Cyprus, officially the Republic of Cyprus, is an island country in the eastern Mediterranean Sea. Situated in West Asia, its cultural identity and geopolitical orientation are overwhelmingly Southeast European. Cyprus is the third largest and third most populous island in the Mediterranean, after Sicily and Sardinia. It is located southeast of Greece, south of Turkey, west of Syria and Lebanon, northwest of Israel and Palestine, and north of Egypt. Its capital and largest city is Nicosia. Cyprus hosts the British military bases Akrotiri and Dhekelia, whilst the northeast portion of the island is de facto governed by the self-declared Turkish Republic of Northern Cyprus, which is separated from the Republic of Cyprus by the United Nations Buffer Zone.
A universal national health system, known as GESY, was implemented in Cyprus in June 2019. The system was created as part of a requirement in the bail-out agreement with the International Monetary Fund, the European Commission and the European Central Bank (the Troika). The new system aims to provide affordable and effective medical care to all people residing permanently in Cyprus.
Source: https://en.wikipedia.org/wiki/Cyprus

COMMUNITY


The neonatal intensive care unit (NICU) is often seen through the eyes of mothers and clinicians, but another voice remains underrepresented: fathers. In June 2025, AngelEye Health hosted a national webinar bringing together NICU dads and clinicians to discuss fatherhood in the NICU. What emerged was honest, emotional, and long overdue. These fathers revealed that while the NICU centers around the fragile infant, it is also a crucible for shaping new fathers through fear, resilience, and love.
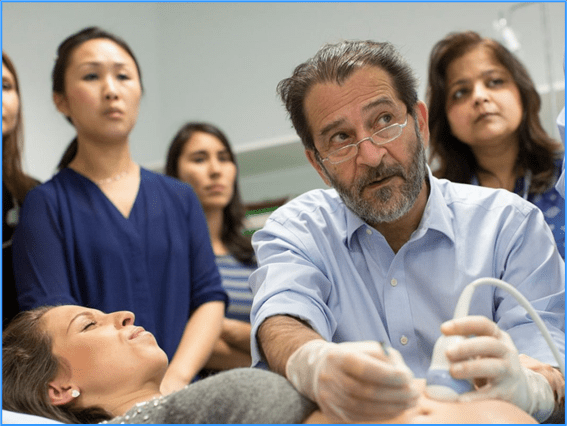
Meet the Facilitator:
Dr. Craig Garfield is a professor of pediatrics and a NICU hospitalist with over 25 years of experience caring for premature infants in an 85-bed Level III NICU. Dr. Garfield’s research focuses on understanding the role fathers play in the lives of families and elevating the voices of fathers in the healthcare system.
Meet the Dads:
Teo Muñoz became a first-time father while still in his early twenties. His son was admitted to the NICU following an emergency transfer during a complicated delivery at only 24 weeks and 2 days of gestation. Teo juggled hospital visits, work transitions, and supporting his fiancée during a NICU stay that lasted 128 days.
Jared Muscat and his wife experienced a premature birth of their son at only 24 weeks of gestation that led to a NICU stay of 97 days. With a background in healthcare advocacy and personal experience managing his epilepsy, Jared brought a thoughtful perspective on communication, peer support, and emotional resilience.
Adam Wood entered the NICU after a high-risk pregnancy and a traumatic delivery following IVF. His son required intensive support immediately after birth at 25 weeks of gestation. Overwhelmed and unprepared, Adam gradually found purpose in presence and routine throughout the 135-day journey.
Their stories reflected a broad range of emotions and circumstances, yet common themes emerged—ones that can inform how neonatal teams engage fathers moving forward.
Lesson 1: Dads Need to Be Seen—and Heard: As Teo reflected, “I was running upstairs to see my wife, downstairs to see the baby, back home to get things we forgot—we were still just kids ourselves.” NICU dads often carry invisible burdens as they work hard to try to keep things going for their partners. Many fathers report that they shoulder an increasing number of burdens to alleviate the burdens that fall on mothers. Their role is typically seen as secondary or supportive, yet they are equally affected. Many expressed feeling overlooked by both care teams and support systems, highlighting a need to engage fathers as partners in care intentionally—not just visitors or helpers, but as essential members of family-centered care who, like many mothers, are grieving the loss of a “normal” pregnancy.
Lesson 2: The Mental Health Toll Is Different—but Just as Deep: Dr. Garfield noted, “Our studies show that while maternal stress often decreases over time, paternal stress levels remain steady— because their needs are frequently unaddressed.” (1, 2) Several dads described post-traumatic stress symptoms and emotional suppression during their baby’s stay, only processing their experience months or even years later. As Teo shared, “I did not start talking about it until a week ago, when my son turned one.”
Lesson 3: Identity and Purpose Emerge from Chaos: Adam described his transformation: “I hadn’t finished the nursery. I hadn’t even finished reading the book (The Expectant Father). (3) But once I figured out how to help—whether it was delivering milk or simply being present, I started to feel like a dad.” Many echoed this shift: from feeling helpless to finding meaning through routine, presence, and celebrating small milestones.
Lesson 4: Fathers Want—and Need—Connection: Fathers found strength through connections with care teams and with one another. Jared shared how he found a dad whose twins shared the same pod as him and his wife, and they committed to meeting up each Thursday night after they both finished their skin to-skin time. “We built a routine and stuck to it. After visiting our sons each night, we’d go out together just to talk—even if it wasn’t about the NICU.” Whether through structured peer groups or informal moments of release and connection, relational touchpoints proved vital to their emotional survival.
