel-gaza/index.html
Asim Azhar & Shae Gill – Bulleya (Official Video)

5,017,656 views May 29, 2023 #Bulleya #AsimAzhar #ShaeGill
Asim Azhar & Shae Gill collaborates for the first time. Presenting the official video of “Bulleya” A song about peace, harmony & love 🤍🎶 This is definitely going straight into your daily travel playlist.


Why Infant Deaths are Rising in 2023

For the first time in two decades, infant mortality is on the rise in the United States. The nation already struggles with a higher infant mortality rate than many other developed countries. Moreover, like other countries, the United States has recently charted higher rates of low birthweight and preterm births. Nevertheless, new data from the CDC clearly illustrate the factors driving infant deaths – and give powerful clues about how to prevent them. Infant Mortality Data:
Between 2021 and 2022, the United States saw a 3% climb in its infant mortality rate. That raises infant fatalities to 5.6 per 1,000 live births. In a nation that welcomes 3.7 million babies each year, this means that more than 18,000 newborn lives were lost last year.
Babies of color face a higher risk of death:
A Black infant born in America is about twice as likely as a white infant to die in the first year of life. Native American infants and babies born before 37 weeks of gestation experienced the starkest change in mortality over the past few years.
Reversing the Trend:
The CDC cites two primary causes of infant mortality: maternal complications and bacterial meningitis. However, the “cause of death” alone paints an incomplete picture. The factors driving changes in infant survival, especially the disparities in maternal and infant health, are complex and multifaceted.
Consider that Black, Alaskan Native, Native Hawaiian, and Native American women are far more likely than white women to face fetal death, preterm births, stillbirths, and low-birthweight babies. These same groups have higher rates of pregnancies for which they receive no prenatal care and have higher incidences of maternal mortality.
The trend suggests that lack of access to adequate prenatal care and interventions contributes to the rise in infant deaths. The COVID-19 pandemic, which reduced hospital visits and led some clinics to close, also deepened healthcare inequalities.
Better access to care could not only save infants but also reduce pregnancy-related maternal death.
Reducing infant mortality, therefore, will require targeted policy interventions. Policymakers, healthcare professionals, and communities can unite around policy initiatives that bolster maternal and prenatal health services and education.
One example is the Black Maternal Health Momnibus Act of 2023, which aims to address the maternal health crisis in the United States. The legislation provides critical funding to address social determinants of health, enhance data collection processes, improve access to maternal mental health care, and promote maternal vaccinations to protect the health of moms and their babies.
All expectant mothers, regardless of their demographic background, should have access to timely and comprehensive prenatal care. By prioritizing maternal health care and addressing disparities in access, policymakers, advocates, and providers can work toward a healthier, more equitable future for mothers and babies alike”.
Source:https://neonatologytoday.net/newsletters/nt-dec23.pdf

HEALTHCARE PARTNERS

Cardiac Corner: Critical Physiological Principles when Caring for Babies with Congenital Heart Diseases

Gil Wernovsky, MD; Benjamin Hopkins, OMSIV (Discussant)
In this month’s edition of Cardiac Corner, I would like to discuss some critical physiological principles necessary for all those caring for babies with congenital heart disease. There are three broad concepts which determine chamber and great artery pressures, as well as direction of shunting
• A hole of any significant size equalizes the pressure on both sides of the hole.
• “Holes” equalize pressure, but do not determine the direction of shunting 1. Blood rolls “downhill”.
• The differences in the vascular resistance determine the direction of shunting 2. Blue is better than gray.
• A “low” oxygen saturation with normal cardiac output typically results in improved oxygen delivery than a “normal” oxygen saturation with low systemic blood flow
Let me get into this distinction in more detail. It is not uncommon at the bedside to confuse the crucial distinctions between pressure and resistance. When discussing “holes” such as atrial septal defects, ventricular septal defects, patent ductus arteriosus, and AP window, etc., it is essential to remember that the pressures are equal on either side of the hole, particularly at the ventricular and great vessel levels. Therefore, it is also vital to understand the strict definition of pulmonary hypertension: a mean pressure in the pulmonary artery greater than 25 mmHg. Thus, in all patients with a large VSD and with a large patent ductus arteriosus, the pulmonary artery pressure is at the systemic level. Thus, there is “pulmonary hypertension.” I will get into this in more detail below
The second rule, blood rolls downhill, involves resistance, not pressure. For example, in a baby with a ventricular septal defect, blood will shunt, in most situations, from the left ventricle to the low-resistance pulmonary circuit via the right ventricle. This results in a left to right shunt, pulmonary congestion, and no hypoxemia. If pulmonary vascular resistance is high, or there is an obstruction to pulmonary blood flow, as in Tetralogy of Fallot, blood may go from the right ventricle to the left ventricle, where there is less resistance to flow.
Number three, “blue is better than gray,” is the physiologic principle most frequently quoted when discussing complex physiology with my NICU colleagues. By that, we mean that the delivery of oxygen, is more important than the oxygen saturation via pulse oximetry (which, of course, is the percent of hemoglobin, which is bound to oxygen). Indeed, if cardiac output is normal and carrying capacity (hemoglobin) is normal, oxygen saturations in the 60s and 70s, even if sustained, will not result in tissue ischemia, metabolic acidosis, or, importantly, neurologic injury. It is beyond the scope of this article to discuss all of the details of every congenital heart problem. Still, in general, not all oxygen saturations that are “higher” are “better.”
The next concept that I’d like to discuss is “shunting.” This, by convention in most NICUs, refers to shunting in only one direction, right to left, resulting in hypoxemia, and may be labeled “PPHN”. This can easily be determined by pulse oximetry. However, the degree of left-to-right shunting cannot be quantified at the bedside but may result in significant clinical illness.
I think of “shunting” associated with hypoxemia in two broad categories. The most common scenario in the NICU is interpulmonary shunting, where the blood returning from the pulmonary veins is not fully saturated; this is due to lung disease, pneumothorax, pleural effusion, atelectasis, etc. Intracardiac shunting, however, results in systemic hypoxemia due to systemic venous return bypassing the pulmonary circulation through an intracardiac or great vessel connection. So, in a hypoxemic newborn with congenital heart disease, it is important to distinguish systemic hypoxemia due to an intrapulmonary shunt, intracardiac shunt, or both.
Finally, “pulmonary hypertension” is a frequently misused term, and I wonder if we will ever get it out of our lexicon. In my world as a congenital cardiologist, pulmonary hypertension needs to be divided into two categories: pulmonary hypertension due to elevated pulmonary vascular resistance (such as seen in PPHN, diaphragmatic hernia, and meconium aspiration), and pulmonary hypertension due to the connection of the ventricles or the great vessels by “holes” (Rule #1), and differences in resistance (Rule #2). For example, echo reports may report “elevated right ventricular and pulmonary artery pressure,” which may be assumed by the bedside team that the pressure is elevated due to elevated resistance (“PPHN”), with institution of pulmonary vasodilation. However, it may also be due to Intracardiac or great vessel communications – a very important distinction for management.
As a parting comment, systemic hypoxemia without alveolar hypoxia does NOT cause an elevated pulmonary vascular resistance or “worse PPHN” – otherwise, all babies with intracardiac shunts from congenital heart disease would have elevated pulmonary vascular resistance! It is alveolar hypoxia which causes elevations in pulmonary vascular resistance, sometimes severe, and should be treated with usual ventilatory maneuvers, inhaled nitric oxide, ECMO, etc. If a baby has hypoxemia with no lung disease, increasing oxygen, non-invasive or invasive mechanical ventilation is likely to do more harm than good.
Source:https://childrensnational.org/visit/find-a-provider/gil-wernovsky

NICU Nurses Have ‘Something Special’ | Jan, 15, 2024 | News 19 This Morning

WHNT News 19 Jan 15, 2024
Do you believe in angels? What about miracles? Some say they’ve seen both in the Regional Neonatal Intensive Care Unit at Huntsville Hospital for Women and Children.

So Many Babies”: An interview with author and neonatologist Susan Landers, MD
Jul 8, 2023 #theartofmedicine #podcastsonamazonmusic
It’s a pleasure to welcome Susan Landers, MD, to The Art of Medicine with Dr. Andrew Wilner. Dr. Landers is a retired neonatologist and author of the memoir, “So Many Babies.” After four years of medical school, three years of pediatric residency, and three years of neonatology fellowship, Dr. Landers worked as a neonatologist for 34 years. She has many stories to tell! In “So Many Babies,” Dr. Landers tells the stories of many of her tiny patients and their distraught and devoted families. She also shares the challenges she faced as a full-time working Mom. Dr. Landers tried desperately to balance her dedication to her patients and academic career with the roles of wife and mother to three children. She learned that working full-time, producing scholarly publications, teaching medical students and residents, providing optimal patient care, and raising a family can be too much for one person to do simultaneously. The lessons she learned may help young physicians, nurses, and other career-minded professionals succeed in their careers and family life. You can find “So Many Babies” on Amazon and in my library.