Lesson 5: Communication Matters—Even When It Is Hard: Fathers stressed the importance of being included in updates and decision-making. Medical jargon, even when simplified, could still feel overwhelming. Jared noted, “They kept using grams and kilograms—I started doing my own math to stay involved.” Humor and engagement became bridges for understanding and partnership.
Practical Insights from NICU Dads In follow-up reflections, both Adam Wood and Teo Muñoz offered practical guidance for clinicians working with fathers in the NICU. Their combined perspectives provide actionable strategies that underscore the importance of presence, effective communication, and emotional attunement.
For Physicians:
● Acknowledge the father’s emotional entry point. Teo emphasized that many dads are the first to see or touch their newborn in the NICU—an emotionally complex moment that while can be filled with joy in finally seeing their baby, for many dads it is accompanied by feelings of guilt that their partner may not be with them and sadness that the pregnancy ended prematurely. Recognize the complexity of that moment.
● Be realistic—but human. Honest, grounded communication helps parents stay mentally prepared.
● Include fathers in real-time updates. A brief call can make a meaningful difference.
● Affirm their efforts. Let dads know their presence matters and is beneficial for their baby.
● Many dads are grateful to be prescribed roles and responsibilities, such as helping moms by cleaning and preparing the pump supplies or delivering the expressed colostrum when ready.
● Ask how they process information. Tailor the level of detail to each father’s preferences.
For Nurses:
● Encourage hands-on participation. Reassure fathers that their gentle touch and care are meaningful.
● Help build confidence. Demonstrate caregiving techniques to ease fear.
● Create personal mementos. Milestone cards or NICU photos tailored for dads can strengthen bonding.
● Use humor and connection. Lightness can break tension and invite deeper engagement.
● Consider QI projects and initiatives that support bedside staff in working with fathers.
Final Reflection: As Adam Wood shared, “This baby is our world and we are entrusting you with helping not only our baby—but us—make it out. Show us that you care. Build trust. Let us advocate for our baby with your support.”
Implications for Clinical Practice
Fathers are not secondary parents—they are essential pillars of the NICU family. As clinicians, we must:
– Normalize emotional check-ins for dads, not just moms – Provide anticipatory guidance tailored to
fathers
– Offer dedicated peer support pathways
– Acknowledge and affirm their identity as caregivers
When we reframe NICU care to include the whole family unit, outcomes improve not just for infants but for every caregiver who walks through the NICU doors. These changes do not require significant resources—just intentionality. The impact on family connection, parental confidence, and outcomes can be profound.
Conclusion: “Celebrate the ounces gained,” Adam said. “Celebrate every milestone. Because if you don’t, it’s easy to get lost in everything else.” These fathers have shown us what presence means. Their voices challenge us to rethink how we engage, educate, and empower every member of the NICU family. Fathers are not extra. Fathers are not optional. Fathers are critical—and they deserve to be seen that way. As NICUs strive to become more inclusive and equitable, elevating the father’s voice is not only overdue—it is essential. To hear these fathers’ stories in their own words, you can view the recorded here:https://us02web.zoom.us/webinar/register/WN_HYS5KcDDTFK9GV_7Z7HkYw.



Cyprus’ President, Nicos Anastasiades, has bestowed the Grand Cross of the Order of Makarios lll on Paphos-born Dr Kypros Nicolaides, a world-renowned pioneer in fetal medicine, in recognition of his invaluable contribution to science and society more generally.
At a ceremony at the presidential palace, Anastasiades paid tribute to the London-based doctor whose discoveries have revolutionised the field and earned him the title the ‘Miracle Maker.’
Anastasiades noted that Cyprus’ highest honour is normally awarded to heads of government, and only in exceptional cases to distinguished personalities.
“As President of the Republic of Cyprus, taking into consideration the invaluable contribution of Professor Kypros Nicolaides in promoting health, and particularly the field of fetal medicine, I decided that the only worthy honour to this world known scientist was to award the Grand Cross of the Order of Makarios lll,” the President said.
As a doctor, Nicolaides has dedicated his life to fetal health, developing pioneering research and clinical programmes for prenatal diagnosis and treatments and inextricably linking his name to numerous breakthroughs in diagnostics, including of Down Syndrome.
Through his work in medical schools and scientific publications he has helped advance prenatal medicine and opened up the horizons to the revolutionary sector of fetal surgery, the President said.
Nicolaides has helped promote accessibility to these breakthroughs with the establishment of the non-profit Fetal Medicine Foundation in 1995 which has invested millions in research and training, and offered scholarships to doctors worldwide, among other.
Cyprus has also benefitted from the doctor’s expertise and generosity, the President said. The Fetal Medicine Centre has worked closely with the Makarios Hospital’s gynecological department to deal with high-risk pregnancies, while Nicolaides donated cutting edge ultrasound equipment to the hospital. In recognition of the professor’s contribution, a maternity ward at the hospital was named after him.
Indicative of the world recognition Nicolaides enjoys was his recent election to the US national academy of medicine – one of only 10 clinical doctors who are not US citizens, Anastasiades said.
Pioneer of fetal medicine, Dr Kypros Nicolaides, has been awarded Cyprus’ highest honour.
Accepting the award, Nicolaides said he saw it as a tribute to the love and support to the doctors worldwide who have dedicated their lives to the service of women and their newborns.
“To those who will not compromise with the tragic reality that every minute a woman somewhere in the world dies as a result of a complication in her pregnancy or at childbirth and that the large majority of these can be avoided. To the doctors who dedicated their lives to reducing peri-natal mortality, forecasting and preventing premature births, congenital anomalies, placental insufficiency, and other,” he said.

For over 50 years there has been a commitment to multilateralism and funding for science and health. Recent shifts around the world jeopardise the ability of all countries to address existing and new health crises, and specifically threaten hard-won progress in reproductive, maternal, newborn, and child health, including for preterm babies who are particularly vulnerable.
Preterm birth remains a silent emergency of a global scale. Every 2 seconds, a baby is born too soon. Every 40 seconds, one of those babies dies. An estimated 13.4 million babies were born preterm (before 37 weeks of pregnancy) in 2020 – equivalent to nearly one in ten babies being born preterm worldwide.
Preterm birth is the leading cause of child deaths, accounting for more than 1 in 5 of all deaths of children occurring before their 5th birthday. From 2010 to 2020, an estimated 152 million babies were born preterm. Yet, rates of preterm birth have remained stagnant, with some regions even witnessing an increase. For preterm survivors, challenges extend far beyond the neonatal period, as they face a higher risk of lifelong health complications, including developmental delays, disabilities, and chronic conditions . Limited advancements in the prevention of preterm births and gaps in the implementation of the care of preterm newborns have contributed to the global slowdown in progress for reducing newborn and child mortality since the adoption of the Sustainable Development Goals (SDGs) in 2015. Hence, progress remains insufficient to achieve the necessary reductions in newborn and child mortality to meet the SDG targets by 2030. In response, the 77th World Health Assembly Resolution on accelerating progress for maternal, newborn, and child health included a strong call for intensified global action to address the root causes and effects of preterm birth.
To fast-track evidence-based implementation on the prevention of preterm birth and care for preterm babies, this supplement expands content from the 2023 report “Born too soon: decade of action on preterm birth” . We are also building on the first Born Too Soon report in 2012 , which presented the first ever national and global preterm birth estimates, and the linked BMC Reproductive Health supplement (2013), which translated the chapters into academic articles. We have emulated this approach with a supplement in the same journal. The papers in this supplement expand on the chapters in the 2023 edition of Born Too Soon. Each paper presents evidence synthesis based on literature reviews, country case studies about good practices on policy and implementation and lived experiences and community perspectives.
This 2025 supplement anchors preterm birth as a key issue within the continuum of maternal and newborn care, including the prevention of stillbirth. The supplement highlights the importance of women’s sexual and reproductive health and rights (SRHR). It places additional emphasis on adolescent girls, who have an increased risk of preterm birth but often have far less access to the services and care that they need to support their health and well-being. Importantly, a life-course perspective is foundational and recognises the intergenerational impacts of preterm birth. Hence, we place additional emphasis on the follow-up care and support that is needed for survivors of preterm birth and their families.
The 2023 Born Too Soon report was part of a campaign to elevate awareness around the burden, solutions and priorities for preterm birth. This movement for action was spearheaded by the Partnership for Maternal, Newborn and Child Health (PMNCH), the world’s largest alliance for women’s, children’s and adolescents’ health and wellbeing, and harnessed three shifts: power of data, people’s stories and partnerships.
Priorities to catalyse change/Power of data and new evidence
The 2010 estimates on preterm birth showed that preterm birth affected every country, including high-income ones, with the USA in the top ten for numbers of babies born too soon. Evidence-based action could save over a million children who die needlessly each year. Equity gaps are enormous, with only 1 in 10 extremely preterm babies (< 28 weeks) surviving in low-income countries, compared to more than 9 in 10 in high-income countries . These inequities in survival are driven by a lack of access to quality care and determine the likelihood of preterm birth, death, and disability. Disparities, however, do persist in high-income countries, where marginalised groups face significant challenges in accessing timely and effective care. Poverty often limits access to essential services such as prenatal care, proper nutrition, and safe living conditions, which are critical for preventing preterm births and managing complications. Systemic racism further exacerbates these issues, with minority groups frequently encountering bias, lower-quality care, and obstacles in navigating healthcare systems, resulting in poorer outcomes for both mothers and babies .
Yet, investment in preterm birth prevention and care can unlock more human capital than at any other time across the life course, impacting futures for millions of families and resulting in significant human and economic returns.
Power of people at the centre
These data and large numbers reflect affected individuals and communities – women, babies and their families and healthcare workers – which PMNCH put at the heart of the campaign. An essential dimension of the Born Too Soon movement was a collection of narratives from affected families and other lived experiences, including healthcare workers [13]. Parent and patient groups along with healthcare professional associations have led the charge for preterm birth; in this supplement, we argue for a broad and multi-constituency mobilisation around this agenda, to improve investments in preterm birth across sectors.
Power of partnerships
The 2023 Born Too Soon report , and this supplement were fuelled by engagement of 70 organisations, including 140 individuals from 46 countries. The campaign reached 215 media products across six continents, for a total estimated media reach of 3.47 billion people. With a diverse authorship explicitly including leaders from low- and middle-income countries (LMICs) and young experts, the papers in this supplement position the prevention and care for preterm babies as a cornerstone of integrated and high-quality maternal and newborn care, including stillbirth prevention. The 2023 Born Too Soon report was co-published by PMNCH, WHO, UNICEF and UNFPA, and guided by a high-level Advisory Group. In addition, this supplement has been published as part of the 2025–2026 joint WHO and PMNCH advocacy campaign, linked to the 2025 World Health Day theme: “Healthy Beginnings, Hopeful Futures”, calling for unified action and urgent prioritisation of maternal and newborn health.