PREEMIE FAMILY PARTNERS
How to support your premature child at school

The Smallest Things Jul 20, 2023
A webinar from The Smallest Things premature baby charity and the University of Leicester for parents and carers who want to help their prematurely born children at school. • Hear from leading academics including Professor Samantha Johnson on the latest research findings into educational needs and how schools can support premature children • Receive practical advice and resources to help you advocate for your child and ask their school to become Prem Aware • Watch teachers from Prem Aware schools explain why they took the three steps to achieve the Prem Aware Award and how it’s making a difference to their communities • Listen to an adult born prematurely and a parent of premature children talk about their experiences of the education system.


Lullaby-Playing Pacifier Helps Premature Babies Thrive | UCLA Health Newsroom
UCLA Health – Feb 11, 2019
Babies who are born premature often struggle with feeding and the reflex to suck, breathe and swallow, which is pivotal for their development. And when parents watch their premature newborns in the neonatal intensive care unit (NICU), they often feel helpless. Now, researchers with the music therapy program at UCLA Mattel Children’s Hospital are testing whether an unusual device, which plays a lullaby recorded by the baby’s parents when a baby successfully sucks on the connected pacifier, can empower parents by helping them bond with their babies — and strengthen the babies by improving their oral abilities, which play a crucial role in the ability to feed. A family with triplets participated in the research and used the pacifier-activated lullaby (PAL) device to aid in their babies’ development.

Seeking Local Parent /Patient support? EFCNI provides contact information for International and National Parent and Patient Organizations.

Parent and Patient Organisations

International Organizations
- INTERNATIONAL COUNCIL OF MULTIPLE BIRTH ORGANISATIONS / ICOMBO
- INTERNATIONAL FEDERATION OF SPINA BIFIDA AND HYDROCEPHALUS / IFSBH
- INTERNATIONAL PATIENT ORGANISTION FOR PRIMARY IMMUNODEFICIENCIES / IPOPI
- 57 Countries are listed with identified patient/parent organizations
ENTER HERE

Source:https://www.efcni.org/parent-and-patient-org-2/

Early body contact develops premature babies’ social skills
November 30, 2023 Karolinska Institutet