Papers in this supplement
This supplement, Born Too Soon: Progress, Priorities, and Pivots for Preterm Birth, expands on the content of the Born Too Soon 2023 report, adopting a life-course approach that follows women and their newborns over time within a continuum of care. The supplement consists of seven analysis papers and four commentaries.
We present updated data and evidence from the 2012 report , now examined through a broader lens, including new data on preterm birth rates, trends, risk factors, and advances in measurement globally; maternal health and care relevant to preterm prevention, with an emphasis on sexual and reproductive health and rights; care for small and sick newborns; and implementation learning for systems change, extending beyond preterm care alone. Within each paper, content was organised by three domains:
- 1. progress, particularly in the last decade, related to preterm birth;
- 2. programmatic priorities based on up-to-date and policy-relevant evidence; and
- 3. pivots needed to accelerate change in the decade ahead
Five papers in this supplement align to the 2012 set including:
- Paper 1: Learning from the past to accelerate action in the next decade.
- Paper 2: Global epidemiology of preterm birth and drivers for change .
- Paper 3: Progress and priorities for respectful and rights-based preterm birth care.
- Paper 4: Women’s health and maternal care services, seizing missed opportunities to prevent and manage preterm birth..
- Paper 5: Care for small and sick newborns, evidence for investment and implementation.
- Paper 6: Integration of intersectoral interventions for impact on preterm birth.
- Paper 7: Accelerating change to 2030 and beyond.
- Two new papers cover novel topics of increasing importance with new evidence that were not included in the 2012 Born Too Soon report:
Overall, these supplement papers emphasise a healthy beginning for vulnerable babies, and the life course approach underlining the follow-up care and support needed for survivors of preterm birth and their families over the course of their lives. The first paper reviews progress during the last decade since the last report, primarily from a policy perspective, and considers the challenges that have hindered advancements and looks ahead, positioning preterm birth as a pivotal issue for driving more rapid and integrated progress for women and children.
The second paper presents updated national estimates of preterm birth rates for 195 countries, with trends for the last decade emphasising the flatlining of progress for preterm birth rates in every region, with new insights on risk factors. There are positive improvements in measurement and opportunities to more accurately count and account for preterm births and use these data to drive action.
The third paper focuses on rights and respect for women and their babies, calling for a rights-based approach to respectful care for the mother-baby dyad, especially small and preterm babies who are the most vulnerable. This paper also promotes an enabling environment for healthcare workers with supportive policies and accountability mechanisms .
The fourth paper focuses on women’s health and maternity services, highlighting the evidence and the importance of seizing missed opportunities in preventing and managing preterm birth within existing care packages. A broader emphasis on sexual and reproductive health and rights is also championed.
The fifth paper highlights the opportunity for impact and high return on investment with small and sick newborn care, and sets out interventions and innovations for faster implementation with health systems shifts to ensure newborns survive and also thrive and families are at the centre of care. Crucial gaps for infrastructure, devices, data and especially workforce are highlighted.
The sixth paper focuses on intersectoral interventions to improve preterm birth and highlights the need for an intersectoral approach that addresses the multifaceted challenges of prevention and care for preterm birth, focusing on equity and rights, education, economy, environment (including nutrition and climate) and emergencies (“the five Es”)
The seventh and final paper outlines a forward-looking call to action, highlighting investment, implementation in partnership with women and families, integration, and innovation to drive progress.
Three additional commentaries are also included in the supplement: the first is a high-level political commentary by prominent signatories, including three heads of agencies and the PMNCH Board chair, the second focuses on community voices; and the third highlights data and findings on preterm births from recent work led by Countdown to 2030 and partners, placing preterm birth within the context of the maternal-newborn-stillbirth transition framework and the Every Woman Every Newborn Everywhere coverage targets.
Progress is possible
The Born Too Soon movement, the report and these papers, take stock of the journey of the past decade – the good and the bad, the challenges and the opportunities to accelerate preterm birth prevention and improved neonatal care into the next decade. Born Too Soon shines a spotlight on countries’ achievements and innovations that can inspire and inform faster progress. The agenda for preterm birth is central to the SDGs, recognising that progress on maternal and newborn health and stillbirths depends on collaboration across sectors. Highlighting where progress is happening, this supplement looks to the future to reduce the burden of preterm birth by investing more in high-quality, respectful care for women and babies so that they can survive and thrive, in every country, in the decade to come.


PREEMIE FAMILY PARTNERS

June is National Safety Month, and it’s the perfect time to share a few key tips to help keep babies safe while they sleep. At First Candle, we know how overwhelming all the advice can be, so we’re keeping it simple: safe sleep saves lives.
Each year, thousands of babies die from Sudden Unexpected Infant Death (SUID), which includes SIDS and Accidental Suffocation. The truth is, most of these deaths involve more than one unsafe sleep practice—and nearly 60% happen when a baby is sharing a sleep surface with someone else.
Here’s what you really need to know:
- Back is Best: Always place baby on their back to sleep, on a firm, flat surface with a tight-fitting sheet. If the surface is too soft (like a couch or adult mattress), it can increase the risk of suffocation.