Summary:
Skin-to-skin contact between parent and infant during the first hours after a very premature birth helps develop the child’s social skills. The study also shows that fathers may play a more important role than previous research has shown.
Skin-to-skin contact between parent and infant during the first hours after a very premature birth helps develop the child’s social skills. This is according to a new study published in JAMA Network Open by researchers from Karolinska Institutet and others. The study also shows that fathers may play a more important role than previous research has shown.
In current practice, very premature babies are usually placed in an incubator to keep them warm and to stabilize them during the first hours after birth.
In the “Immediate parent-infant skin-to-skin study” (IPISTOSS), 91 premature babies born at 28 to 33 weeks were randomized to either traditional care in an incubator or immediate skin-to-skin contact with one of the parents.
The study has generated several results that show, among other things, that immediate skin-to-skin contact is safe for babies and beneficial for their cardiorespiratory stabilization and temperature maintenance, and that it is perceived as valuable by the parents.
Now, as part of this study, the researchers have also studied the social development at four months of age of 71 of these premature babies.
The children were randomly assigned to receive either standard care in an incubator or to receive care resting on one of their parents’ breasts, either the mother’s or the father’s, for the first six hours after birth.
“What is new about our study is that we also allowed the fathers to have skin-to-skin contact immediately after the birth. In most previous studies, it is the mother who is the primary caregiver, but in our study it was the fathers who had the most skin-to-skin contact,” says Wibke Jonas, midwife, senior lecturer and associate professor at Karolinska Institutet’s Department of Women’s and Children’s Health, as well as research leader and last author of the study.
“The study has identified fathers as a previously untapped resource that really has an important function in having immediate skin-to-skin contact with their infant if the mother is not available,” says Siri Lilliesköld, PhD student at the same department and specialist nurse in neonatal care, and first author of the study.
After four months, the social interaction between mother and infant was filmed and assessed by two psychologists who did not know which infant had received early skin-to-skin contact and which had not.
The quality of the interaction was measured according to the Parent-Child Early Relational Assessment (PCERA) scale, where different elements are graded between one and five, with one being cause for concern and five being very good quality.
The infants who received immediate skin-to-skin contact had significantly better results in a subscale measuring the infant’s communicative and social skills.
On the five-point scale, their average score was closer to four, while the infants cared for according to current practice were just above three.
“What you could see was that the infants in the skin-to-skin group had slightly better communication skills, they were a bit more social and happier,” says Wibke Jonas.
Premature babies have developmental challenges as they grow up and need a lot of support.
Even though medical developments have come a long way, the care of these babies still needs to be developed, the researchers say.
“If we combine the immediate medical care of the very premature babies with a relatively simple intervention such as skin-to-skin contact, it has effects on the infants social skills,” says Jonas Wibke and continues.
“Previous studies have shown that premature babies perform slightly poorer when socially interacting, for example, they do not give as clear signals in the interaction with their mothers. The closeness between babies and their parents at birth may therefore stimulate later interaction and thus the development of the infant.”
The benefits of immediate skin-to-skin contact are so clear that both Wibke Jonas and Siri Lilliesköld believe it should be introduced now in Swedish neonatal care.
And this work is already underway, they say.
‘We have worked very actively to minimize separation between infants and parents in general, and now we have the evidence to do the same with these very premature babies,” says Siri Lilliesköld.
The research team will continue to report on the development of the infants at 12 and 24 months.
The study is a collaboration between researchers from Karolinska Institutet and the University Hospital of Stavanger, Norway, and the University of Turku, Finland. The research was funded by, among others, the Swedish Research Council, Region Stockholm and Stiftelsen Barnavård. The researchers declare that there are no conflicts of interest.
Source:https://www.sciencedaily.com/releases/2023/11/231130113047.htm

INNOVATIONS

Two-Year Autism Risk Screening and 3-Year Developmental Outcomes in Very Preterm Infants
Coral L. Shuster, PhD1; Stephen J. Sheinkopf, PhD2; Elisabeth C. McGowan, MD1,3; et alJulie A. Hofheimer, PhD4; T. Michael O’Shea, MD4; Brian S. Carter, MD5; Jennifer B. Helderman, MD, MS6; Jennifer Check, MD6; Charles R. Neal, MD, PhD7; Steven L. Pastyrnak, PhD8; Lynne M. Smith, MD9; Cynthia Loncar, PhD3; Lynne M. Dansereau, MSPH1; Sheri A. DellaGrotta, MPH1; Carmen J. Marsit, PhD10; Barry M. Lester, PhD1,3
Key Points
Question How are screening examinations using a 2-stage parent-report autism risk screening tool at 2 years of age associated with 3-year developmental and behavioral outcomes among infants born very preterm?
Findings In this longitudinal cohort study of 467 infants born less than 30 weeks’ gestation, children who screened positive on the 2-stage parent-report autism risk screening tool at age 2 years were significantly more likely to have cognitive, language, and motor delay as well as internalizing, externalizing, and autism-related behavior problems at age 3 years.
Meaning Study results suggest use of the 2-stage parent-report autism risk screening tool for behavior problems and overall developmental delays for infants born very preterm, regardless of future autism diagnosis.
Abstract
Importance Use of the Modified Checklist for Autism in Toddlers, Revised With Follow-Up, a 2-stage parent-report autism risk screening tool, has been questioned due to reports of poor sensitivity and specificity. How this measure captures developmental delays for very preterm infants may provide support for continued use in pediatric care settings.
Objective To determine whether autism risk screening with the 2-stage parent-report autism risk screening tool at age 2 years is associated with behavioral and developmental outcomes at age 3 in very preterm infants.
Design, Setting, and Participants Neonatal Neurobehavior and Outcomes for Very Preterm Infants was a longitudinal, multisite cohort study. Enrollment occurred April 2014 to June 2016, and analyses were conducted from November 2022 to May 2023. Data were collected across 9 university-affiliated neonatal intensive care units (NICUs). Inclusion criteria were infants born less than 30 weeks’ gestational age, a parent who could read and speak English and/or Spanish, and residence within 3 hours of the NICU and follow-up clinic.
Exposures Prematurity and use of the 2-stage parent-report autism risk screening tool at age 2 years.
Main Outcomes and Measures Outcomes include cognitive, language, motor composites on Bayley Scales for Infant and Toddler Development, third edition (Bayley-III) and internalizing, externalizing, total problems, and pervasive developmental disorder (PDD) subscale on the Child Behavior Checklist (CBCL) at age 3 years. Generalized estimating equations tested associations between the 2-stage parent-report autism risk screening tool and outcomes, adjusting for covariates.
Results A total of 467 children (mean [SD] gestational age, 27.1 [1.8] weeks; 243 male [52%]) were screened with the 2-stage parent-report autism risk screening tool at age 2 years, and outcome data at age 3 years were included in analyses. Mean (SD) maternal age at birth was 29 (6) years. A total of 51 children (10.9%) screened positive on the 2-stage parent-report autism risk screening tool at age 2 years. Children with positive screening results were more likely to have Bayley-III composites of 84 or less on cognitive (adjusted odds ratio [aOR], 4.03; 95% CI, 1.65-9.81), language (aOR, 5.38; 95% CI, 2.43-11.93), and motor (aOR, 4.74; 95% CI, 2.19-10.25) composites and more likely to have CBCL scores of 64 or higher on internalizing (aOR, 4.83; 95% CI, 1.88-12.44), externalizing (aOR, 2.69; 95% CI, 1.09-6.61), and PDD (aOR, 3.77; 95% CI, 1.72-8.28) scales.
Conclusions and Relevance Results suggest that the 2-stage parent-report autism risk screening tool administered at age 2 years was a meaningful screen for developmental delays in very preterm infants, with serious delays detected at age 3 years.
Source:https://jamanetwork.com/journals/jamapediatrics/article-abstract/2812810

Quality of inpatient care of small and sick newborns in Pakistan: perceptions of key stakeholders
Nousheen Akber Pradhan, Ammarah Ali, Sana Roujani, Sumera Aziz Ali, Samia Rizwan, Sarah Saleem, Sameen Siddiqi
Abstract
Background
In LMICs including Pakistan, neonatal health and survival is a critical challenge, and therefore improving the quality of facility-based newborn care services is instrumental in averting newborn mortality. This paper presents the perceptions of the key stakeholders in the public sector to explore factors influencing the care of small and sick newborns and young infants in inpatient care settings across Pakistan.
Methods
This exploratory study was part of a larger study assessing the situation of newborn and young infant in-patient care provided across all four provinces and administrative regions of Pakistan. We conducted 43 interviews. Thirty interviews were conducted with the public sector health care providers involved in newborn and young infant care and 13 interviews were carried out with health planners and managers working at the provincial level. A semi-structured interview guide was used to explore participants’ perspectives on enablers and barriers to the quality of care provided to small and sick newborns at the facility level. The interviews were manually analyzed using thematic content analysis.
Findings
The study respondents identified multiple barriers contributing to the poor quality of small and sick newborn care at inpatient care settings. This includes an absence of neonatal care standards, inadequate infrastructure and equipment for the care of small and sick newborns, deficient workforce for neonatal case management, inadequate thermal care management for newborns, inadequate referral system, absence of multidisciplinary approach in neonatal case management and need to institute strong monitoring system to prevent neonatal deaths and stillbirths. The only potential enabling factor was the improved federal and provincial oversight for reproductive, maternal, and newborn care.
Conclusion
This qualitative study was insightful in identifying the challenges that influence the quality of inpatient care for small and sick newborns and the resources needed to fix these. There is a need to equip Sick Newborn Care Units with needed supplies, equipment and medicines, deployment of specialist staff, strengthening of in-service training and staff supervision, liaison with the neonatal experts in customizing neonatal care guidelines for inpatient care settings and to inculcate the culture for inter-disciplinary team meetings at inpatient care settings across the country.
Source:https://bmcpediatr.biomedcentral.com/articles/10.1186/s12887-021-02850-6

Seven simple innovations that could save the lives of two million pregnant women and babies