- Clear the Crib: Keep baby’s sleep space totally empty—no pillows, bumpers, stuffed animals, or blankets. (Yes, even a soft little blanket can be deadly.) Use a wearable blanket instead if you’re worried about warmth.
- Watch the Products: Swings, rockers, loungers, and other inclined gear might be great for awake time, but they’re not safe for sleep. If baby nods off, move them to a crib, bassinet, or play yard right away.
- If You’re Tired, Put Baby Down: We know how comforting it is to cuddle your little one, but if you’re feeling sleepy—even just for a second—lay baby down in a safe space. Babies can suffocate in a parent’s arms if the parent falls asleep. Don’t take the risk.
We’re here to help make safe sleep simple. These small changes can make a huge difference—and give you peace of mind while your baby rests.
Let’s spread the word this National Safety Month and protect every little life we can.
This educational video introduces the importance of preventing Central Line-Associated Bloodstream Infections (CLABSIs) as part of a broader effort to reduce hospital-acquired conditions and support children’s recovery. The video explains that a central line is a special tube placed in a large vein near the heart to aid in treatments, and while helpful, it carries a risk of infection if not properly managed. To help prevent CLABSIs, parents and caregivers are encouraged to: — Talk daily to the healthcare team about the need for the central line. — Wash hands thoroughly before touching the line or the area around it. — Help with daily cleaning using Chlorohexidine Gluconate (CHG) wipes if the child is over 2 months old. — Check that the dressing is clean, dry, and secure. — Change bed sheets daily to reduce infection risk. The video emphasizes that parents play a critical role in infection prevention and encourages them to continue watching the series.


Key Points
Having a baby in the NICU can be stressful for families. Expect to have many different feelings about your baby’s health and care.
You, your partner, and your family may cope with the stress of the NICU differently. It’s OK to have different feelings.
It’s important to take care of yourself so that you can care for your baby.
You may feel sad and worried during your baby’s NICU stay. If you think you have a more serious condition, like depression or anxiety, talk with your healthcare provider or NICU team right away.
What emotions could you have when your baby is in the neonatal intensive care unit (NICU)?
Many parents feel very alone during their baby’s NICU stay. The stress of having a baby in the NICU can go on for weeks and months. It can be tiring to learn so much about your baby’s medical condition and make care and treatment decisions. No parent is fully prepared for life in the NICU. But parents can find ways to get comfortable there.
You may have many different feelings, including guilt, helplessness, sadness, anger, fear, shock, and a sense of loss when your baby’s in the NICU. There is no “normal” way to feel. You and your partner may cope differently. Know that your feelings are shared by many families who have had a baby born early, with birth defects, or other medical conditions. Over time, you will be able to better face and cope with your feelings.
There are a lot of ways to get support. Letting other people know how you’re feeling may help you on your journey through the NICU. Your partner, friends, family, and hospital staff can play a big role in how you cope.
How can you take care of yourself when your baby is in the NICU?
It’s hard for parents to leave their baby in the NICU. It may be even harder to think about taking care of yourself, because you’re so focused on your baby’s needs. But doing so means that you can stay well and have more energy to spend time with your baby.
One way to take care of yourself is to have a daily routine. This means eating meals, drinking plenty of water, taking showers, and getting regular sleep while your baby’s in the NICU. If you’re having trouble doing these things, talk to your healthcare provider, the NICU social worker, or your baby’s nurse. As part of your routine, decide when you want to be with your baby in the NICU. Share these times with your baby’s nurse so they know when to expect you.
Another way to take care of yourself is to connect with NICU families. If your baby is in a single room, look for families at NICU classes or in the family lounge. If your baby is in a room with many babies, take time to get to know the other families. They may understand your experience better than other people in your life.
It’s also helpful to find healthy ways to take breaks from the NICU. This can include going outside, getting lunch with a friend, or taking a nap at home. It’s OK to make time for yourself and your family at the hospital and at home.
What can you do if you need to go back to work when your baby’s in the NICU?
If you need to go back to work while your baby is still in the NICU, it may be helpful to talk with NICU staff. Let them know your work schedule and when you plan to be with your baby. You also may want to discuss your work schedule with your employer. Ask if you can get time off from work while your baby is in the NICU. Or see if you can work different hours so you can be with your baby when it’s best for them. Know that you’re doing the best that you can and try not to be too hard on yourself.
What if you feel sad and worried when your baby’s in the NICU?
Having a baby in the NICU can be an emotional time for parents. You may feel sad and worried. Lots of NICU parents feel this way during their child’s NICU stay or even once they’ve come home. Sometimes you or your partner may have more serious conditions, like depression and anxiety. These conditions can be brought on by the NICU stay but also your body’s reaction to your baby being born. Having depression or anxiety can make it hard for you to take care of your baby.
Baby blues are feelings of sadness a mom may have in the first few days after having a baby. Baby blues are also called postpartum blues. Postpartum means after giving birth. Baby blues can happen 2 to 3 days after you have your baby and can last up to 2 weeks. They usually go away on their own, and you don’t need any treatment. If you have sad feelings that last longer than 2 weeks, tell your healthcare provider. They may want to check you for a condition called postpartum depression.
Postpartum depression (PPD) is a kind of depression that some people get after a baby is born. PPD is strong feelings of sadness, anxiety, and tiredness that last for a long time. These feelings can make it hard for a parent to take care of their baby. This depression can happen during pregnancy or in the first year after a baby is born. PPD is more common in people who have or have had a baby in the NICU. It often starts within 1 to 3 weeks of having a baby. It’s a medical condition that needs treatment to get better.
If you think you may have PPD, call your healthcare provider or talk with your NICU team right away. There are things you and your provider can do to help you feel better. If you’re worried about hurting yourself or your baby, call 911.
Last reviewed: April 2025 –https://www.marchofdimes.org/find-support/topics/neonatal-intensive-care-unit-nicu/coping-stress-nicu
HEALTHCARE PARTNERS

Highlights:
– NICU-specific CLABSI bundle reduced infection rates by over 80%.
– Central line days and total healthcare costs decreased significantly.
– Preterm-specific modifications improved bundle safety and feasibility.
– Multidisciplinary approach enhanced bundle adherence and sustainability.
Abstract:
Background
Central Line-Associated Bloodstream Infections (CLABSIs) in Neonatal Intensive Care Units (NICUs) significantly impact patient outcomes and healthcare costs. This study evaluates the effect of NICU-specific bundle designed to prevent CLABSIs.
Method
This retrospective single-center study was conducted at Hacettepe University Faculty of Medicine from March 2020 to August 2021. It was designed to compare 2 periods: pre-intervention and post-intervention period.
Result
The implementation of the bundles led to a significant reduction in infection rates, with CLABSIs decreasing from 29 to 4 per 1000 central line days in NICU-1 and from 14.2 to 2.6 per 1000 central line days in NICU-2. This decline was accompanied by an 80% reduction in the average healthcare cost per patient.
Conclusion
The implementation of a NICU-specific CLABSI prevention bundle significantly reduced infection rates and lowered healthcare costs by approximately 80% per patient. These findings highlight the effectiveness of structured, multidisciplinary infection control strategies in improving neonatal outcomes and resource utilization.
Source: https://www.ajicjournal.org/article/S0196-6553(25)00427-4/abstract



Building Trust and Transparency in Trauma-Informed Developmental Care: A Foundation for Healing
In trauma-informed developmental care (TIDC), trust and transparency are foundational principles that nurture the connection between caregivers, families, and infants. These values are essential in creating an environment where healing can truly thrive. Within the NICU, every action, communication, and decision shapes the experience of both families and clinicians, making trust and transparency vital elements for fostering a safe and supportive space.
Why Trust and Transparency Matter in TIDC
For families in the NICU, trust is more than just a comfort; it is a lifeline. The NICU can be an overwhelming place, where uncertainty often looms and the ability to make sense of complex medical information is a challenge. When caregivers lead with openness and integrity, they provide families with a sense of stability and assurance, letting them know that they are not alone in this journey.
Transparency is equally important—it bridges the gap between clinical decisions and family understanding. Through honest and clear communication, transparency ensures that families are not left in the dark. They become active participants in their baby’s care, making informed decisions that honor both their role and their connection to their child. This empowers families and builds a collaborative, respectful partnership between clinicians and parents.
Building Trust Through Consistent Communication
In TIDC, building trust requires more than a single moment of reassurance. It is an ongoing commitment to consistent, open communication. Caregivers can foster trust by:
- Being present and available: Spending time with families, answering questions, and genuinely listening to their concerns builds a foundation of trust that extends through every interaction.
- Providing information proactively: Rather than waiting for questions, sharing updates and explaining procedures in a way that’s accessible and respectful shows families that you value their involvement.
- Honoring family perspectives: Listening to families’ insights about their baby and their own needs fosters a partnership that acknowledges their expertise and deep connection to their child.
Each of these actions reinforces that caregivers are allies on this journey, deeply invested in the well-being of the family and their baby.
Practicing Transparency with Compassion
Transparency in TIDC goes beyond simply sharing information—it involves delivering it in a way that is compassionate and supportive. Here are some key aspects of practicing transparency in a trauma-informed way:
- Clarity in communication: Avoiding jargon and speaking in clear, accessible language ensures families can understand and feel comfortable asking questions.
- Honesty about challenges and limitations: Being forthright about the uncertainties or potential complications in care allows families to feel genuinely informed and respected, rather than shielded from difficult truths.
- Inviting collaboration: Transparency means involving families in care discussions and decisions as much as possible, allowing them to be active participants rather than passive recipients of care.
By integrating compassion into transparent communication, caregivers build trust while respecting the vulnerability and emotional experience of families in the NICU.
The Ripple Effect of Trust and Transparency in the NICU
When trust and transparency are at the heart of trauma-informed care, the effects are far-reaching. Families feel valued and empowered, creating a foundation of resilience that will benefit them and their child beyond the NICU. Babies, too, benefit from this foundation, as families who feel confident and supported are better equipped to provide the emotional nurturing and bonding that are essential for healthy development.
Moreover, trust and transparency extend to the clinicians themselves. When caregivers practice these principles, they create an environment of respect and honesty that fosters teamwork and mutual support. This culture of openness reduces stress, enhances job satisfaction, and helps create a more compassionate and connected caregiving community.
Trust and Transparency: Essential Pillars of Trauma-Informed Care
In trauma-informed developmental care, trust and transparency are not just principles; they are acts of love and respect that resonate deeply within the caregiving environment. By leading with these values, we create a NICU space where families and clinicians feel valued, connected, and empowered to provide the best possible care.