MATERNAL HEALTH – BEATRIZ LECUMBERRIPATRICIA R. BLANCO– Madrid – SEP 13, 2023
A study by the Bill and Melinda Gates Foundation states that the world is experiencing an epidemic of maternal and child mortality
Seven medical innovations or treatments, most of them inexpensive and easy to implement, could significantly reduce maternal and infant deaths around the world, particularly in sub-Saharan Africa and South Asia. This is the conclusion of the 2023 Goalkeepers Report published by the Bill and Melinda Gates Foundation this Tuesday. “By making new innovations accessible to those who need them most, 2 million additional lives could be saved by 2030 — and 6.4 million lives by 2040,” estimates the philanthropic organization in its annual report, which focuses on maternal and child mortality, whose progress has become stagnant since 2016 and even increased in some countries, including the United States.
Among these innovations are the rapid diagnosis of postpartum hemorrhage, an intravenous infusion of iron against anemia, a probiotic supplement for babies, antenatal corticosteroids (anti-inflammatories) for women who will give birth prematurely, azithromycin (an antibiotic) to prevent infections, and an AI-enabled ultrasound device to monitor high-risk patients in low-resource places.
In 2015, world leaders agreed on 17 Sustainable Development Goals with an eye toward 2030. The year 2023 marks the halfway point to achieving those goals and, in the case of maternal, child and neonatal mortality, the data indicate that there is still a long way to go. The goal was to end all preventable child deaths by 2030 and reduce maternal mortality to 70 out of every 100,000 births, but that has not happened. Every day, 800 women around the world die from reasons related to pregnancy and childbirth. That is, one every two minutes. According to the UN, 70% of these deaths occur in sub-Saharan Africa. In addition, every year approximately five million children die before their fifth birthday, and nearly two million more are stillborn.
This happens despite the fact that there has never been so much scientific knowledge on maternal and child health: “Researchers have learned more about the health of mothers and babies over the past 10 years than they did in the century before that,” the report states. The problem is that the solutions do not reach those who need them most. The authors even speak of an “epidemic” of maternal and child mortality, and not only in low-income countries: in the United States, for instance, mortality among Black mothers has doubled since 1999. “American women are more than three times more likely to die from childbirth than women in almost every other wealthy country. But, as I noted earlier, the biggest crisis is among Black and Indigenous women,” writes Melinda French Gates.
In the 2000s, indicators of human well-being such as poverty or education improved substantially, and it was precisely maternal and child health what made the most progress. This was possible, in part, because several international organizations had set ambitious goals; these, however, were curtailed after 2016 and ended up stagnating with the arrival of the Covid-19 pandemic. In some countries, like Venezuela or the United States, the situation has even worsened, according to the report.
Three low-cost lifesavers
According to Melinda French Gates, three inexpensive innovations can prevent thousands of women in low- and middle-income countries from dying during pregnancy and childbirth: a new treatment for postpartum hemorrhage, the use of the antibiotic azithromycin to prevent infections, and intravenous infusions of iron for cases of anemia.
Postpartum hemorrhage (PPH), which occurs when a woman loses more than half a liter of blood within 24 hours of childbirth, is the number one cause of maternal death. The World Health Organization (WHO) estimates that it affects 14 million women a year, killing 70,000, particularly in low-income countries. In impoverished countries, the main problem is realizing that a significant loss of blood is taking place. In many places this is only estimated visually, and thousands of women die without receiving the treatment that could save them.
The Gates Foundation proposes a simple, low-cost way to assess this blood loss: a calibrated obstetric drape that looks like a V-shaped plastic bag, which is hung on the edge of the patient’s bed so the blood falls into it and rises like the mercury in a thermometer. That is a quick visual gauge that can alert healthcare personnel in time. Furthermore, instead of sequentially applying the five treatments to stop bleeding (uterine massage, oxytocic drugs, tranexamic acid, IV fluids and genital-tract examination), they propose grouping them all together. In a study called E-MOTIVE, Nigerian obstetrician-gynecologist Hadiza Galadanci and a team of researchers from four African countries with a high maternal mortality rate found that using the drapes and following the updated guidelines managed to decrease cases of severe bleeding by a remarkable 60%.
Another of the proposed changes is the treatment of anemia, which affects 37% of pregnant women (although in some areas of the world, such as South Asia, it can go up to 80%) and increases the chances of hemorrhage during childbirth. Diagnosing it during pregnancy is essential, but instead of treating it with oral iron supplements that must be taken for 180 days, Bosede Afolabi, a Nigerian obstetrician and researcher, is working to implement a promising new intervention in her country: a single intravenous infusion of iron that takes 15 minutes and can replenish a woman’s iron reserves during pregnancy.
Another of the main causes of maternal mortality is infection. In recent years, researchers have discovered that one of the most promising new ways to prevent infections during pregnancy is one of the most used antibiotics in the world: azithromycin. In a trial carried out in sub-Saharan Africa, it reduced cases of sepsis (an extreme inflammatory reaction) by one third.
“These breakthroughs aren’t silver bullets on their own — they require countries to keep recruiting, training, and fairly compensating health care workers, especially midwives, and building more resilient health care systems. But together, they can save the lives of thousands of women every year,” reflects Melinda French Gates.
The baby knowledge boom
“Over the past decade, the field of child health has moved faster and farther than I thought I’d see in my lifetime,” writes Bill Gates, highlighting the launch of three Gates Foundation programs to carry out research on the deaths of children and newborns, in order to prevent them: CHAMPS (Child Health and Mortality Prevention Surveillance); PERCH, which analyzes the causes of childhood pneumonia; and GEMS, for diarrheal diseases.
Ten years ago, he explains, “any record of a child’s death would generally list one of the four most common causes: diarrhea, malnutrition, pneumonia, or premature birth.” However, he continues, “each was a vast ocean of different illnesses, with scores of different causes and cures. Pneumonia, for example, is linked to more than 200 types of pathogens.”
The collection of data carried out in recent years — taking blood and tissue samples from children who had died and comparing cases — has revealed that some pathogens were less likely than expected, such as the one that causes whooping cough, while others were more common, such as Klebsiella, which is more difficult to treat. The new information about this last bacteria “is leading doctors to change what antibiotics they use,” explains Bill Gates. This is what he refers to as the baby knowledge boom. “Thanks to studies like CHAMPS, GEMS and PERCH, the medical field has begun to understand precisely when and why some babies are dying, which allows them to keep others alive,” he stresses.
Another example that Gates highlights is how doctors help premature babies breathe by giving antenatal corticosteroids (ACS) to pregnant mothers who are going to give birth prematurely. According to the foundation’s calculations, “ACS could save the lives of 144,000 infants in sub-Saharan Africa and South Asia by 2030 and nearly 400,000 by 2040.” Probiotic supplements with bifidobacteria (bacteria that live in the digestive system and help break down milk sugars) also reduce the risk of death or serious illness in premature babies.