At Caring Essentials, we believe that trust and transparency are essential pillars of trauma-informed care, supporting every interaction, every decision, and every relationship within the NICU. By honoring these principles, we are building a future where families and clinicians alike can find strength, healing, and hope—together. With unwavering commitment to fostering trust, Mary Coughlin.

INNOVATIONS

Clinical innovations in neonatology have historically faced roadblocks. Among other reasons, designing and executing studies that test safety and efficacy in a vulnerable patient population is a challenging pursuit. Neonatologists at Cleveland Clinic Children’s aim to overcome barriers within the field by engaging colleagues in a dialogue about innovations on the horizon in neonatal care.
Innovation was the theme of the recent Symposium on Health Innovation and Neonatal Excellence (SHINE). The meeting, hosted in Orlando, included a variety of speakers and sessions and one element that introduced a new twist—a competition.
Following an international call for submissions of noncommercialized innovations, the symposium directors received 36 proposals from centers around the world. Submissions underwent a peer-review process by a scientific committee—a panel of distinguished neonatologists—and were evaluated based on originality and potential impact within the field.
Read on for a recap of the top seven projects underway, listed below in no particular order.
A new screening paradigm for retinopathy of prematurity
The current approach to screening for retinopathy of prematurity (ROP), the leading cause of childhood blindness, is both technically challenging for providers and physiologically stressful for neonates, and most will never require ophthalmic intervention. Researchers have developed two new camera technologies that combine ultra-widefield imaging and AI: one is a low-cost 2D camera, and the other is a 3D optical coherence tomography device. These technologies examine patients’ retinas without the need for dilation, bright white light, scleral depression — or an ophthalmologist. The screening is completed in less than 10 seconds and provides immediate results. These innovations are poised to reimagine ROP screening by providing an objective evaluation, enhancing the patient experience and offering lower-cost technology for families and providers. Presenting author: J. Peter Campbell, MD, Oregon Health & Science University
Converting bCPAP sounds into clinical insights
The bubble continuous positive airway pressure (bCPAP), a mainstay in neonatal care, has considerable limitations, including a circuit system prone to obstruction and leaks. Nurses and respiratory therapists must conduct frequent manual checks to resolve the issue. Currently, providers rely on bCPAP sounds to affirm the device is working properly. The project proposes to leverage acoustic sounds by converting them into electronic signals to help quantify pressure, oscillations and leaks. This could provide real-time insights into CPAP therapy, informing and optimizing the management of neonates. Presenting author: Wissam Shalish, MD, PhD, Montreal Children’s Hospital, McGill University
Deep learning that combines video with vital signs
This innovation uses a deep learning algorithm trained on video and physiological data to detect and quantify events in the NICU. The project addresses a need within neonatal care for accurate and continuous monitoring of infant stressors, which are currently captured manually with the Neonatal Infant Stressor Scale. The trained model can accurately estimate short-term physiological responses and identify activities that induce significant stress responses. Researchers are hopeful that the technology can facilitate earlier detection of adverse events and support appropriate interventions to improve outcomes. Presenting author: Ryan M. McAdams, MD, University of Wisconsin-Madison
Reimagining the CPAP nasal interface
Continuous positive airway pressure (CPAP) is a noninvasive and effective alternative to nasal cannula therapy for infants and neonates experiencing respiratory distress. However, the nasal interface consists of multiple pieces that can make assembly burdensome and dislodgment of the interface a common occurrence. This project aims to reimagine the device by developing a single-piece nasal CPAP interface that integrates multiple components into a secure, ergonomic and scalable product. The device could lead to improved use and adoption, offering a low-cost, high-impact option for a broader patient population. Presenting author: Mohamed Mohamed, MD, Cleveland Clinic Children’s
Earlier detection of opioid withdrawal symptoms
Conventional approaches to assessing opioid withdrawal in infants rely on subjective clinical observation of symptoms. A new algorithm-based technology, the physiologic opioid withdrawal score (POWS) system, offers an objective, real-time monitoring option. It’s trained on retrospective data of infants with neonatal opioid withdrawal syndrome (NOWS) and, taken together with physiologic data, the proposed tool—a portable, hospital-grade device— aims to continuously monitor vital signs to improve treatment timing and reduce variability. Presenting author: Zachary Vesoulis, MD, Washington University
Optimizing NIRS sensor placement to detect necrotizing enterocolitis
Necrotizing enterocolitis (NEC) is one of the leading causes of death in preterm infants. Early detection and intervention of malperfusion can mitigate fulminant NEC. Near-infrared spectroscopy (NIRS) is the gold standard for measuring intestinal perfusion; however, it is imprecise, as it also includes cerebral NIRS for abdominal applications. Researchers have developed a novel computational model to enhance existing technology by utilizing an algorithm that predicts the NIRS fluence rate signal in the neonate’s abdomen. This approach could significantly improve early detection and offer a cost-effective, scalable solution for reducing neonatal mortality. Presenting author: Vishnu S. Emani, BS, Harvard University
Feeding tube capable of vital sign monitoring
Trinity Tube is a multifunctional, sterile, single-use nasogastric feeding tube. It integrates enteral feeding with vital sign monitoring, including ECG, temperature and continuous airway pressure assessment. Designed specifically for neonatal care, it eliminates the need for skin-mounted sensors, thereby reducing the risk of skin injury and infection. It also contains a pressor sensor that supports continuous non-invasive assessment of airway pressure and allows teams to transition infants to “pressure targeted high flow therapy,” a novel approach that combines high-flow nasal cannula with the effectiveness of CPAP. The device aims to simplify care, improve the patient experience and reduce the nursing burden in NICUs.
Source: 7 Emerging Innovations in Neonatology

Despite a 44% reduction in neonatal mortality since 2020, 65 countries still risk missing the Sustainable Development Goal to reach a neonatal mortality rate of 12 per 1000 livebirths or less by 2030, and approximately 2·3 million preterm and sick newborns die each year. Health care for neonates is extremely challenging. With recommendations to drive innovation, the Lancet Child & Adolescent Health Commission on the future of neonatology presents an ambition for equitable, innovative, research-driven neonatal medicine that will both close treatment gaps and seize more opportunities within the neonatal period to reduce mortality and shift the health trajectory of every newborn towards lifelong wellbeing.
Uncertainty lingers across many fundamental aspects of neonatal medicine, and the Commission analyses the delays and disruptions in research and development that hinder innovation. Just a few neonatal conditions—acute respiratory failure, bronchopulmonary dysplasia, hypoxic-ischaemic encephalopathy, congenital malformations, necrotising enterocolitis, and severe infections—account for 76% of neonatal deaths. Yet none of these conditions are understood well enough, pathophysiologically, to develop preventive measures and effective therapies. Much practice in neonatal critical care, including management of septic shock and multisystem organ failure, are informed by adult critical care. Similarly, common treatments—including essential medicines such as sedatives and analgesics for pain management—have, by necessity, been adopted from other areas of medicine to address unmet needs for neonates. The Commission argues for stronger financial and regulatory support to ensure such treatments are specifically designed for and tested in neonates, enabling tailored treatments and a high quality of evidence.
The Commission identifies medicines and medical devices that could strengthen clinical practice. It also outlines how the neonatal research ecosystem is shaped by stakeholders of neonatal health: institutional review boards, ethics committees, and regulatory agencies; industry; physicians and allied health-care professionals; former patients, family representatives, and advocacy groups; and governments, universities, and academic medical centres. Each are offered recommendations to address challenges with knowledge gaps, funding, and regulatory and commercial obstacles to development.
For the 68% of the world’s children who are born in resource-constrained settings, overcoming issues with cost, infrastructure, and human resources are immediate priorities to improve neonatal care. The Commission speaks to these logistical hurdles but challenges the assumption that blanket expansion of existing interventions is safe and productive. Antenatal steroid prophylaxis and therapeutic hypothermia are key examples of interventions that showed initial promise in clinical trials but proved far from universally safe across all settings. To realise the vision of equitable neonatal health, the Commission emphasises the importance of evidence-based neonatal medicine through research and development that is both accelerated and sustainable to benefit all neonates.
Accompanying Comments highlight three of the Commission’s main themes: the role of caregivers in improving neonatal research; special considerations for research and development in low-resource settings; and the value of collaboration and training. Arti Maria beckons leaders in neonatal wards to disrupt entrenched hierarchies and welcomes families as equal partners in neonatal research. Msandeni Chiume and colleagues call for collective ambition in implementation research across low-resource regions and point to Africa’s successes in securing national investments in sustainable neonatal health. Finally, Chris Gale and colleagues share insight on cultivating a strong research ethic, emphasising training for the entire neonatal care team—especially neonatal nurses—to contribute to research. Thought leadership across these diverse settings shows the immense opportunity for innovative partnerships in neonatology.
Neonatology has profound potential to influence population health across the lifespan. All stakeholders of neonatal health must contribute towards innovation, collaboration, and resources to realise this potential. Neonatologists are especially encouraged by the Commission to use their expertise in high-level decision making across academia, industry, government, and the charitable sector. As advocates for neonates’ health-care needs, they can ensure neonatal research and development reaches the top of population health agendas worldwide.
Source: https://www.thelancet.com/journals/lanchi/article/PIIS2352-4642(25)00189-0/fulltext



Womb Warriors: The Power of Small Kindnesses
To my fellow preemie survivors—August is often a month marked by both warmth and reflection. It’s a time when summer winds down, school gears up, and the world seems to shift gears quietly. This month, in honour of World Humanitarian Day, I want to remind us of something beautiful: we don’t need to be loud to be powerful. We don’t need to be big to make a difference. Sometimes, the smallest acts of kindness speak the loudest—especially for those of us who started out small but mighty.
I’ve always found a special kind of joy in watching children support each other in everyday ways. Whether it’s a classmate quietly cheering on a friend at soccer practice, or a child helping another with their backpack after school, these moments—simple and unassuming—have such weight. They remind me that the spirit of kindness is often most alive in the tiniest gestures. As someone who once fit in the palm of a hand, I’ve learned that small things can carry immeasurable strength.
This August, I encourage all of us—parents, survivors, and supporters—to take part in acts of kindness, however small they may seem. Share your crayons. Smile at a stranger. Send a note to a NICU nurse who once held your life in their hands. Compliment a friend on their effort, not just their achievement. These actions, rooted in compassion, build a softer yet stronger world—one we know from experience is worth manifesting.
Born a preemie, our vulnerability and strengths are exposed, and our relationship with communities is born. Born to soon, we are blessed with a deeper capacity for empathy, forged in our earliest days. Let’s carry that forward. Let’s choose kindness this month—not because the world is perfect, but because we understand how powerful it is when someone simply cares.
Because even now, long after the wires and monitors are gone, we are still warriors. And warriors don’t just survive—we lift others up along the way.
With strength, gratitude, and hope, Kat