Unlocking Potential: The Early Stages of Preemie Education Programming – A Journey of Growth and Exploration
Every preemie represents a world of untapped potential, and preemie education programs are at the forefront of pioneering innovative approaches. These programs are breaking away from traditional teaching methods, placing a strong emphasis on adaptability and forward-thinking to cater to each child’s unique needs. Envision a classroom where lessons seamlessly blend with sensory experiences, social interactions, and progressive challenges. In an ideal learning/teaching environment education is far from a one-size-fits-all model; it’s a journey of individual resonance, finely tuned for every individual learner.
Within this promising new educational frontier targeting the needs and great potentialities of prematurely born children, and as research continues, we can anticipate the expansion of such programs over time. With increased understanding and ongoing innovation, we can look forward to the implementation of more of these tailored educational approaches, ensuring that every preemie has the opportunity to thrive and reach their full potential.
Preemie education programming isn’t a fanciful educational approach; it’s a pragmatic response to unique challenges. It signifies the resilience of preemies, the creative expertise of teachers, the importance of tailored learning, and a cooperative effort that benefits both learners, educators, and their support systems. Our education-focused journey is in its early stages, and the possibilities are vast, inviting our creativity, knowledge, and most of all, engagement.

Preemie Chat – Catriona Ogilvy – on January 14 at 1 pm EST
Following the successful introduction of the UK Prem Aware Award, helping teachers to support the needs of children born prematurely in school, this presentation will highlight the lasting journey and impact of premature birth, with a specific focus on education and learning. While being born premature does not mean that a child will have special educational needs, it does increase the chances. It is essential therefore that parents and teachers alike are aware of the potential difficulties and become equipped to meet these needs. This presentation will examine this topic and discuss what more we can do to support the long-term outcomes of children born early.
Preemie babies become capable adults when grown up, new study confirms

New research shows that extremely prematurely born adults are transitioning to adult life similarly to their term-born peers.22 DECEMBER 2023 RESEARCH AND CLINICAL TRIALS | NICU
New evidence from a world-leading Victorian study following premature babies into adulthood shows that babies born before 28 weeks’ gestation are doing surprisingly well as young adults in their twenties.
In a paper published in PEDIATRICS, new data released from the Victorian Infant Collaborative Study (VICS) 1991-92 cohort reveals insights from the 25-year point of the long-term study.
The study, co-led by the Royal Women’s Hospital and Murdoch Children’s Research Institute (MCRI), shows that extremely prematurely born adults are just as likely to have completed secondary school, be in paid work, and be in a romantic relationship, compared to their peers born at full term.
Dr Lauren Pigdon, Research Officer at MCRI, analysed the new data from the unique Australian geographic cohort who were recruited at birth and followed for 25 years.
“A strength of this study is that it represents the earliest survivors of the post-surfactant era to navigate the transition into adulthood and fills a gap in knowledge,” Dr Pigdon said.
The introduction of exogenous surfactant in the early 1990s was a game changer in treating respiratory distress syndrome in newborn intensive care. Since then, there has been a dramatic rise in survival of infants born extremely preterm (younger than 28 weeks’ gestation) or with extremely low birthweight (less than 1000g).
With increased survival rates of even the tiniest babies, concerns arose that these tiny babies might have increased chances of health and developmental problems as children and adults. And that this may in turn have an impact on their transition into adult life. But is this true?
Professor Jeanie Cheong, Consultant Neonatologist at the Women’s and Co-Group Leader of the Victorian Infant Brain Studies group at MCRI.
“Our data paints a positive and encouraging picture,” Dr Pigdon said. “There were minimal group differences in self-reported general interpersonal relationships, satisfaction with different aspects of life, and current smoking behaviour.”
However, Professor Jeanie Cheong, Consultant Neonatologist at the Women’s and Co-Group Leader of the Victorian Infant Brain Studies group at MCRI, said there were some differences between the groups.
“More adults born extremely preterm had their main income source from government financial assistance and more had not yet moved out of the parental home compared with their peers born full term,” Professor Cheong said.
“Data from the past 25 years has allowed us to look at how, over time, care has improved for Victoria’s youngest and most vulnerable patients,” Professor Cheong said.
“While survival rates have gone up, we now also know that these babies have the chance to become fully functional members of our society.
“Findings from our study are relevant when counselling families after their baby is born, to put into perspective what the long-term outcomes may mean for their child.”
Meet Duane:
Duane has certainly grown up since he was born extremely premature at 26 weeks’ gestation in March 1992. He weighed only 886 grams at birth.
“I was so tiny that my father’s wedding ring could fit all the way up my arm to my shoulder,” Duane remembers.
After a happy and normal childhood, Duane completed high school and became a competitive slalom skier, trying out for the Australian National Team. While he is an experienced downhill racer avoiding major obstacles, Duane faced a few health issues and injuries in his early 20s.
Duane is now a professional skiing and snowboard instructor. He follows the snow seasons and enjoys living and working abroad. He spent a long time in Austria, where he completed a sports diploma in Innsbruck, and now speaks German fluently.
Currently, Duane is keen for his torn ACL in the knee to heal. Then he plans to hit the slopes again and has offers to work in the USA, Japan, and Europe.


This Is The Way We Go To School By Edith Baer, Book Read Aloud, Book about Transportation

What are all the ways we can go to school around the WORLD, watch and find out! SUBSCRIBE for more books! This is another of D’s school books with FCA.

Surfing clubs at Mubarak Village Beach

Yasir Jawed Nov 25, 2022 MUBARAK VILLAGE BEACH
The coastal belt of Pakistan has one of the best beaches in the World. In today’s vlog, we are going to be surfing at Mubarak village beach. Surfing is a sport that is not popular in Pakistan like other water sports but there are people who love to surf in Pakistan, we will meet the surfing community of Rehman Goth @Surfers of Bulleji and another group resident of Mubarak Village. I’d like to appreciate the efforts and support of Dr. Aftab Ahmed Siddiqui who has been supporting the fishing community of Mubarak village he has provided them the equipment, accessories training to encourage them to do this sport. Moreover, I am thank full to Mr. Murtaza Sabir Ali for engaging me in such activities, I am sure the bond is getting stronger day by day. For me Surfing was entirely new but since I love water sports, it was a great experience for me. My son 9 years old and my friend Khalil also enjoyed the day by far. Special thanks to Team @shaharyarkhanvlogs & Team @PakistanwithFarhanAli because of the fellow content creators we had extreme fun. Thanks to @Atiq a professional surfer from Rehman Goth, I wish he becomes a star in the sports one day.

